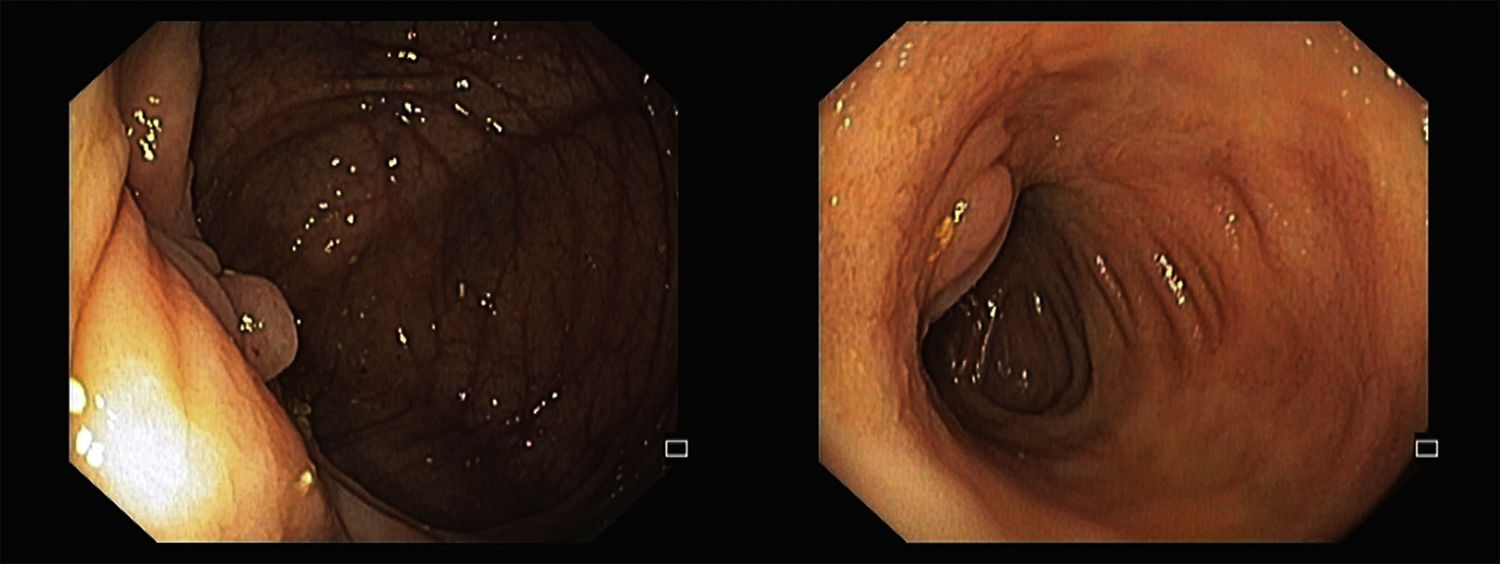
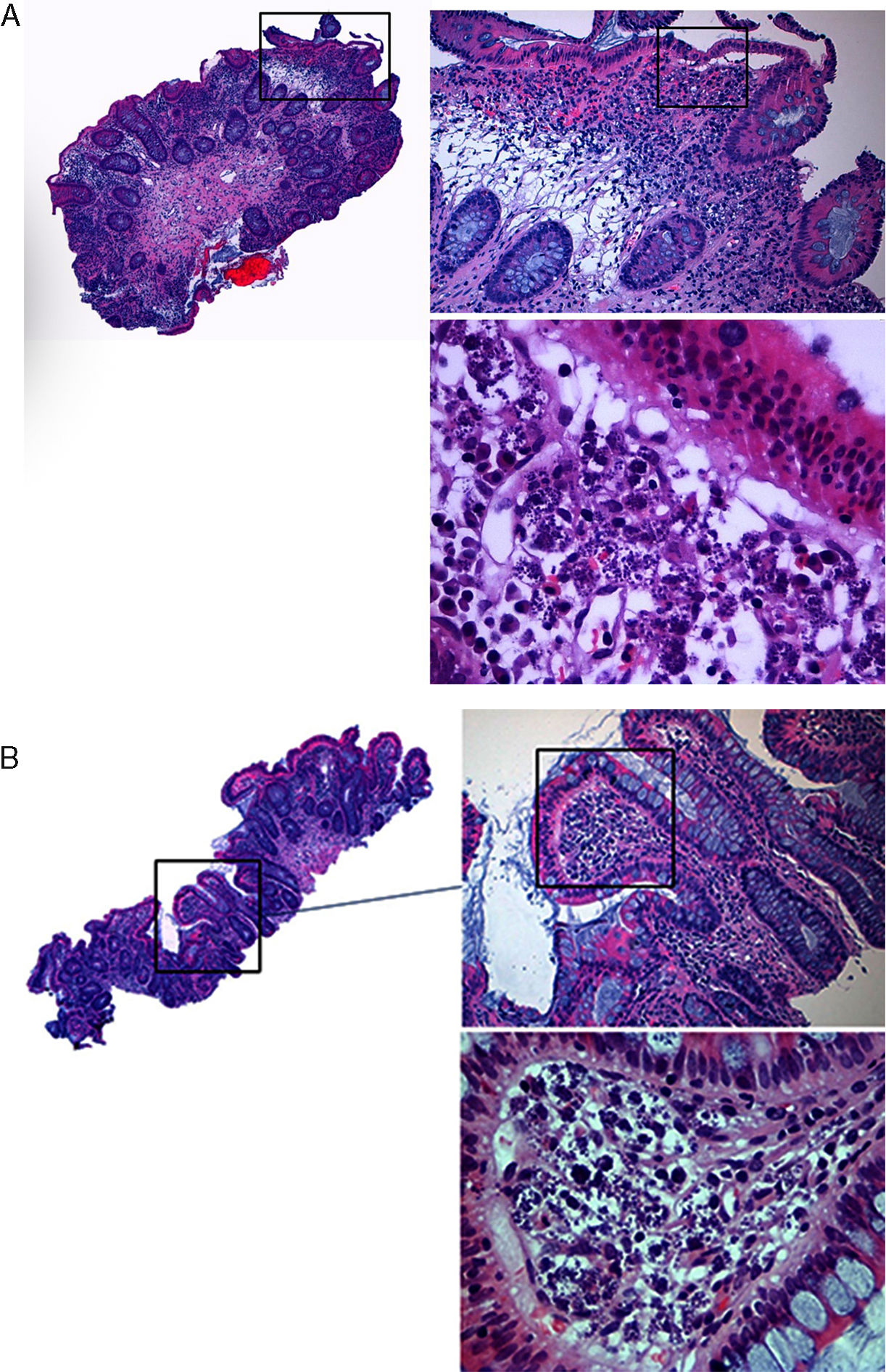
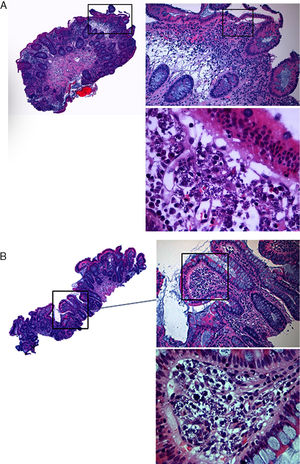
A 41-year-old male, journalist, with a history of ileal Crohn's disease (CD), stricturing phenotype, diagnosed in 2011, and renal transplant in 2014 due to IgA nephropathy. He referred several trips to the Middle East in recent years and he was immunosuppressed with tacrolimus and prednisolone. Due to CD activity and malabsorption of immunosuppressive drugs, infliximab was initiated a few months after transplant, with clinical improvement. Two years later, the patient reported a slight increase of his bowel movements. Physical examination was relevant for hepatosplenomegaly. Lab workup showed pancytopenia and stool cultures were negative. The ileocolonoscopy showed scarring areas and pseudopolyps of the terminal ileum and the right colon (Fig. 1). Biopsies were performed in the right colon and in the terminal ileum, and the pathological exam revealed preservation of the glandular architecture of the mucosa, with an inflammatory lymphoplasmocytic infiltrate and macrophages with spherical and small amastigotes structures of Leishmania sppI (Fig. 2). Polymerase chain reaction analysis of the biopsy specimens was performed and confirmed the presence of Leishmania infantum. HIV screening test was negative. The patient started therapy with liposomal amphotericin B.
Leishmaniasis is a chronic protozoan disease of the mononuclear phagocytic system.1Leishmania spp is endemic in several regions of the world, including the Mediterranean área.1 The incubation period is usually long, and under conditions of immunosuppression, there is evidence of activation of latent infection several years after exposure to the parasite.1 TNF-α has a major role in mediating host protection against visceral leishmaniasis (VL), so the use of anti-TNF agents may potentially cause worsening or reactivation of latent infection.1,2
Cutaneous leishmaniasis is the most common leishmanial syndrome worldwide.3 VL, which reflects dissemination of Leishmania parasites throughout the reticuloendothelial system, is potentially life threatening without treatment.2 VL is a systemic disease characterized by hepatosplenomegaly, fever, cachexia, hypergammaglobulinaemia, and pancytopenia.1 Nevertheless, asymptomatic leishmanial infection has been reported previously.1
The diagnosis of enteric VL is histological, requiring visualization of amastigotes inside macrophages of the intestinal lamina própria.4,5 A characteristic endoscopic image of this invasion has not been described so far, and the diagnosis is established by taking biopsies.4,5 A correct diagnosis of VL is challenging and easy to miss, especially in cases that are not clinically suspected, as the case reported. Liposomal amphotericin B is the preferred treatment choice.5