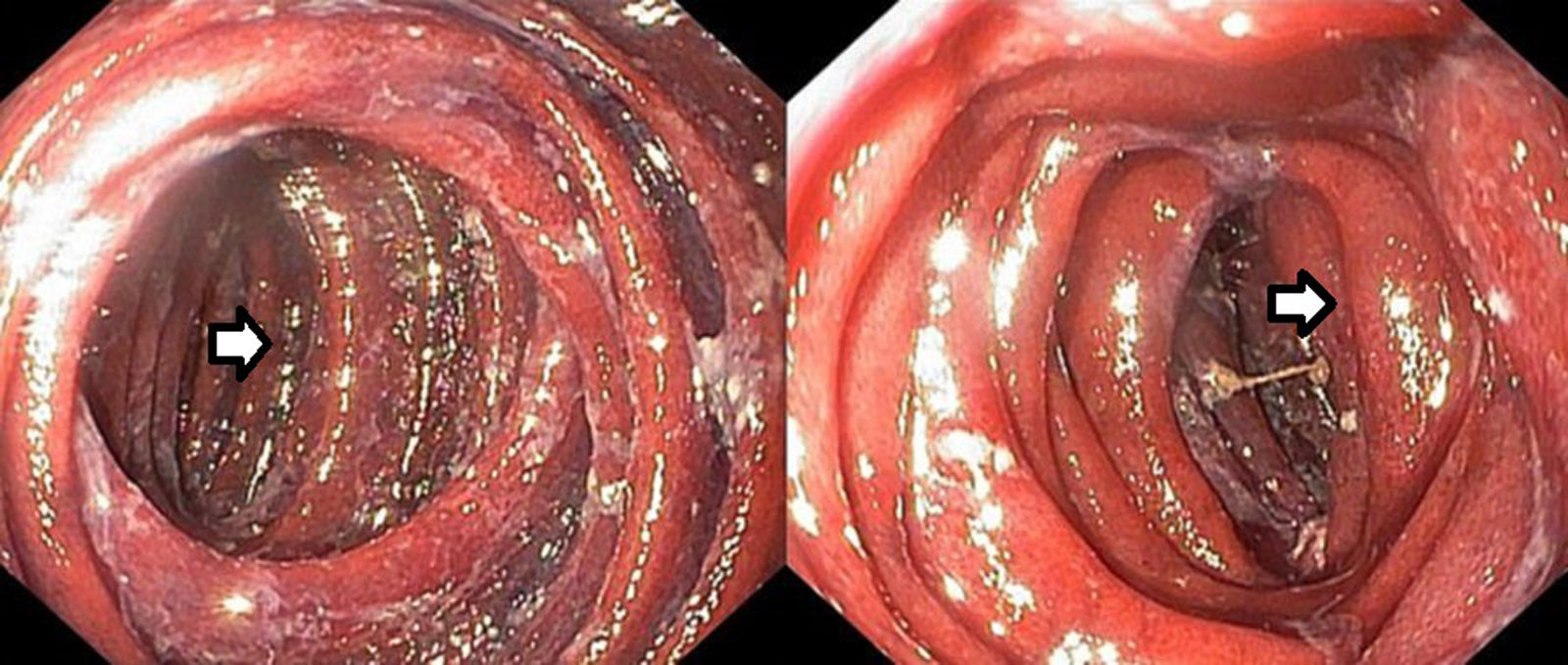
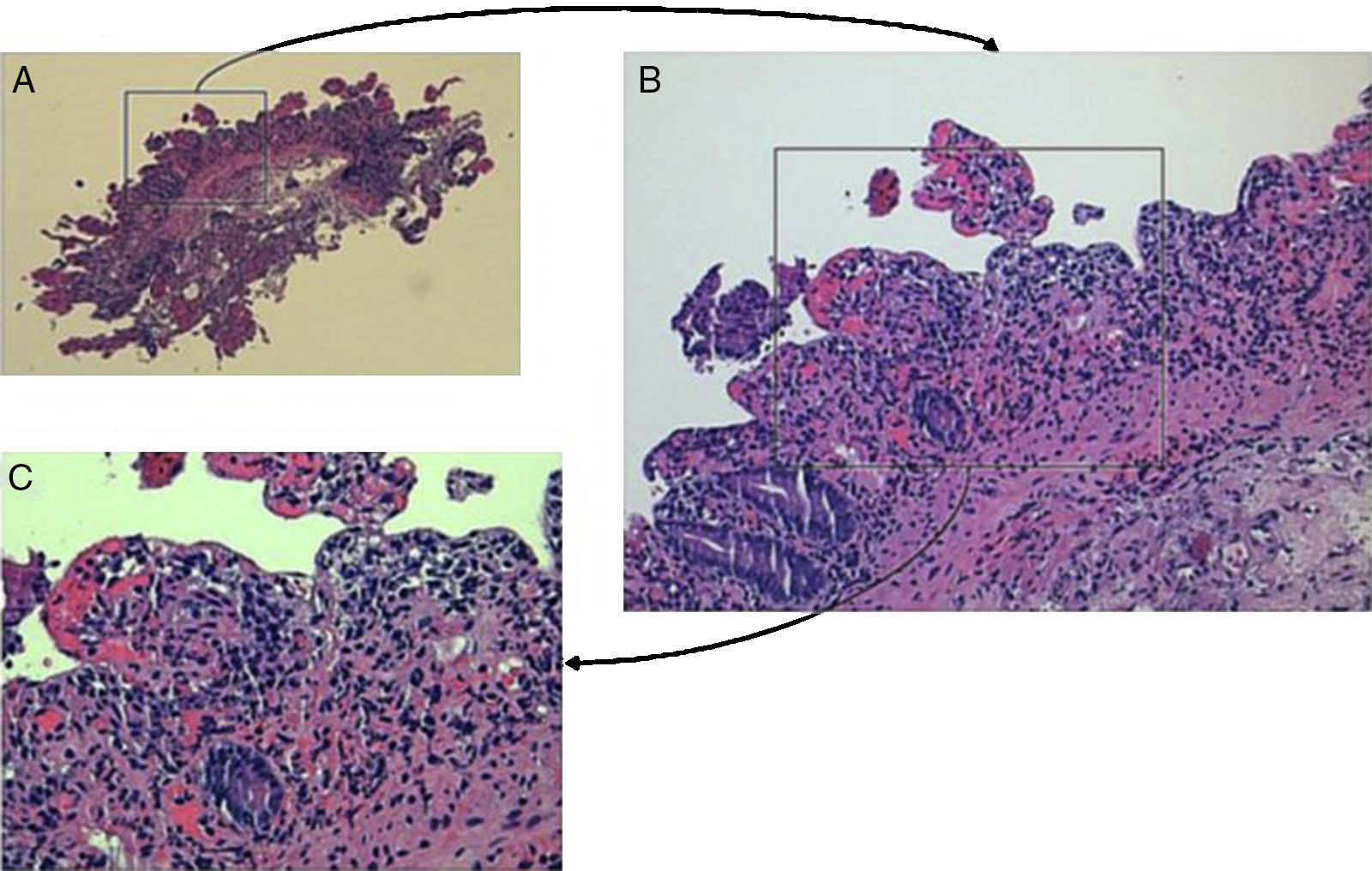
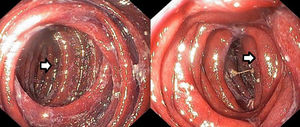
The authors present the case of an 83-year-old woman submitted a month before to a total gastrectomy for gastric adenocarcinoma who admitted to the emergency department with hematemesis. After resuscitation and hemodynamic stabilization an upper endoscopy was performed that showed a regular esophagojejunal anastomosis in healing process; however, in the efferent jejunal loop the mucosa appeared edematous, of purplish appearance, with superficial ulceration and exudate, and friability with spontaneous bleeding (Fig. 1). Biopsies were performed. With the suspicion of ischemic enteritis a CT angiography was performed that revealed a conglomerate of jejunal loops with wall thickening and increased uptake of the mucosa, with tightness and twist of the mesenteric vessels (Fig. 2). The arterial vessels seemed patent, however the mesenteric veins had become globular with aspects suggestive of an ischemic process by venous congestion. The patient then underwent laparotomy where was noted migration/herniation of entero-enteric anastomosis of the “Y-en-Roux” to the supramesocolic floor through the mesocolon, confirming the presence of mesenteric torsion and venous congestion conditioning edema and endoluminal bleeding. The ischemic segment was resected and new anastomosis were performed. The patient was discharged after 14 days under oral nutrition. Later, histology evaluation confirmed the diagnosis of ischemic enteritis (Fig. 3).
In the literature there are rare cases of ischemic enteritis, particularly non-duodenal ischemia, documented by endoscopy, since most of the cases are diagnosed by imaging, and especially surgery.1 Ischemic enteritis can be classified as either occlusive or nonocclusive. Embolism and thrombosis of the superior mesenteric artery causes this disease entity in 30% and 25% of all patients, respectively.2 Nonocclusive ischemic enteritis occurs in 25% of all patients.2 The jejunum is affected in 20% of all patient and the ileum in 45–55% of all patients.2 This condition, although infrequent, primarily affects people over 60, especially with diffuse atherosclerotic disease.3 However, cases at earlier ages are described primarily in the context of autoimmune diseases.4 Given its high mortality rate, early diagnosis is crucial to the prognosis.5 However, because most patient has unspecific symptoms such as pain and abdominal distension, the diagnosis is often delayed. Contrast-enhanced imaging can establish the diagnosis in a significant percentage of cases, however emergent surgery is performed in most cases to diagnosis and possibly treatment.1 The endoscopic diagnosis is rarely made, except where blood loss is observed, usually hematochezia.6 Hematemesis as a form of presentation is extremely rare.7 Internal hernia after gastrectomy with Roux-Y reconstruction is likely underreported (5% in a series of 298 patients underwent gastrectomy for cancer with Roux-Y reconstruction).8 A high degree of suspicion for internal hernia should be maintained in patients presenting with emesis or abdominal pain after gastrectomy with Roux-Y reconstruction, especially after laparoscopic or total gastrectomy. Closure of mesenteric defects after laparoscopic and total gastrectomy should be considered when technically feasible. In our case due to surgical foregoing, the presence of an esophageal-jejunal anastomosis facilitated due to the presence of hematemesis proximal paresis of secondary loops to ischemia. In this case the endoscopic findings suggestive of ischemia allowed the rapid treatment of the patient, improving their prognosis. To our knowledge this is the first case described in the context of total gastrectomy for gastric carcinoma (Fig. 3).