Incidence of inflammatory bowel disease (IBD) is increasing progressively. Few recent epidemiological prospective studies are available in Spain. The Epicom study, a population-based inception cohort of unselected IBD patients developed within the European Crohn's and Colitis Organization, was started in 2010. Vigo is the only Spanish area participating.
ObjectiveTo describe the incidence of IBD in the Vigo area and the phenotypical characteristics at diagnosis and to compare them with previous data available in Spain.
Material and methodsEpidemiological, descriptive, prospective, and population-based study. All incident cases of IBD during 2010 and living in the Vigo area at diagnosis were included. The Copenhagen Diagnostic criteria were used to define cases. Background population at the start of the study was 579,632 inhabitants. Data were prospectively entered in the EpiCom database.
ResultsA total of 106 patients were included (57.5% men, median age 39.5 years). Of them 53 were diagnosed of as Crohn's disease (CD), 47 ulcerative colitis (UC) and six IBD unclassified (IBDU). The incidence rate per 100,000 per year for patients aged 15 years or older was 21.4 (10.8 for CD, 9.4 for UC, 1.2 IBDU). Including pediatric population incidence rates were 18.3 (10.3 CD, 8.7 UC, 1.2 IBDU). Median time since onset of symptoms until diagnosis was 2 months.
ConclusionsThe incidence rate of IBD in Vigo is the highest compared to former Spanish cohorts, especially in CD patients. Median time since onset of symptoms until diagnosis is relatively short.
La incidencia de la enfermedad inflamatoria intestinal (EII) va paulatinamente en aumento. En España escasean los estudios epidemiológicos prospectivos recientes. En 2010 se inició el estudio Epicom, un estudio demográfico de cohortes de inicio de pacientes con EII no seleccionados que se desarrolla en el marco de la Organización Europea de Enfermedad de Crohn y Colitis Ulcerosa. La de Vigo es la única zona española participante.
ObjetivoDescribir la incidencia de la EII en el área de Vigo y las características fenotípicas en el momento del diagnóstico y compararlas con los datos previos disponibles sobre España.
Material y métodosEstudio epidemiológico, descriptivo, prospectivo y demográfico. Se incluyeron todos los casos de EII incidentes durante el año 2010 en residentes de la zona de Vigo. Para definir los casos se emplearon los criterios diagnósticos de Copenhague. La población del entorno al inicio del estudio era de 579.632 habitantes. Los datos se incluyeron en la base de datos EpiCom de manera prospectiva.
ResultadosSe incluyó un total de 106 pacientes (57,5% varones, mediana de edad de 39,5años). De ellos, 53 fueron diagnosticados con enfermedad de Crohn (EC), 47 con colitis ulcerosa (CU) y 6 con EII no clasificado (EIINC). La tasa de incidencia anual por 100.000 para pacientes de 15años o más fue de 21,4 (10,8 para EC; 9,4 para CU; 1,2 para EIINC). Si se incluye la población pediátrica, la tasa de incidencia fue de 18,3 (10,3 para EC; 8,7 para CU; 1,2 para EIINC). La mediana de tiempo para la aparición de los síntomas hasta el diagnóstico fue de 2meses.
ConclusionesLa tasa de incidencia de la EII en Vigo es la más alta en comparación con antiguas cohortes españolas, sobre todo en el caso de los pacientes con EC. La mediana de tiempo para la aparición de los síntomas hasta el diagnóstico es relativamente breve.
Inflammatory bowel diseases (IBD), Crohn's disease (CD) and ulcerative colitis (UC) are chronic inflammatory diseases of the gastrointestinal tract of unknown etiology. High quality epidemiological studies of unselected patients are essential in order to assess the real burden of IBD. Incidence and prevalence are highly variable among different countries, with IBD being more common in industrialized than in non-industrialized countries. For adult patients, the incidence rates vary between 0.1–20.2 for CD and 0.5–31.5 per 100,000 person-years for UC.1,2 Traditionally, North America, Scandinavia and United Kingdom are considered the areas of highest incidence. In recent years, incidence is progressively increasing in all geographic settings,1,3,4 but there are studies that show a change in this trend, with stabilization or decrease in areas with previously high incidence.5,6 The reasons for this rising incidence are uncertain. An increase in disease awareness, improved access to healthcare and diagnostic procedures, or true changes in life-style and environmental factors as a consequence of the socio-economic transition from ‘developing’ to ‘developed’ in many countries could all account for some of the changes.7,8
Population-based inception cohorts, including incident (newly diagnosed) patients, offer the most valid picture when studying the occurrence and natural course of the disease. However, due to difficulties in executing and maintaining population-based cohorts, the capability of performing this type of study is limited in most countries.9
Spain is considered a low-incidence region compared with northern European countries,5 but few recent prospective studies are available and they show variable data in terms of incidence.10–17
The European Crohn's and Colitis Organization's (ECCO) Epidemiological Committee (EpiCom) study is a prospective, population-based cohort of unselected IBD patients diagnosed in 2010 within well described geographical areas, aiming to investigate if an east-west gradient exists across European countries and to identify environmental factors involved in these differences. The study was carried out in 31 centers from 22 European countries, covering a total background of 10.1 million people.2 In Spain, Vigo is the only area participating in the EpiCom study.
The aim of this study within the ECCO-EpiCom cohort was to describe the incidence of IBD in the Vigo area and the disease phenotype characteristics at diagnosis as well as to compare them with previous data available in Spain.
Material and methodsStudy centersThis is an epidemiological, descriptive, prospective, population-based study developed in the Vigo area. Vigo area is located in the South-West of Galicia, in the Atlantic coast, and includes 26 municipalities. Cases were collected from hospitals included in the public health system (Complexo Hospitalario Universitario de Vigo and Hospital POVISA). Patients who belonged to Vigo area and were diagnosed in private Hospitals (mainly Hospital POVISA, Hospital Fatima and Hospital Perpetuo Socorro) or private clinics were also included. Furthermore, to complete data collection, regular visits to other departments apart from Gastroenterology were performed (Surgery, Internal Medicine, Radiology and Codification).
Case definitionIncident cases diagnosed from 1st January to 31st December 2010 and living in the Vigo area for at least one year at the time of diagnosis were included. Diagnosis of CD and UC was based on the Copenhagen Diagnostic criteria.18,19 Cases in which not all criteria for CD or UC were fulfilled, but patients were in need of relevant IBD therapy were classified as IBD unclassified (IDBU). Patients younger than 15 years were included as pediatric patients. Disease phenotype classification by disease location and behavior for CD and disease extend for UC were made according to the Montreal classification.20
Data collection and external validationDemographic data (age at diagnosis, gender, smoking habit), disease type and phenotype characteristics (extend, location, and behavior), weight, height and time from onset of symptoms until diagnosis were collected.
Data were prospectively entered by authors in the EpiCom database (www.epicom-ecco.eu), a web-based epidemiological database, previously designed specifically for IBD and validated.20,21 In order to improve data quality several built-in control and validation tests were used and an audit of our registered information was carried out.
Statistical analysisBackground population at the start of the study was 579.632 inhabitants. The incidence rate (number of new cases/100,000 inhabitants) was calculated. Age-standardized annual incidence rates were obtained using the European Standard population using 10-year age groups (from 15 to 65 years), and including also a pediatric specific group and a >65 years old group. The qualitative variables are expressed as number (n) and percentage. The quantitative variables are expressed as the mean and range. Median time from onset of symptoms and diagnosis is expressed in months. The Square-chi test was used to compare qualitative variables, and quantitative variables were compared using the Student's T test. Differences were considered to be statistically significant if p<0.05. Statistical analyses were performed with the SPSS software version 15.0 (SPSS Inc., Chicago, IL, United States).
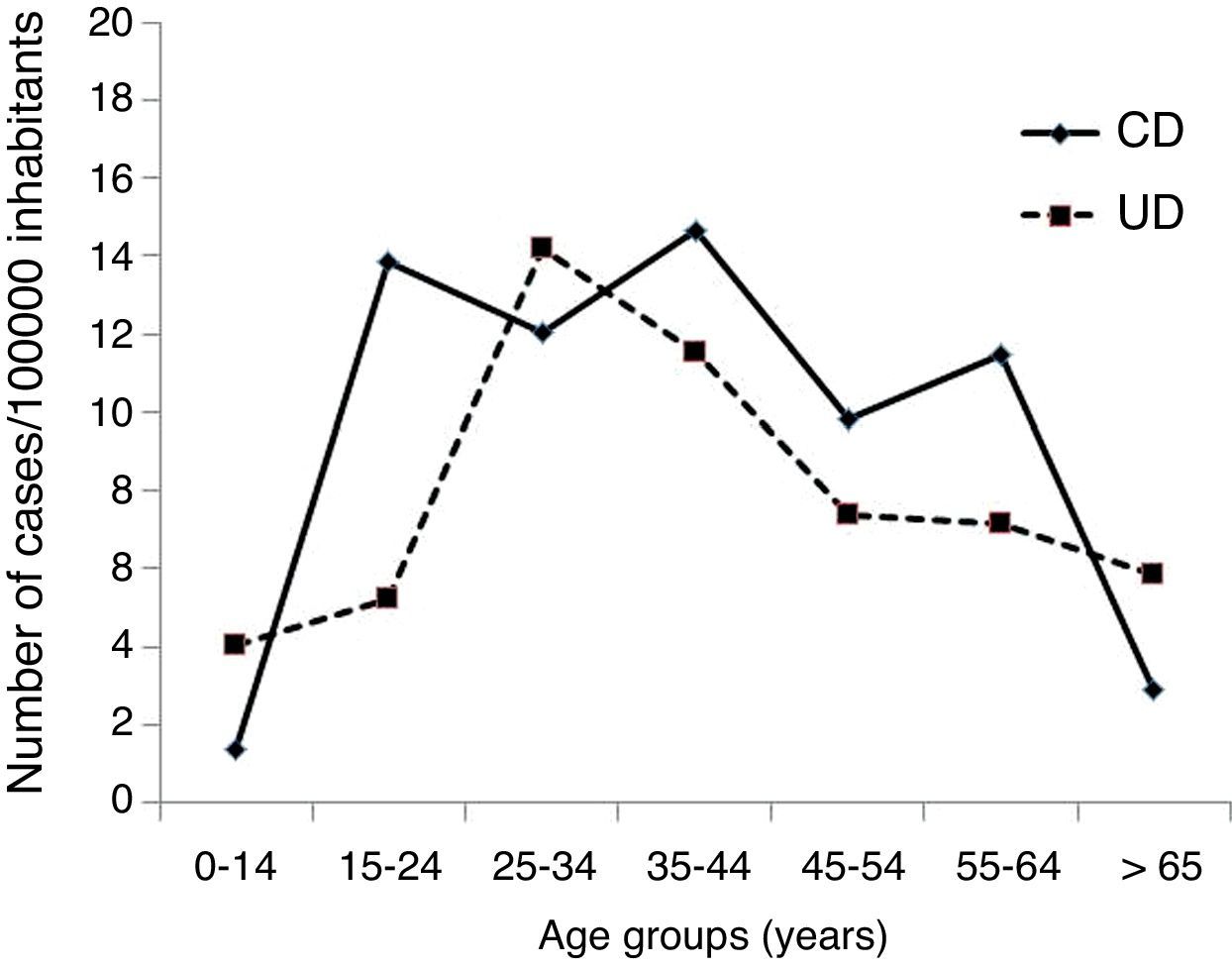
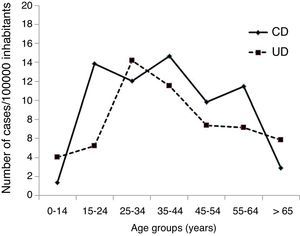
ResultsIncidence and disease phenotype characteristics of the Vigo 2010 cohortDuring the study period, 106 patients were diagnosed of IBD (102 aged 15 years or older, four pediatric patients). Of them, 53 (50%) were diagnosed with CD, 47 (44.3%) with UC and 6 (5.7%) IBDU. The incident rate (per 100,000 per year) for patients aged 15 years or older was 21.4 (10.8 for CD, 9.4 for UC and 1.2 for IBDU). Including pediatric population, incidence was reduced to 18.3 (10.3 CD, 8.7 UC and 1.1 IBDU). Age-standardized incidence rates are shown in Fig. 1.
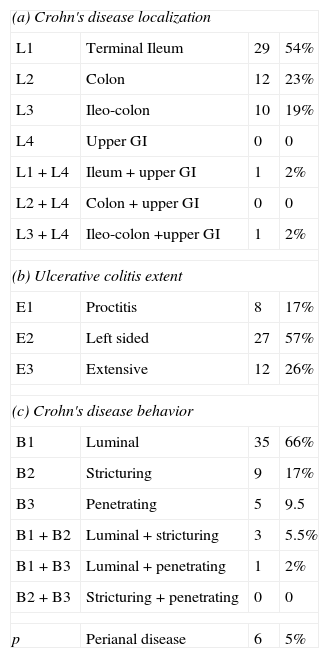
With respect to gender, 61 (57.5%) were men. Median age at diagnosis was 39.5 years (range 5–80). Specifically, median age in CD patients was 38 years (5–78) and in UC patients it was 41 (9–80). Disease phenotype characteristics at diagnosis (extend for UC, location and behaviors for CD) are summarized in Table 1. In relation with CD, 54% of patients presented ileal location at diagnosis, 19% ileocolonic and 23% colon only, stricturing behavior at diagnosis was identified in 22% of the cases and penetrating disease in 11%. Extensive presentation of UC was seen in 26% of patients. Six patients (5%) suffered from perianal disease at diagnosis, and 10 (9%) patients presented extraintestinal manifestations (8 joint diseases, 2 ophthalmological disorders).
Disease localization and behavior at diagnosis.
| (a) Crohn's disease localization | |||
| L1 | Terminal Ileum | 29 | 54% |
| L2 | Colon | 12 | 23% |
| L3 | Ileo-colon | 10 | 19% |
| L4 | Upper GI | 0 | 0 |
| L1+L4 | Ileum+upper GI | 1 | 2% |
| L2+L4 | Colon+upper GI | 0 | 0 |
| L3+L4 | Ileo-colon +upper GI | 1 | 2% |
| (b) Ulcerative colitis extent | |||
| E1 | Proctitis | 8 | 17% |
| E2 | Left sided | 27 | 57% |
| E3 | Extensive | 12 | 26% |
| (c) Crohn's disease behavior | |||
| B1 | Luminal | 35 | 66% |
| B2 | Stricturing | 9 | 17% |
| B3 | Penetrating | 5 | 9.5 |
| B1+B2 | Luminal+stricturing | 3 | 5.5% |
| B1+B3 | Luminal+penetrating | 1 | 2% |
| B2+B3 | Stricturing+penetrating | 0 | 0 |
| p | Perianal disease | 6 | 5% |
Median time from onset of symptoms until diagnosis was 2 months, but in six cases this period was greater than 12 months (3 cases CD, 3 cases UC). Globally, bowel mass index (BMI) at diagnosis was 24.8 (range 14.5–42.5), for CD patients 23.7 (15.3–42.5) and for UC it was 25.5 (17.5–35.7)
In relation to pediatric population, three cases were CU (two of them extensive), with age at diagnosis as 9, 11 and 12 years respectively. The remaining case was a CD, diagnosed at 5 years, with ileal (long segment) and colonic involvement and luminal behavior.
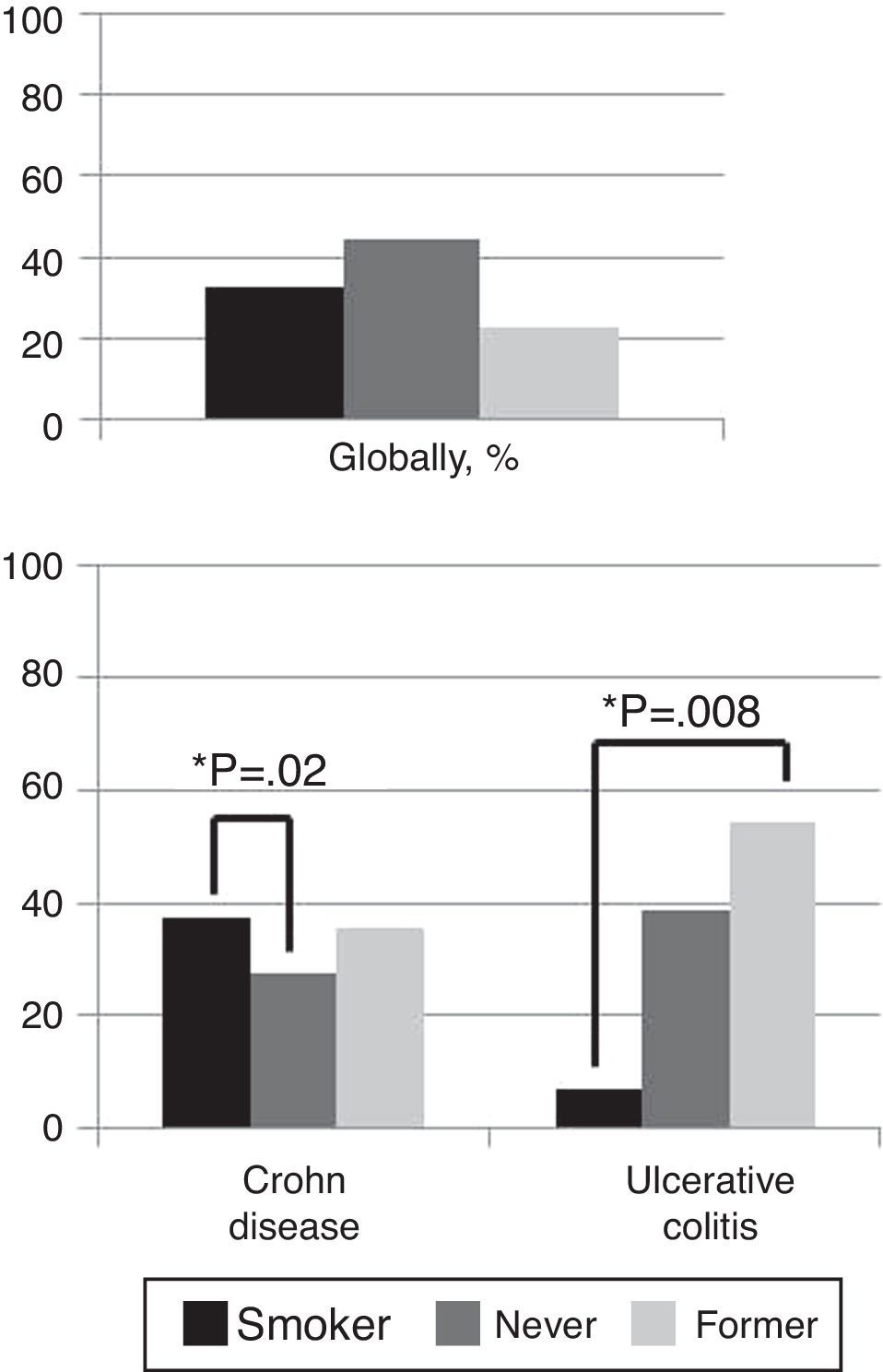
Globally, 32.7% of patients were smokers, 44.6% former smokers and 22.7% never smokers. In CD patients, 37.2% were smokers and 35.3% former smokers contrary to 27.5% who had never smoked (p=0.02). In UC patients only 7% were smokers versus 54.5% former smokers (p=0.008) (Fig. 2).
No statistic significant differences were found between CD and UC patients in terms of age (p=0.4), gender (p=0.5), BMI (p=0.3) or median time from onset of symptoms until diagnosis (p=0.08).
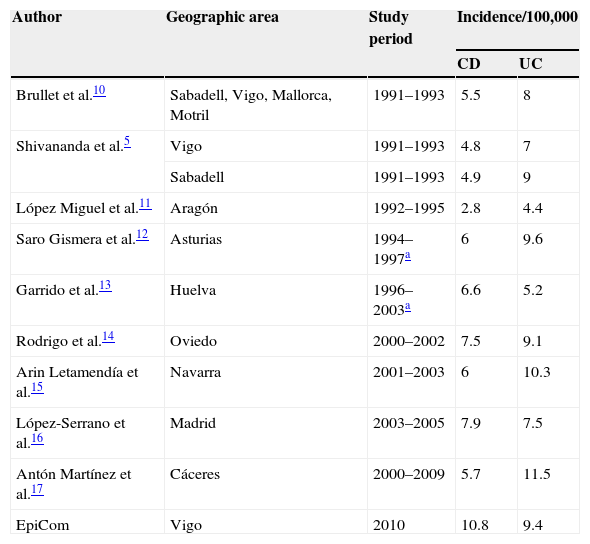
Comparison of the Vigo 2010 cohort with historical Spanish cohortsThe incidence rate of IBD in our study is higher than other Spanish cohorts. Considering only UC, it seems to have no significant differences, but substantial increase appears when comparing CD incidence rates (Table 2).
Incidence rates of Inflammatory Bowel disease in Spain, population-based and prospective studies including results of the EpiCom study.
| Author | Geographic area | Study period | Incidence/100,000 | |
|---|---|---|---|---|
| CD | UC | |||
| Brullet et al.10 | Sabadell, Vigo, Mallorca, Motril | 1991–1993 | 5.5 | 8 |
| Shivananda et al.5 | Vigo | 1991–1993 | 4.8 | 7 |
| Sabadell | 1991–1993 | 4.9 | 9 | |
| López Miguel et al.11 | Aragón | 1992–1995 | 2.8 | 4.4 |
| Saro Gismera et al.12 | Asturias | 1994–1997a | 6 | 9.6 |
| Garrido et al.13 | Huelva | 1996–2003a | 6.6 | 5.2 |
| Rodrigo et al.14 | Oviedo | 2000–2002 | 7.5 | 9.1 |
| Arin Letamendía et al.15 | Navarra | 2001–2003 | 6 | 10.3 |
| López-Serrano et al.16 | Madrid | 2003–2005 | 7.9 | 7.5 |
| Antón Martínez et al.17 | Cáceres | 2000–2009 | 5.7 | 11.5 |
| EpiCom | Vigo | 2010 | 10.8 | 9.4 |
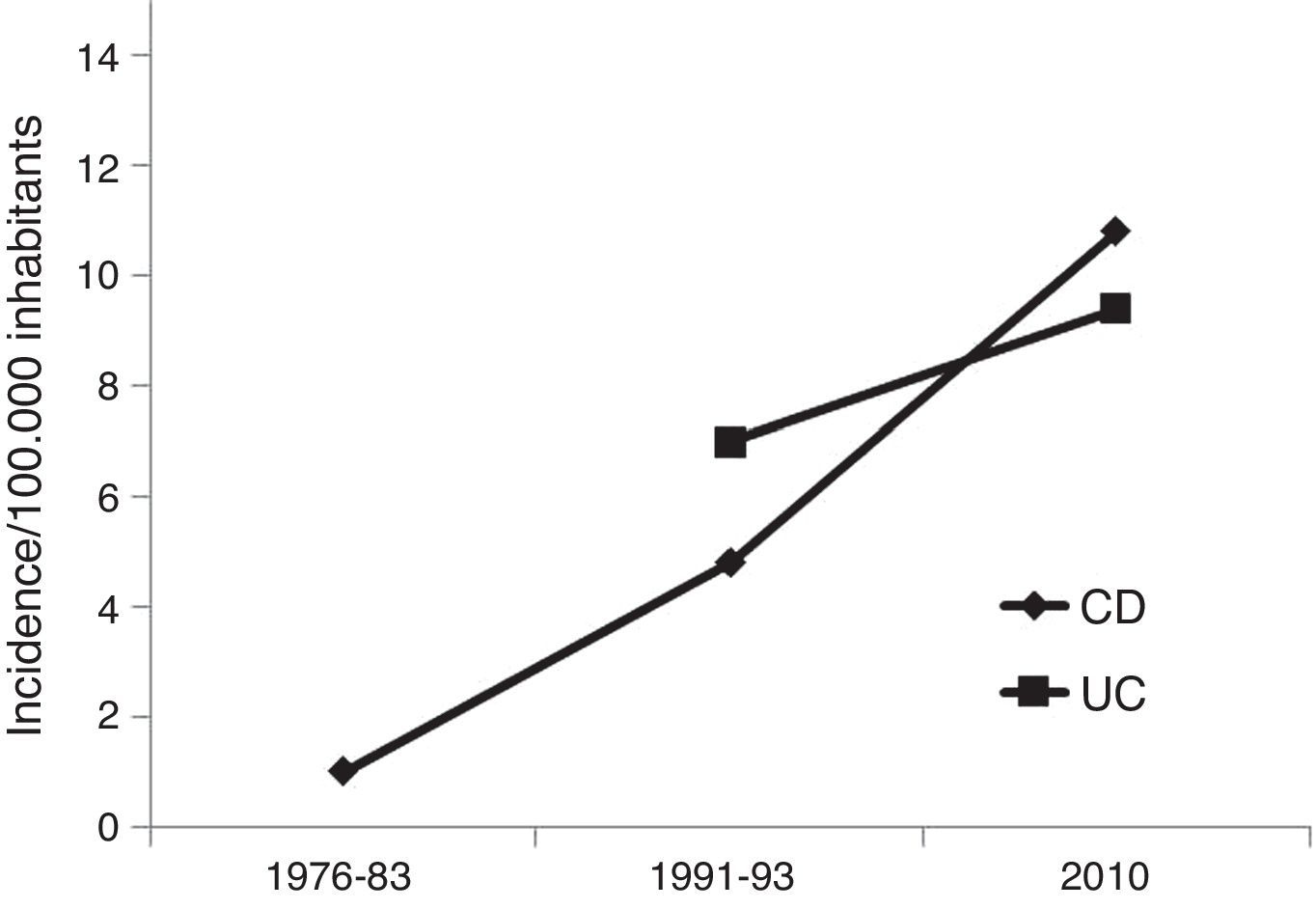
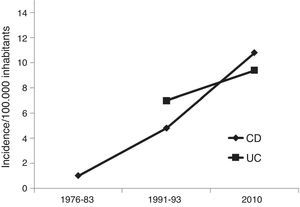
Compared with data previously reported in our uptake area,5,22 a marked increase in incidence is observed: 1/100,000 in 1976–1983, 12.5/100,000 in 1991–1992 and 21.4/100,000 in 2010 (Fig. 3).
DiscussionThe results of our study, compared with previously published data (Table 2, prospective studies), show the highest incidence rate described so far in Spain, mainly due to an increasing incidence of CD. This agrees with a recently published systematic review that reported an increasing incidence of IBD worldwide.1 Focusing in Spain, the trend of the incidence of CD shows a notable increase in the last decade.23
Comparing different geographical areas could lead to a bias in the interpretation of results, even within the same country because of: different population-age distribution, rural-urban environment or reference center versus general gastroenterological clinic. Nevertheless, Vigo area has a consolidated trajectory in epidemiological studies since the initial data published by Dr. Ruíz Ochoa in 1984,22 which were continued in 1991–92 in a European collaborative study.5 Therefore, we can develop a more accurate assessment of the incidence over time. As an example, a summary of previous epidemiological studies developed in Vigo, adding our data, is showed in Fig. 3, where an evident trend of an increasing incidence is shown. However, a study developed in Vigo during the period 1998–2005, including only part of the whole area (almost 180,000 inhabitants), found incidence rates of CD between 9 and 13.9 (median 10.5).24 Although these results are limited, as they do not include the entire Vigo area, taking into account our data, it could suggest that we are probably approaching the maximum peak of incidence.
The increasing trend in incidence is even more evident when European data are compared. In the first European collaborative study EC-IBD developed in 1991–19935 Vigo and Sabadell were the Spanish areas included. The overall incidence rate for UC in all European centers’ participants was 40% higher that all southern European centers; for CD the difference was even greater (80%). Nevertheless, in the setting of the recent EpiCom study,2 our local data are quite similar or even higher than those from areas traditionally considered of high incidence.
The increase in the incidence of IBD in our area is mainly due to an increase in CD incidence. The systematic review by Molodecky et al. reported that 75% of studies found an increase in CD incidence, while only 60% of UC studies reported an increase in incidence.1 Similar evolution over time, with marked increase in the proportion of CD patients, has been described in Northern European countries, also comparing consecutive population-based IBD cohorts.25 UC incidence is usually higher than that of CD, but it seems to be a tendency to a progressive evolution toward equality. In this way, the UC/CD incidence ratio was 1.9/1 in the 1991–93 European Collaborative Study EC-IBD,5 1.7/1 in Navarra (2001–2003),15 1.3/1 in Huelva (1996–2003)13 or 1.5/1 in the EpiCom study (2010).2 In our area, the proportion UC/CD is near to one (0.9/1). Further studies are warranted to elucidate whether this change in the UC/CD incidence ratio reflects a tendency, or is it the result of data collection bias.
In relation to age, IBD traditionally presents a bimodal distribution, with two peaks of incidence at second-third decade and in the last decades of life.26 Median age at diagnosis in UC is usually 5–10 years later than in CD patients.27 Our data confirm this last statement but when the age-standardized incidence rate for CD is analyzed, we find similar levels of incidence during second, third and fourth decades, and a progressive decrease in older patients. In UC patients, we find only one clear peak of incidence at second-third decade and a progressive decrease without the second traditional peak. The EC-IBD study also failed to show the traditional bimodal distribution, and our age-standardized incidence curve is very similar to that found in 1991–93.5 Therefore, we could hypothesize that the age-related pattern of incidence is changing.
A remarkable aspect of our results is phenotypical characteristics at diagnosis of CD patients, especially in relation with behavior. We found structuring disease in 22% patients and penetrating disease in 11%. Isolated inflammatory behavior was described in only 66% of the cases in contrast to other European classical series where this pattern has been described in 75–80% of the cases.28–30 This increased incidence in complicated forms of CD at diagnosis is not exclusive in our area; in the recent EpiCom study, considering globally all participating western European countries, incidence of structuring pattern was 19%, penetrating 5% and pure luminal behavior was 68%.2 This high incidence of aggressive CD could reflect a subset of patients with oligosymptomatic, latent course who did not seek medical assistance until the complication is evident.
Smoking is the most important environmental risk factor of developing IBD and influences the clinical course of the disease. This relationship is antagonistic depending on the type of IBD. Current smoking decreases the risk for UC (42% reduced risk on comparing with never smoking) and being a former smoker has been associated with 1.8 increased risk to develop the disease.31 Even more, smoking is associated with a more benign disease course, reduced risk of colectomy and lower relapse rate,32,33 and cessation of smoking in UC patients with the severity of the disease.34 In contrast, smoking is a major risk factor for developing CD (relative risk increased more than twice)31,35 and these patients generally present a more severe course of CD.36 This risk has been associated also with passive smoking.37 Results of our study completely match with previous published data; particularly in UC where the percentage of smoking patients at diagnosis is very low and there are a high proportion of former smokers.
The present study has a major limitation, the possibility that some cases were missed. To ensure the highest quality data not only was the cases search developed in the Gastroenterology departments but uptake was also expanded to Surgery, Histopathology, Radiology and especially Codification Departments. We found the cooperation with the later particularly useful and important. Some authors worked also in the main private hospitals of our uptake area. With this strategy we cannot ensure 100% capture accuracy, and we believe that we missed a few cases. Moreover, several measures were used to secure the quality and validity of the rates recorded such as audit visits. The use of a unified database and built-in data control give extra strength to the results. Finally, another factor that we believe enhances quality of data is the fact that Vigo area has participated previously in inception cohort trials.
In conclusion, incidence of IBD continues to increase in our area, especially in CD cases, approaching to data of high-incidence countries. Median time since onset of symptoms until diagnosis is relatively short in our area, although there are still few cases with remarkable delay.
FundingThis work has not received any public or private funding.
Conflict of interestThe authors declare no conflict of interest.
We thank Johan Burisch (Copenhagen), Pia Munkholm (Copenhagen) and Peter Lakatos (Budapest) for their useful comments.