We present a case of a 58 years-old female with no past medical history but several cervical spine surgeries due to a traumatic cervical fracture and later on due to pseudoarthrosis of the osteosynthesis plate. The patient refers years of cough after food intake accompanied by vomiting, which had been getting worse recently. These symptoms appear with both solids and liquids, and the patient complains that they began after surgical interventions.
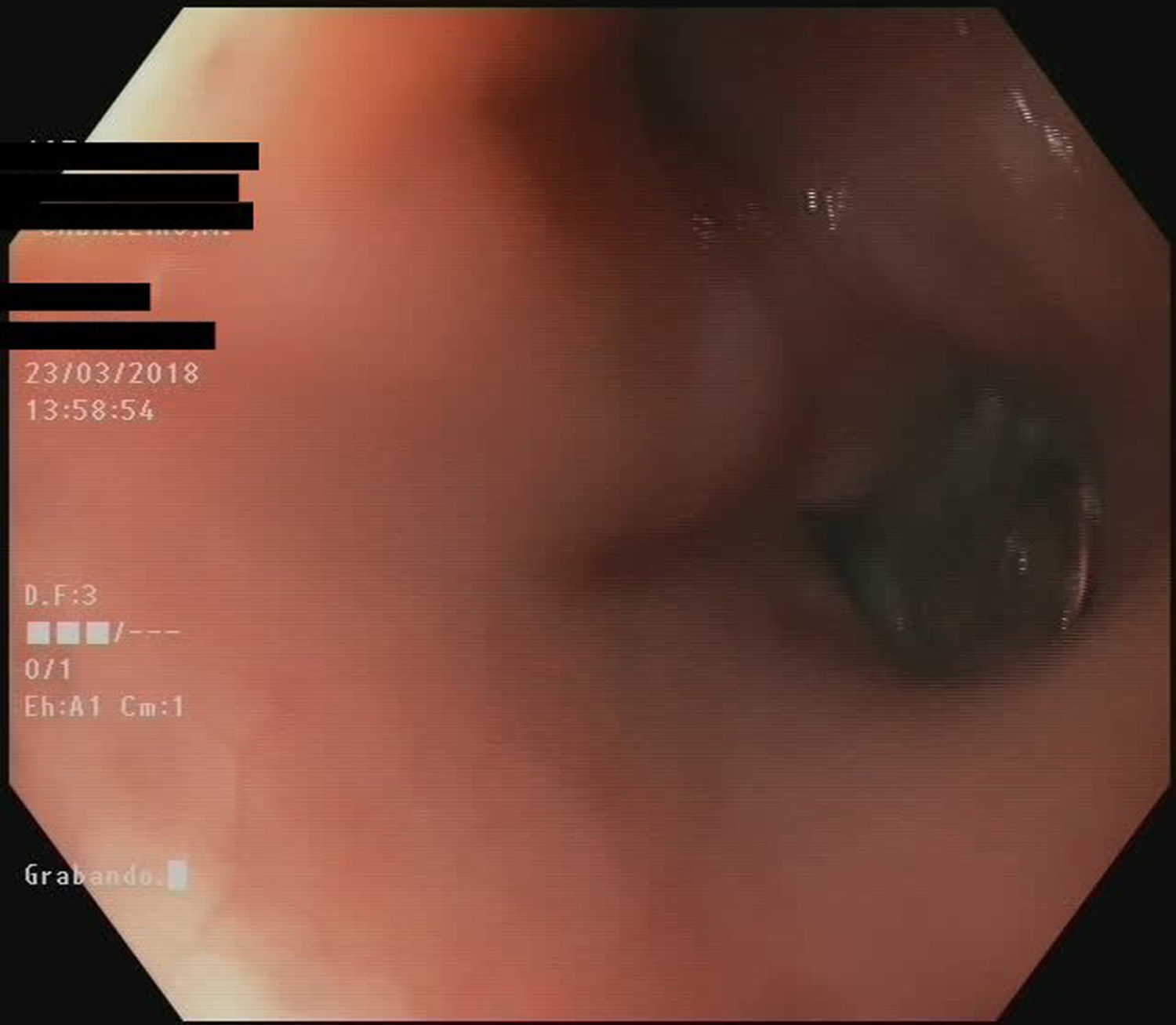
An esophageal transit and CT Scanner were performed as the first diagnostic test showing the presence of a diverticulum in close relationship with the osteosynthesis plate with contrast leak at that level (Fig. 1). A gastroscopy was requested. A diverticulum was observed and inside it, osteosynthesis material, that had eroded the wall and penetrated into its lumen (Figs. 2 and 3) (Video 1).
The case was discussed, and combined surgery was performed. Neurosurgery department removed the osteosynthesis plate, and esophagogastric surgeons completed diverticulectomy. The operation was carried out without complications, and the patient was discharged, asymptomatic, and tolerating a regular diet.
The literature on the esophageal complications of cervical surgery is scarce. Surgery of the cervical spine with anterior approach can lead to multiple complications, however most of them are extremely rare. Dysphagia is one of the most frequent (transient 5–30%, dysphagia 0.8–5%).1 In cervical surgeries, esophageal perforation occurs between 0.25% and 1%, and pharyngeal perforation around 0.2–1.2%,2,3 it usually occurs in the upper cervical region. In most cases, it is not detected during surgery, and symptoms appear later as local infection, fistula, sepsis, or mediastinitis. It often occurs as a result of tissue retraction or graft displacement.