La enfermedad inflamatoria intestinal (EII), comprende tanto a la colitis ulcerosa como a la enfermedad de Crohn, entidades consideradas enfermedades inmunomediadas, sistémicas y de curso crónico que conllevan a menudo el desarrollo de manifestaciones extraintestinales. A pesar de que el estudio de las comorbilidades haya sido desarrollado tradicionalmente en contexto de otras enfermedades inflamatorias sistémicas, este concepto está emergiendo también en la EII. Multitud de patologías han sido vinculadas a la EII, entre las que destaca la enfermedad cardiovascular, la primera causa de muerte en los países desarrollados. Los pacientes con EII están expuestos a un mayor riesgo de entidades tales como arterosclerosis precoz e infarto de miocardio o trombosis venosas y tromboembolismo pulmonar. El objetivo de esta revisión, es hacer una aproximación a la fisiopatología de las diferentes manifestaciones de la enfermedad cardiovascular en los pacientes con EII y de cómo prevenirlas.
Inflammatory bowel disease (IBD) includes both ulcerative colitis and Crohn’s disease, which are well recognised as chronic systemic and immune-mediated conditions that frequently involve extraintestinal manifestations. Although comorbidities have long been the subject of research in other chronic inflammatory diseases, this concept is also emerging in IBD. Many pathologies have been linked to IBD, including cardiovascular disease, which is the main cause of death in developed countries. IBD patients are at increased risk of conditions such as early atherosclerosis and myocardial infarction or venous thrombosis and pulmonary thromboembolism. The aim of this review is to make an approximation of the physiopathology of the different manifestations of cardiovascular disease in patients with IBD and how to prevent them.
Crohn’s disease (CD) and ulcerative colitis (UC) are immune-mediated chronic diseases that primarily affect the gastrointestinal tract.1 However, up to a fifth of patients may present compromise of other organs or systems,2,3 thus it seems reasonable to deem them systemic diseases.4,5
Although studies on comorbidity in inflammatory bowel disease (IBD) are less common than studies on rheumatoid arthritis and psoriasis, as early as 1996, Hudson et al. suggested that IBD could represent an independent risk factor for increased cardiovascular (CV) risk.6 Systemic chronic inflammation is associated with early arteriosclerosis,7,8 although other factors such as obesity and metabolic syndrome also contribute significantly to this risk in patients with IBD.9,10
The objectives of this narrative literature review are to evaluate probable factors and mechanisms underlying the increased risk of CV disease in patients with IBD. To do this, a systematic search was conducted using the metasearch engines PubMed, the Cochrane Database and Embase, with no language restriction for the past 10 years.
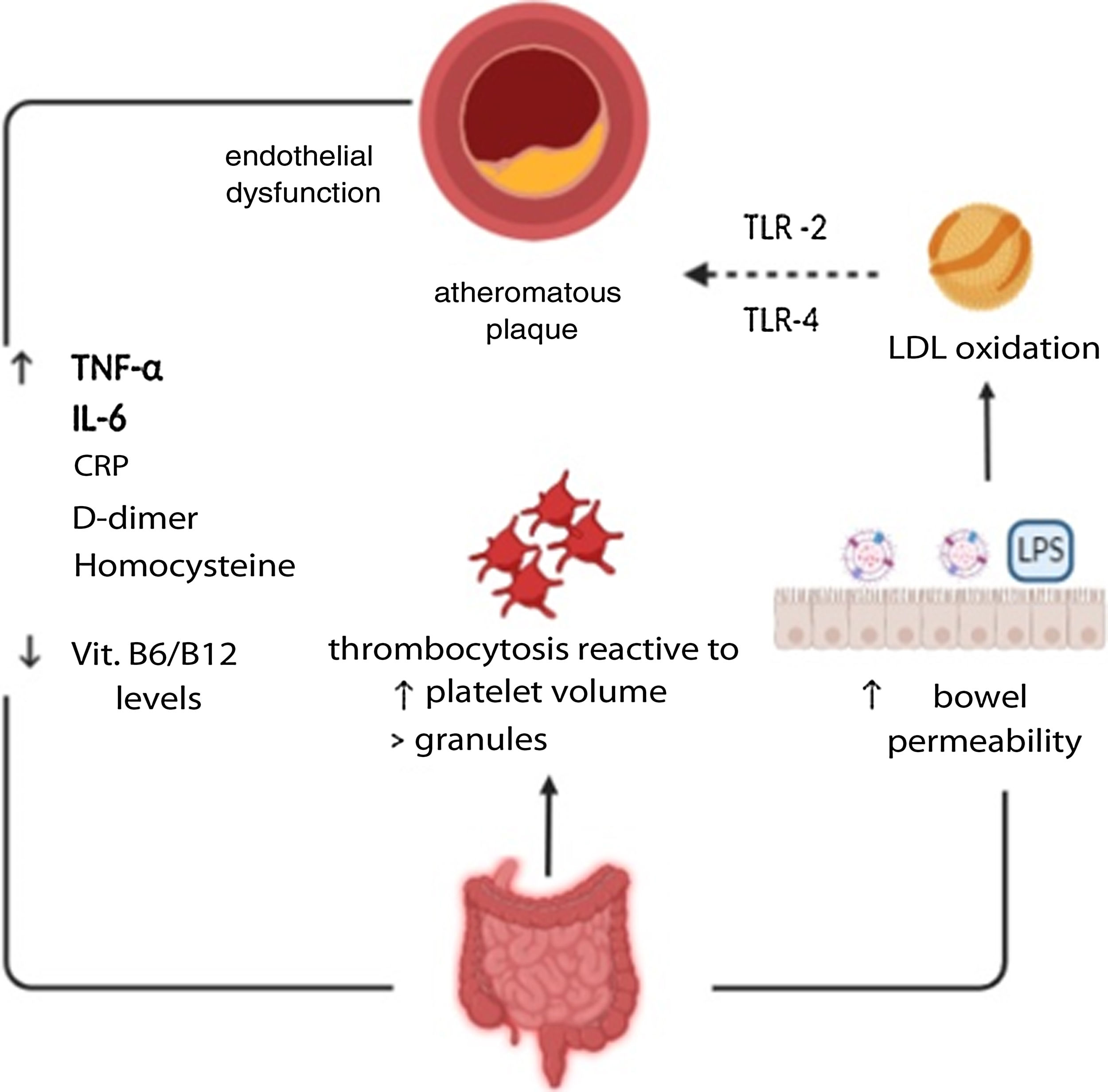
Pathophysiology of cardiovascular disease in patients with IBDArteriosclerosis in patients with IBDArteriosclerosis is a chronic disease with a progressive course, characterised by loss of arterial elasticity. Its precursor lesions consist of subendothelial deposits of cholesterol-laden macrophages. Subsequently, formations of lipids and immune cells (macrophages, mastocytes and T cells) previously activated by micro-organisms, autoantigens and inflammatory molecules constitute true atheromatous plaques located in the intima layer of large and medium vessels.8 The plaques created can be extremely complex, with calcifications and ulcerations on their surfaces. Furthermore, when immune cells are activated, inflammatory cytokines are released, which cause instability in the plaque as they foster the formation of prothrombotic and procoagulant agents. In this way, they may cause complete occlusion of the vessel lumen due to the development of a thrombus on its surface, or because a thrombus has migrated and is acting as an embolus that is occluding the distal portions of the vessel.11
In IBD patients, it is also common to see platelet disorders which may contribute to the phenomenon of atherothrombosis. These were first reported in the late 1960s, when an increased number of platelets was correlated with intensity of clinical inflammatory activity.12 In addition, these are characterised by a larger size and density, which is also correlated with intensity of inflammatory activity. Larger platelets are more active than smaller platelets in terms of metabolism and enzymes. This means that larger platelets have greater thrombotic potential, due to the increase in thromboxane A2 and B2 and expression of the glycoprotein IIb-IIIa receptor. Furthermore, their α-granules release substances such as platelet factor, selectin-P and platelet-derived growth factor, which contributes to neointimal vascular proliferation.13,14
Multiple markers of atherosclerosis have been studied in IBD patients, including acute-phase reactants such as D-dimer and von Willebrand factor.15,16 Another substance involved in its pathophysiology is C-reactive protein (CRP). This is especially elevated during disease flare-ups.17 Tumour necrosis factor alpha (TNF-α), a proinflammatory and proatherogenic cytokine, is also found to be elevated in IBD.18 Similarly, elevated homocysteine levels have been shown to play a role in the pathophysiology of arteriosclerosis, through increased oxidative stress and a drop in nitric oxide levels. In IBD patients, hyperhomocysteinaemia is 4.6 times more common in healthy subjects, especially in times of clinically active disease.19 Decreased levels of vitamin B6 and vitamin B12 have also been found to be related to this increased risk in IBD patients.20,21 Finally, the most specific clinical chemistry parameter associated with inflammatory activity in IBD patients is calprotectin, which has also been shown to be an independent risk factor for suffering from early recurrent CV disease.22
An additional mechanism in IBD patients that may increase thromboembolic risk is increased bowel wall permeability. While this is the main cause of systemic inflammation, it also allows bacterial peptides and micro-organisms to pass directly into the bloodstream, thus causing metabolic endotoxaemia, a direct substrate for the formation of fibrin microclots.23,24 In turn, elevated levels of bacterial lipopolysaccharides may induce proinflammatory cytokines which contribute to endothelial damage and the formation of foam cells (macrophages), stimulating oxidation of the LDLs, which are toxic to the endothelium.25,26 The microbial effect on atherogenesis might be mediated by the toll-like receptors 2 (TLR2) and 4 (TLR4), which are found to be high in atherosclerotic plaques27 (Fig. 1).
Factors associated with cardiovascular risk in patients with inflammatory bowel disease8–17.
The prevalence of overweight and obesity in IBD patients is similar to or greater than that of the general population, as has been observed in some studies.28,29 This may have a deleterious effect on the course of the disease since adipose tissue constitutes a hormonally active organ and is capable of producing proinflammatory cytokines.30 Other risk factors for CV disease, such as diabetes mellitus, may also be seen more often in patients with IBD.31
Dyslipidaemia is one of the main CV risk factors32 and chronic inflammation may lead to significant lipid profile changes.33 Detection of abnormal lipid levels in IBD patients may also be due to a state of malnutrition or malabsorption or a history of bowel resection.34 Some studies have affirmed that IBD patients more frequently have decreased HDL cholesterol levels and elevated LDL cholesterol levels.35 However, increased CV risk has also been reported in spite of decreased levels.36 Thus it appears that more studies are needed on the role played by lipoproteins in the CV risk for these patients.
There is also a reported coexistence of non-alcoholic fatty liver disease and IBD with a prevalence higher than that of the general population,37 such that some authors recommend screening for it.38
Cardiovascular eventsArterial thrombosis: acute myocardial infarction (AMI)/cerebrovascular accidents (CVAs)Bernstein et al. reported a higher risk of arterial thromboembolism phenomena in the population with IBD compared to healthy subjects, noting that cases of cerebral arterial thromboembolism are more common in CD (incidence rate ratio [IRR] 1.26; 95% CI [1.05–1.66]). This has been attributed to, among other factors, this population's higher risk of vitamin B6 deficiency and increased homocysteine levels.39 Anderson's group detected this increased risk in patients under 50,40 and a French study found that inflammatory activity acted as an independent risk factor.41 This was consistent with the data from another study in which the number of AMIs and CVAs was significantly higher in patients with active disease (IRR 1.76 [1.14–2.74] and IRR 1.88 [1.26–2.81], respectively).42
As regards sex, a retrospective cohort of 17,487 IBD patients versus 69,948 control group members found that women over 40 years of age with IBD had a higher risk of AMI (HR=1.6, p=0.003), whereas women under 40 showed a two times higher risk of CVA (HR=2.1, p=0.04) which was not seen in the male population.43 A systematic review also found a higher risk for cardiovascular and cerebrovascular events in women (OR 1.26 [1.18–1.35]) but not in men (OR 1.05 [0.92–1.21]).44 Although women have a lower risk of coronary disease than men in the general population, it appears that women with IBD have higher inflammatory cascade activation, with this playing a key role.45 CV events are more common in the first year following diagnosis, at which point inflammatory activity management may come to represent a real clinical challenge.46
Venous thrombosisThrombotic events represent a significant cause of morbidity and mortality in IBD patients, with a 1.5–4 times higher risk than the general population, especially in periods of disease activity,47 pregnancy and the postpartum period.48,49 The places where they usually manifest are the veins of the legs and lungs, followed by the portal and mesenteric veins. Other more uncommon locations are the cerebrovascular and retinal veins.
To prevent these events, it is important to give patients appropriate counselling, stressing the importance of avoiding a sedentary lifestyle, smoking and oral contraception, as well as staying properly hydrated. Correction of vitamin deficiencies is important, especially vitamin B6, vitamin B12 and folic acid, since they may aid in reducing homocysteine levels.50 During disease flare-ups, prophylactic treatment with heparin may be considered in all cases, according to clinical practice guidelines.51 However, its duration is currently a matter of debate, and there are no randomised controlled studies that might give rise to firm recommendations in this regard.
Pericarditis/myocarditisPericarditis has been seen at a higher rate than in the general population, both in CD (prevalence of 0.19%) and in UC (0.23%), with a greater likelihood in men.48,52 A Danish follow-up study of 15,572 patients found an overall risk of 4.6 cases/100,000 patients/year, with an IRR of 8.3 in CD and 2.6 in UC.49 However, although it might be due to immune-mediated mechanisms, its relationship with treatment with mesalazine or infliximab must always be excluded. Differential diagnosis is complex and may require endomyocardial biopsy.53,54
Rhythm disorders: atrial fibrillation and othersChronic inflammation and electrolyte imbalances are factors that can lead to a prolonged QT interval and therefore ventricular arrhythmias.55 Moreover, a Danish national study of 24,499 IBD patients found a higher incidence of AF during flare-ups (IRR 2.63 [2.26–3.06]) and in the presence of persistent inflammatory activity (IRR 2.06 [1.67–2.55]), but not in periods of clinical remission (IRR 0.97 [0.88–1.08]).56
There is a known increase in prevalence of AF with age. However, in patients with IBD, it has been prospectively observed that there is a higher incidence at younger ages and a significantly higher incidence in patients without associated CV risk factors such as diabetes mellitus, hypertension and dyslipidaemia and in those on treatment with immunomodulators, corticosteroids or biologic therapy (HR 1.46, 1.37 and 2.38, respectively).57
Hence, it is advisable to perform an electrocardiogram on all patients with IBD who present tachycardia, especially hospitalised patients and those in a period of disease flare-up, given the importance of starting the right anticoagulant and antiarrhythmic treatment early.58
Treatment for IBD and CV risk- -
Corticosteroids: Corticosteroid treatment has been found to be linked to increased CV risk.46 This effect might be explained by the influence of corticosteroids on the appearance of traditional CV risk factors leading to higher CV risk also in the general population.
- -
5-aminosalicylates (5-ASA): A study led by Rungoe46 found that treatment with 5-ASA drugs is linked to a dose-dependent reduction in CV risk in IBD patients.
- -
TNF inhibitors (infliximab, adalimumab, certolizumab and golimumab): There seem to be no differences with regard to CV risk in patients on TNF inhibitor treatment compared to patients not on said treatment (IRR 0.6; 95% CI 1,16–1,32).46 However, it is important to consider that TNF inhibitors are contraindicated in patients with moderate to severe heart failure.59
- -
α4β7 integrin inhibitors: Vedolizumab appears to be a safe drug from a CV perspective, as recently reported by Cross et al. after evaluating the adverse effects reported to the FDA for a year in patients on treatment with TNF inhibitors and vedolizumab.60
- -
JAK inhibitors: These have been linked to a greater tendency to present lipid profile abnormalities61 and develop venous thrombosis events in patients with rheumatoid arthritis, over 65 years of age and on high doses (10mg twice daily).62,63
In recent years, IBD patients have been found to be exposed to higher CV risk. The pathophysiology leading to this increased risk is not definitively understood. However, the data available suggest that the consequences of systemic inflammation may play a significant role.
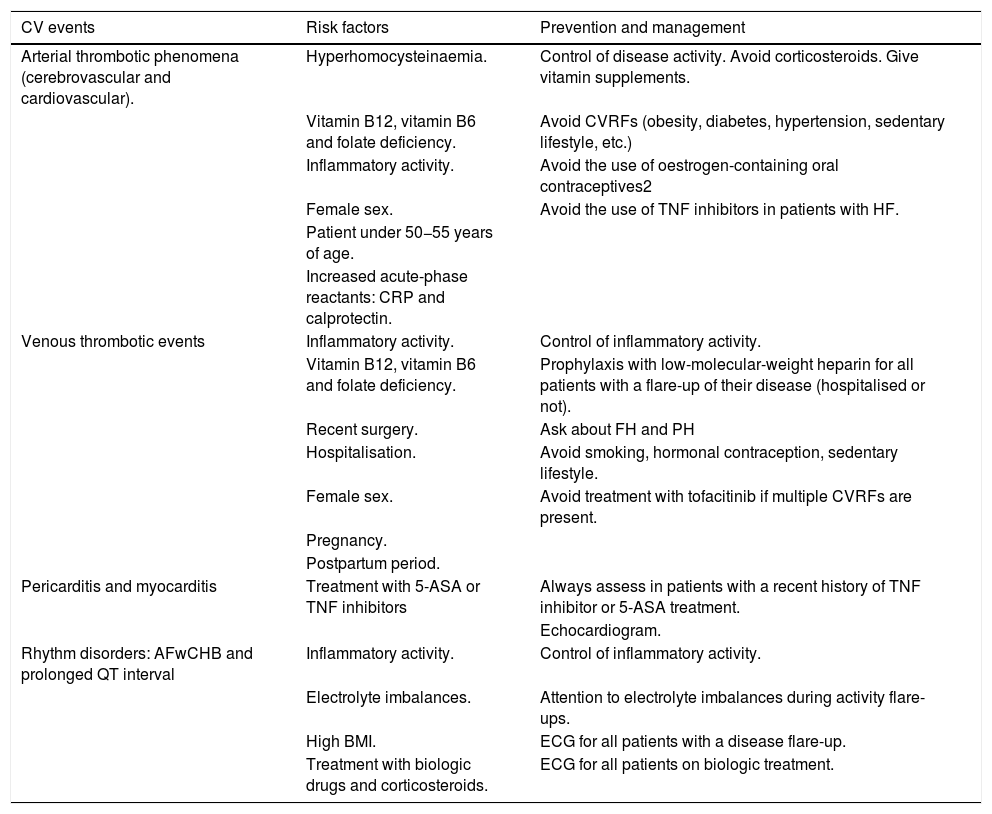
In this way, an increase in both venous and arterial events has been found, with the latter being more common. The main arterial events are cerebrovascular. They occur most often in young patients, in women and during periods of disease activity, when they may include signs and symptoms of pericarditis and arrhythmia. Therefore, it is vitally important to manage inflammatory activity, which could decrease the likelihood of developing these complications. Table 1 shows the main CV events reported in IBD patients, their risk factors and tools for prevention.
Cardiovascular events associated with inflammatory bowel disease.
| CV events | Risk factors | Prevention and management |
|---|---|---|
| Arterial thrombotic phenomena (cerebrovascular and cardiovascular). | Hyperhomocysteinaemia. | Control of disease activity. Avoid corticosteroids. Give vitamin supplements. |
| Vitamin B12, vitamin B6 and folate deficiency. | Avoid CVRFs (obesity, diabetes, hypertension, sedentary lifestyle, etc.) | |
| Inflammatory activity. | Avoid the use of oestrogen-containing oral contraceptives2 | |
| Female sex. | Avoid the use of TNF inhibitors in patients with HF. | |
| Patient under 50−55 years of age. | ||
| Increased acute-phase reactants: CRP and calprotectin. | ||
| Venous thrombotic events | Inflammatory activity. | Control of inflammatory activity. |
| Vitamin B12, vitamin B6 and folate deficiency. | Prophylaxis with low-molecular-weight heparin for all patients with a flare-up of their disease (hospitalised or not). | |
| Recent surgery. | Ask about FH and PH | |
| Hospitalisation. | Avoid smoking, hormonal contraception, sedentary lifestyle. | |
| Female sex. | Avoid treatment with tofacitinib if multiple CVRFs are present. | |
| Pregnancy. | ||
| Postpartum period. | ||
| Pericarditis and myocarditis | Treatment with 5-ASA or TNF inhibitors | Always assess in patients with a recent history of TNF inhibitor or 5-ASA treatment. |
| Echocardiogram. | ||
| Rhythm disorders: AFwCHB and prolonged QT interval | Inflammatory activity. | Control of inflammatory activity. |
| Electrolyte imbalances. | Attention to electrolyte imbalances during activity flare-ups. | |
| High BMI. | ECG for all patients with a disease flare-up. | |
| Treatment with biologic drugs and corticosteroids. | ECG for all patients on biologic treatment. |
CHBwAF: complete heart block with atrial fibrillation; CV: cardiovascular; CVRFs: cardiovascular risk factors; ECG: electrocardiogram; FH: family history; PH: personal history. BMI: body mass index; CRP: C-reactive protein; HF: heart failure.
Finally, short- and long-term treatments used must be taken into consideration as they may contribute to an increased CV risk in these patients.
FundingNo funding of any kind was received to prepare this article.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Nuñez P, García Mateo S, Quera R. Gomollón F. La enfermedad inflamatoria intestinal y los riesgos de enfermedad cardiovascular. Gastroenterol Hepatol. 2021;44:236–242.