Gastrointestinal stromal tumours (GISTs) are the most common mesenchymal tumours of the digestive tract with malignant potential. The current risk classification standard is unable to accurately evaluate the invasiveness and clinical outcomes of GISTs. Ki-67 labelling index (LI) may be an effective indicator in assessing tumour invasiveness and prognosis, however, its exact value in GISTs is still uncertain. The aims of our study were to evaluate the correlation of the Ki-67 LI and clinicopathological features of GISTs and to assess the potential value of the Ki-67 LI in GISTs classification and prognosis.
MethodsThe clinical, pathological and prognostic data were collected and analysed to identify the independent influential factors of GISTs risk stratification and the predictors of GISTs prognosis.
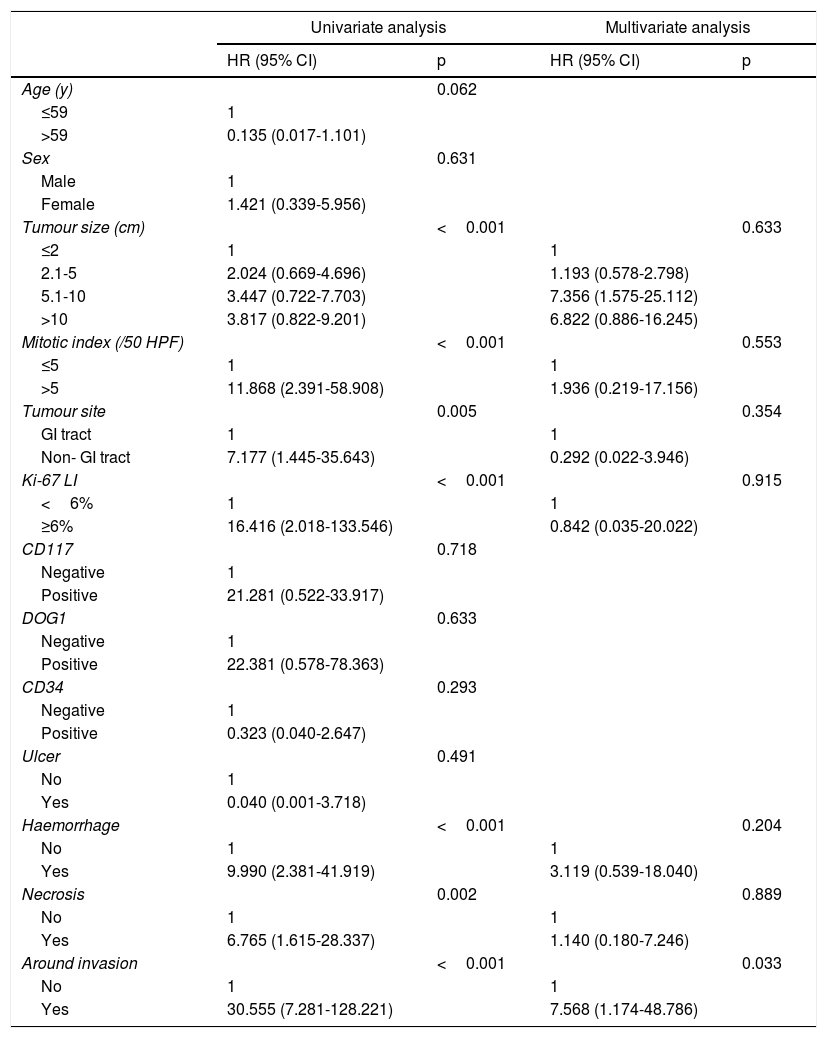
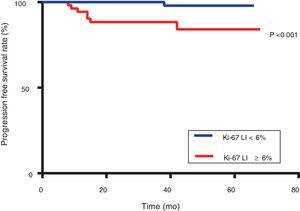
ResultsThe Ki-67 LI was significantly associated with the clinicopathological features of tumour progression (P<0.05). It was an independent influential factor of GISTs risk classification (odds ratio: 1.322; 95% confidence interval: 1.031-1.696) (P=0.028), and the area under the curve (AUC) value of the Ki-67 LI on the discrimination ability of GISTs risk stratification was 0.906 (P<0.001). The optimal cutoff value of the Ki-67 LI was 6% (sensitivity of 87.5% and specificity of 76.2%), and patients with Ki-67 LI≥6% exhibited significantly poorer progression-free survival (PFS) than those with Ki-67 LI<6% (P<0.001). The AUC value of the Ki-67 LI for predicting PFS in postoperative patients was 0.813 (P=0.03).
ConclusionsThe Ki-67 LI has appreciated value to predict the risk grade and prognosis of GISTs. Patients with Ki-67 LI≥6% are prone to recurrence and metastasis after operation and may need a close follow-up.
Los tumores del estroma gastrointestinal (TEGI) son los tumores mesenquimatosos más frecuentes del tubo digestivo con capacidad maligna. Las pautas actuales de clasificación del riesgo no permiten evaluar con precisión la invasividad y los resultados clínicos de los TEGI. El índice de proliferación celular (IPC) Ki-67 puede ser un indicador eficaz para evaluar la invasividad y el pronóstico del tumor, pero todavía existe incertidumbre respecto a su valor exacto en los TEGI. Los objetivos de nuestro estudio fueron evaluar la correlación del IPC Ki-67 y las características clinicopatológicas de los TEGI y evaluar el posible valor del IPC Ki-67 en la clasificación y el pronóstico de los TEGI.
MétodosSe recopilaron y analizaron los datos clínicos, anatomopatológicos y pronósticos para identificar los factores influyentes independientes de la estratificación del riesgo de los TEGI y los factores predictivos del pronóstico de los TEGI.
ResultadosEl IPC Ki-67 se asoció de manera significativa a las características clinicopatológicas de la progresión tumoral (p<0,05). Fue un factor influyente independiente de la clasificación del riesgo de los TEGI (oportunidad relativa: 1,322; intervalo de confianza del 95%: 1,031-1,696) (p=0,028), y el valor del área bajo la curva (AUC) del IPC Ki-67 sobre la capacidad de discriminación de la estratificación del riesgo de los TEGI fue de 0,906 (p<0,001). El valor óptimo de corte del IPC Ki-67 fue del 6% (sensibilidad del 87,5% y especificidad del 76,2%), y los pacientes con un IPC Ki-67 ≥6% mostraron una supervivencia sin progresión (SSP) significativamente peor que aquellos con IPC Ki-67 <6% (p<0,001). El valor AUC del IPC Ki-67 para predecir la SSP en los pacientes postoperatorios fue de 0,813 (p=0,03).
ConclusionesEl IPC Ki-67 tiene un gran valor para predecir el grado de riesgo y el pronóstico de los TEGI. Los pacientes con IPC Ki-67 ≥6% son propensos a la recidiva y metástasis después de una operación y pueden necesitar un estricto seguimiento.
Gastrointestinal stromal tumours (GISTs) are the most common mesenchymal tumours of the gastrointestinal tract, and the annual incidence rate is 6.8-14.5/million.1 The main pathogenesis of GISTs is the continuous activation of the receptor tyrosine kinase due to an acquired mutation in the c-kit gene 2or in the platelet-derived growth factor receptor alpha gene,3 leading to sustained proliferation and tumourigenesis. GISTs can occur in any part of the digestive tract; they are most often found in the stomach, followed by the small intestine, the rectum, and the oesophagus.4 GISTs can also occur outside of the gastrointestinal tract, such as in the omentum, mesentery, and retroperitoneal space.5 Usually, GISTs have an insidious onset without specific clinical presentations, and some are asymptomatic, being discovered accidentally during a physical examination or another operation.6
GISTs are considered potential malignant tumours because they have complex biological behaviours and multidirectional differentiation potential, which can range from benign to highly invasive and even metastatic. It is difficult to define the benign and malignant features of GISTs according to clinical and histological characteristics. At present, the risk of GISTs is often measured by the modified National Institutes of Health (NIH) classification system.7 However, this risk classification system is unable to accurately evaluate the invasiveness of GISTs and other clinical outcomes. Although the tumours are classified as the same risk grade according to the NIH classification, their clinicopathological characteristics, biological behaviours and prognosis are not the same. Some low risk grade GISTs with a small tumour size and a low mitotic index may recur and metastasize after radical operation.8 Therefore, it is necessary to continue to explore other indicators related to the risk of GISTs and prognosis to further improve and supplement the current risk classification standard.
Ki-67 is a nuclear antigen that is closely related to cell mitosis and serves as an indicator of cell division and proliferation. An increasing number of reports have shown that the Ki-67 labelling index (LI) is associated with the prognosis of malignant tumours such as cervical cancer, hepatocellular carcinoma, lymphoma, breast cancer and lung cancer.9–13 The results indicate that the higher the Ki-67 LI is, the stronger the invasiveness and the higher the likelihood of tumours metastasis and recurrence, which results in shorter progression-free survival (PFS) and lower overall survival. These findings strongly suggest that Ki-67expression in tumour tissue may be an effective indicator to judge the invasiveness of tumours and to evaluate prognosis. However, the clinical value of the Ki-67 LI in GISTs has not yet been fully clarified.
In this study, we performed a retrospective analysis to analyse the feasibility of the Ki-67 LI in assessing the GISTs risk classification and to explore the potential value of the Ki-67 LI in GISTs prognosis.
Materials and MethodsEthics statementThis study was approved by the Ethics Committee (Ethical number: Scientific ethics [20182052]). Informed consent was exempted because of the use of retrospective clinicopathological data, and all information was anonymous.
Patient selectionThis retrospective study was conducted on patients diagnosed with GISTs between June 2013 and June 2018. Medical records were reviewed to obtain the patients’ clinicopathological and follow-up data. The inclusion criteria were as follows: (1) patients were radically resected by endoscopy or surgery and clearly diagnosed by pathology, (2) primary GISTs and no other preoperative treatment, (3) complete clinicopathology data, and (4) no other malignant tumour.
VariablesFrom the clinical data, sex, age, symptoms, and clinical progression were recorded. Pathological records included tumour size, mitotic index, tumour site, Ki-67 LI, positive rate of related immunohistochemistry (CD117, DOG1 and CD34), and tumour with ulcer, haemorrhage, necrosis and metastasis. The follow-up period of patients was calculated from the date of the operation until the last follow-up visit. The prognosis was classified as good (PFS) or poor (the patient died due to GISTs or survived but had metastases or recurrence during follow-up).
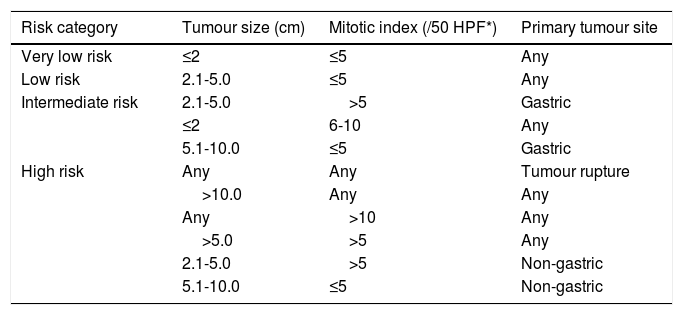
Risk assessmentReferring to the modified NIH GISTs risk category,7 according to tumour size, tumour site, mitotic index, and tumour rupture, GISTs were classified into four risk grades: very low, low, intermediate, and high risk (Table 1).
Modified National Institutes of Health risk classification7
| Risk category | Tumour size (cm) | Mitotic index (/50 HPF*) | Primary tumour site |
|---|---|---|---|
| Very low risk | ≤2 | ≤5 | Any |
| Low risk | 2.1-5.0 | ≤5 | Any |
| Intermediate risk | 2.1-5.0 | >5 | Gastric |
| ≤2 | 6-10 | Any | |
| 5.1-10.0 | ≤5 | Gastric | |
| High risk | Any | Any | Tumour rupture |
| >10.0 | Any | Any | |
| Any | >10 | Any | |
| >5.0 | >5 | Any | |
| 2.1-5.0 | >5 | Non-gastric | |
| 5.1-10.0 | ≤5 | Non-gastric |
HPF: High-power fields
Statistical analysis was carried out using SPSS 23.0 (IBM Corporation, Armonk, New York, USA). In the univariate analysis, χ2, Fisher, and Mann-Whitney U tests were used. The relationship between two variables was examined by the coefficient of contingency, Spearman's rank correlation coefficient. In the multivariate analysis, for factors that showed statistical significance in the univariate analysis, we used logistic regression. The optimal cutoff value was determined by the receiver operating characteristics (ROC) curve. Survival analysis was performed using the Kaplan-Meier method and the log-rank test to reveal the relationship between different groups and prognosis. Statistically significant variables in the survival analysis were enrolled into the multivariate Cox proportional hazards model. The statistically significant value was p <0.05.
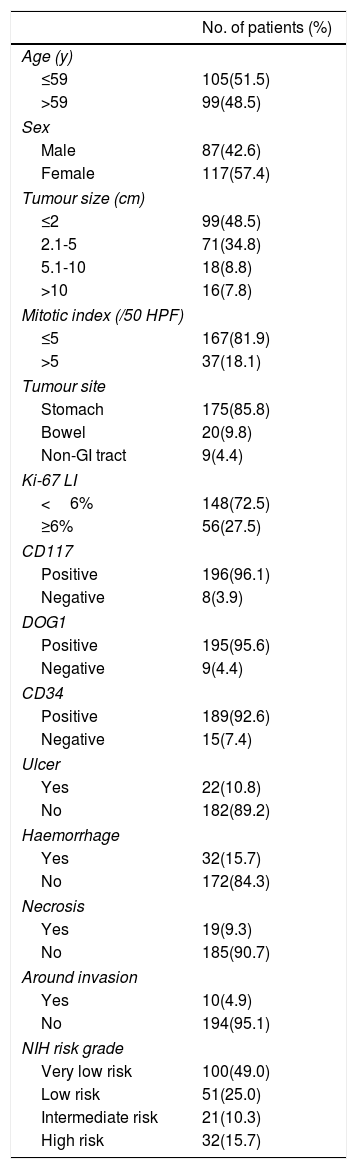
ResultsClinicopathologic features and follow-up dataAccording to the above criteria, a total of 204 patients were included in the study. The clinicopathological features of the patients are shown in Table 2. The median age was 59 years, with an age range of 26-81 years. A total of 87 (42.6%) patients were males, and 117 (57.4%) were females. The first clinical symptoms were as follows: bellyache, 71 (34.8%); abdominal distension, 31 (15.2%); gastrointestinal bleeding, 31 (15.2%); and other digestive symptoms, 43 (21.1%); 28 (13.7%) were found during the physical examination. 175 (85.8%) tumours were distributed in the stomach, 20 (9.8%) in the bowel, and 9 (4.4%) in the non-gastrointestinal tract. The tumour size ranged from 0.4cm to 22.0cm. Tumours with ulcer, haemorrhage, and necrosis were present in 22 (10.8%), 32 (15.7%), and 19 (9.3%) patients, respectively. Ten (4.9%) patients were found to have surrounding invasion during surgery. According to the modified NIH risk assessment, 100 (49.0%) patients were very low risk, 51 (25.0%) were low risk, 21 (10.3%) were intermediate risk, and 32 (15.7%) were high risk.
Clinicopathological features of 204 patients with GISTs.
| No. of patients (%) | |
|---|---|
| Age (y) | |
| ≤59 | 105(51.5) |
| >59 | 99(48.5) |
| Sex | |
| Male | 87(42.6) |
| Female | 117(57.4) |
| Tumour size (cm) | |
| ≤2 | 99(48.5) |
| 2.1-5 | 71(34.8) |
| 5.1-10 | 18(8.8) |
| >10 | 16(7.8) |
| Mitotic index (/50 HPF) | |
| ≤5 | 167(81.9) |
| >5 | 37(18.1) |
| Tumour site | |
| Stomach | 175(85.8) |
| Bowel | 20(9.8) |
| Non-GI tract | 9(4.4) |
| Ki-67 LI | |
| <6% | 148(72.5) |
| ≥6% | 56(27.5) |
| CD117 | |
| Positive | 196(96.1) |
| Negative | 8(3.9) |
| DOG1 | |
| Positive | 195(95.6) |
| Negative | 9(4.4) |
| CD34 | |
| Positive | 189(92.6) |
| Negative | 15(7.4) |
| Ulcer | |
| Yes | 22(10.8) |
| No | 182(89.2) |
| Haemorrhage | |
| Yes | 32(15.7) |
| No | 172(84.3) |
| Necrosis | |
| Yes | 19(9.3) |
| No | 185(90.7) |
| Around invasion | |
| Yes | 10(4.9) |
| No | 194(95.1) |
| NIH risk grade | |
| Very low risk | 100(49.0) |
| Low risk | 51(25.0) |
| Intermediate risk | 21(10.3) |
| High risk | 32(15.7) |
GIST: Gastrointestinal stromal tumours; Ki-67 LI: Ki-67 labelling index; HPF: High-power fields; GI: Gastrointestinal; NIH: National Institutes of Health
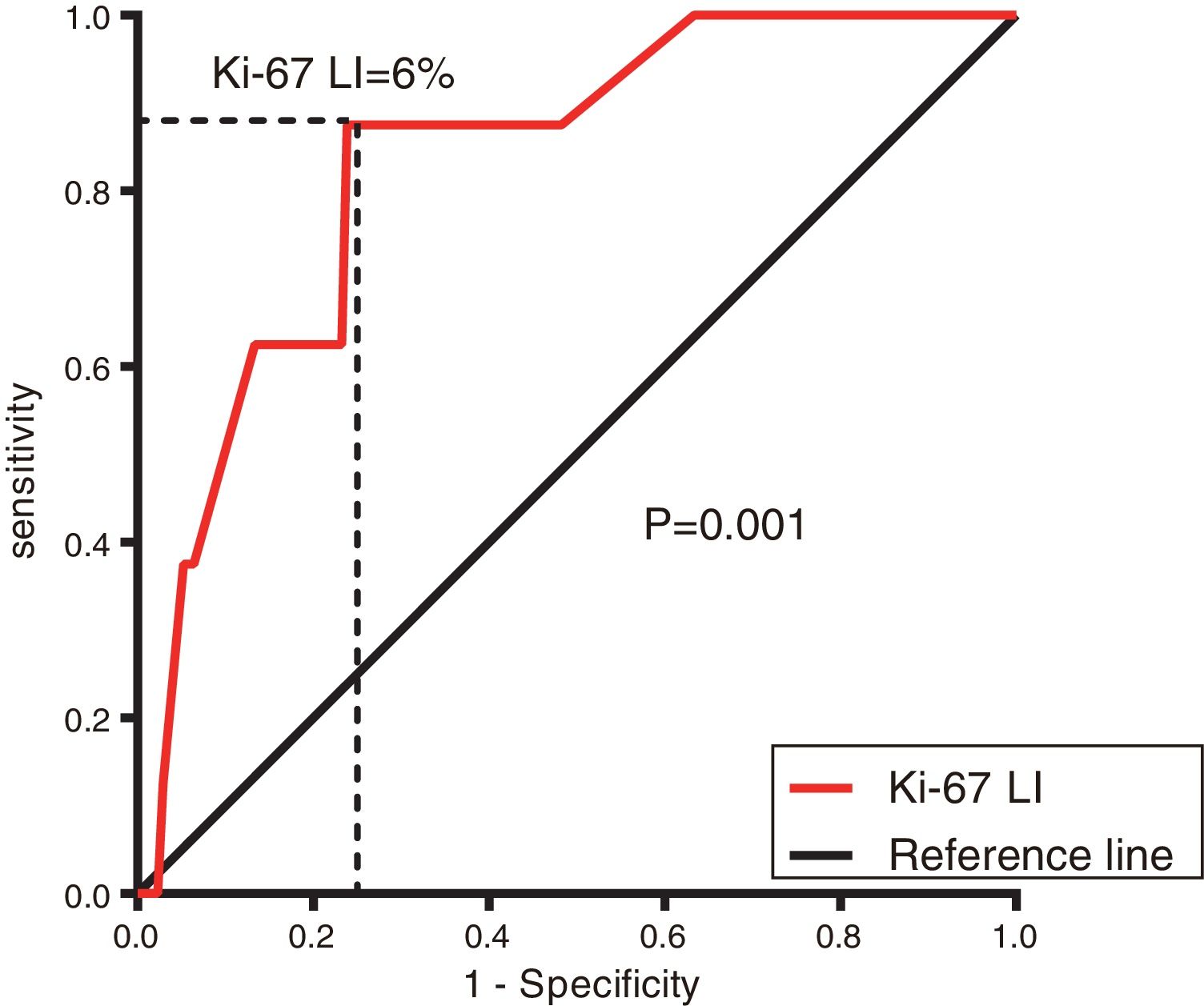
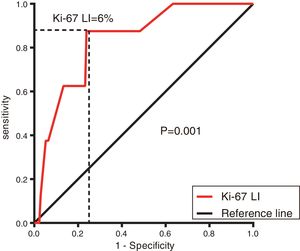
The follow-up period ranged from 0 to 68 months, with a median period of 29 months; 172 (84.3%) patients were alive and progression free, 8 (3.9%) were progressive or had died due to GISTs, and 23(11.3%) were lost to follow-up. The Ki-67 LI ranged from 0 to 60%, with a median of 3%. The optimal cutoff value of the Ki-67 LI by ROC curve analysis was 6% (sensitivity 62.9% and specificity 76.7%) (Figure 1). Based on the cutoff value of the Ki-67 LI, the patients were divided into two groups: Ki-67 LI <6% (148, 72.5%) and Ki-67 LI ≥ 6% (56, 27.5%).
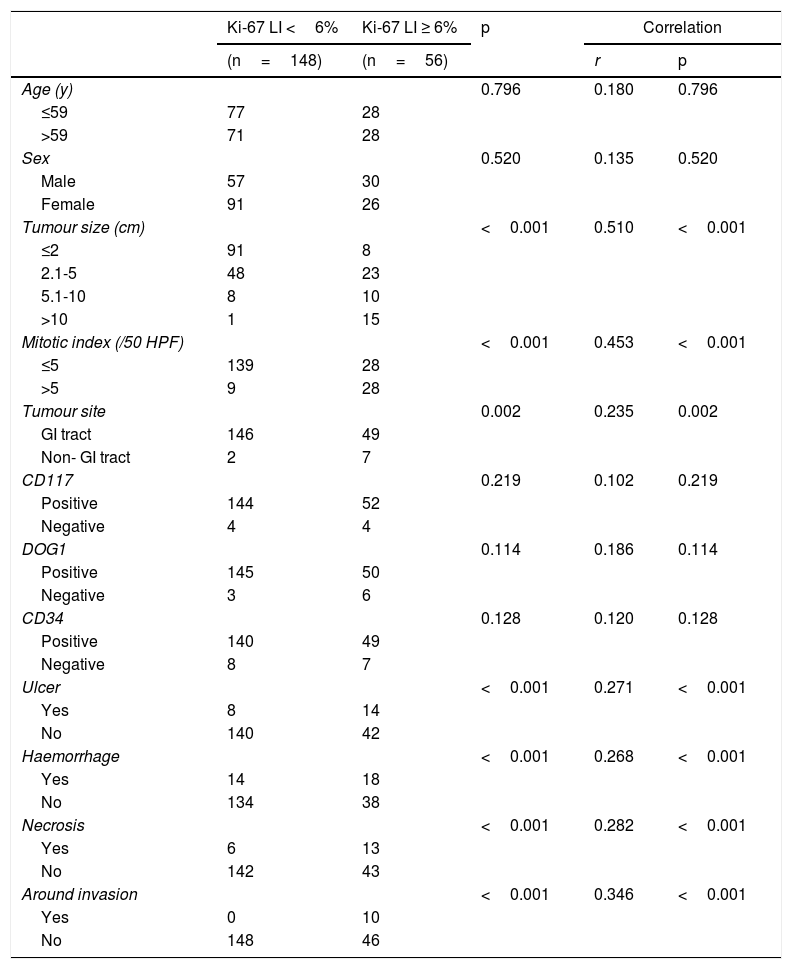
Relationship between the Ki-67 LI and clinicopathological featuresAs shown in Table 3, statistically significant differences in the Ki-67 LI were observed in the following factors: tumour size, mitotic index, tumour site, and tumour with ulcer, haemorrhage, necrosis and around invasion (P <0.05). These factors and the Ki-67 LI were significantly correlated (P <0.05). Ki-67 LI ≥ 6% was related to a larger tumour size, a higher mitotic index, non-gastrointestinal GISTs, and a higher chance of having tumour with ulcer, haemorrhage, necrosis and surrounding infiltration. There was no significant difference or correlation between the Ki-67 LI and age, sex or CD117-, DOG1- and CD34- positive rates (P> 0.05).
Relationship between the Ki-67 LI and clinicopathological features.
| Ki-67 LI <6% | Ki-67 LI ≥ 6% | p | Correlation | ||
|---|---|---|---|---|---|
| (n=148) | (n=56) | r | p | ||
| Age (y) | 0.796 | 0.180 | 0.796 | ||
| ≤59 | 77 | 28 | |||
| >59 | 71 | 28 | |||
| Sex | 0.520 | 0.135 | 0.520 | ||
| Male | 57 | 30 | |||
| Female | 91 | 26 | |||
| Tumour size (cm) | <0.001 | 0.510 | <0.001 | ||
| ≤2 | 91 | 8 | |||
| 2.1-5 | 48 | 23 | |||
| 5.1-10 | 8 | 10 | |||
| >10 | 1 | 15 | |||
| Mitotic index (/50 HPF) | <0.001 | 0.453 | <0.001 | ||
| ≤5 | 139 | 28 | |||
| >5 | 9 | 28 | |||
| Tumour site | 0.002 | 0.235 | 0.002 | ||
| GI tract | 146 | 49 | |||
| Non- GI tract | 2 | 7 | |||
| CD117 | 0.219 | 0.102 | 0.219 | ||
| Positive | 144 | 52 | |||
| Negative | 4 | 4 | |||
| DOG1 | 0.114 | 0.186 | 0.114 | ||
| Positive | 145 | 50 | |||
| Negative | 3 | 6 | |||
| CD34 | 0.128 | 0.120 | 0.128 | ||
| Positive | 140 | 49 | |||
| Negative | 8 | 7 | |||
| Ulcer | <0.001 | 0.271 | <0.001 | ||
| Yes | 8 | 14 | |||
| No | 140 | 42 | |||
| Haemorrhage | <0.001 | 0.268 | <0.001 | ||
| Yes | 14 | 18 | |||
| No | 134 | 38 | |||
| Necrosis | <0.001 | 0.282 | <0.001 | ||
| Yes | 6 | 13 | |||
| No | 142 | 43 | |||
| Around invasion | <0.001 | 0.346 | <0.001 | ||
| Yes | 0 | 10 | |||
| No | 148 | 46 | |||
Ki-67 LI: Ki-67 labelling index; HPF: High-power fields; GI: Gastrointestinal
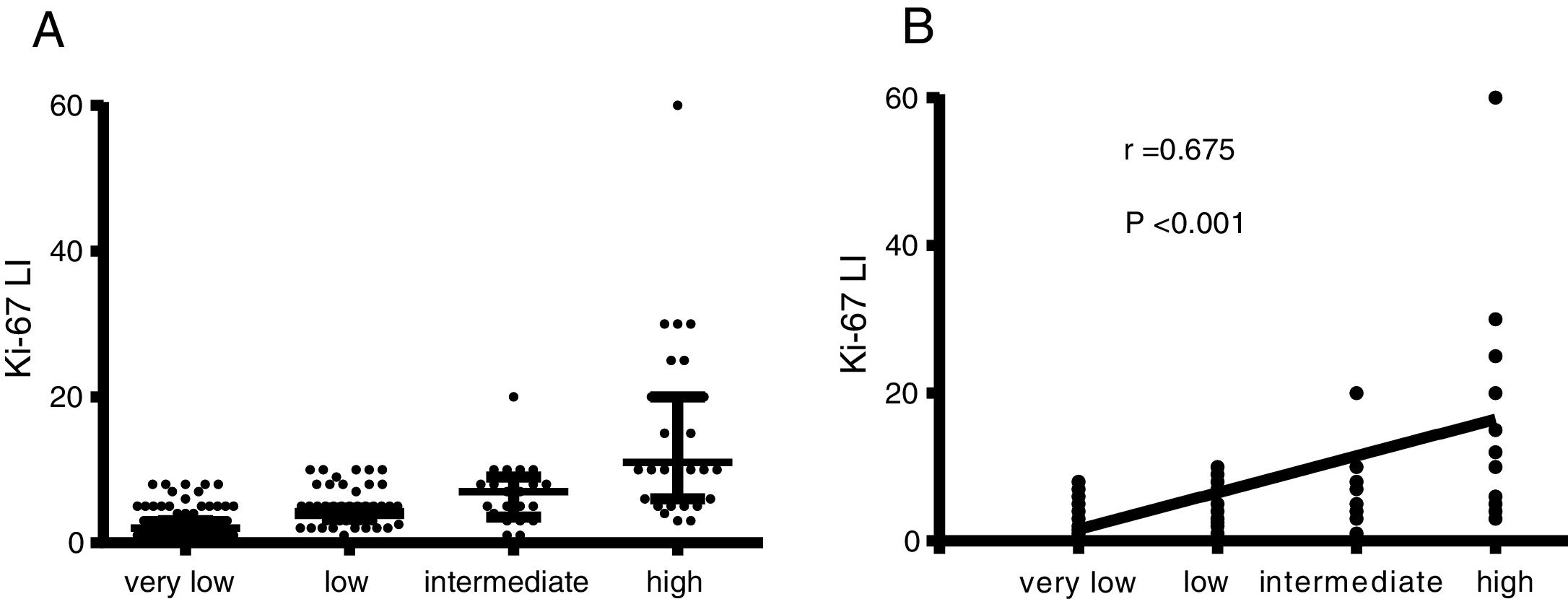
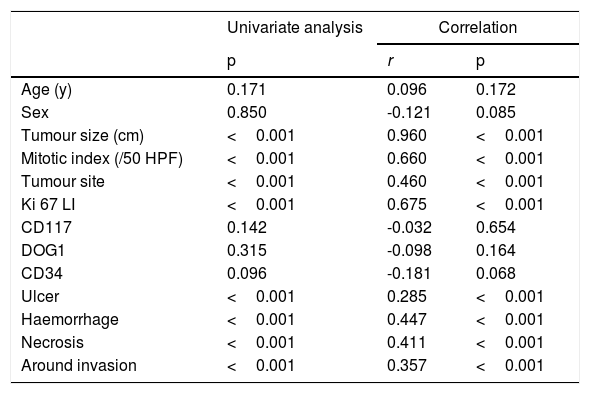
The distribution of the Ki-67 LI in different risk classifications of GISTs is shown in Figure 2. Statistically significant differences in the Ki-67 LI, tumour size, mitotic index, tumour site, and tumour with ulcer, haemorrhage, necrosis and surrounding invasion in different risk grades of GISTs (P <0.05) were determined by the univariate analysis (Table 4). The data from the correlation analysis showed that the higher Ki-67 LI, the larger tumour size, the more mitotic index, the non-gastric tumour, and the greater chance of tumour with ulcer, haemorrhage, necrosis, and surrounding infiltration corresponded to a higher risk grade (P <0.05) (Table 4). Logistic regression analysis was performed on the statistically significant variables in the univariate analysis. The results indicated that the Ki-67 LI was an independent indicator of the risk grade of GISTs (odds ratio (OR): 1.322; 95% confidence interval (CI): 1.031-1.696) (P=0.028), along with tumour size, mitotic index, and tumour site (P <0.005) (Table 5).
Relationship between the GISTs risk classification and clinicopathological features.
| Univariate analysis | Correlation | ||
|---|---|---|---|
| p | r | p | |
| Age (y) | 0.171 | 0.096 | 0.172 |
| Sex | 0.850 | -0.121 | 0.085 |
| Tumour size (cm) | <0.001 | 0.960 | <0.001 |
| Mitotic index (/50 HPF) | <0.001 | 0.660 | <0.001 |
| Tumour site | <0.001 | 0.460 | <0.001 |
| Ki 67 LI | <0.001 | 0.675 | <0.001 |
| CD117 | 0.142 | -0.032 | 0.654 |
| DOG1 | 0.315 | -0.098 | 0.164 |
| CD34 | 0.096 | -0.181 | 0.068 |
| Ulcer | <0.001 | 0.285 | <0.001 |
| Haemorrhage | <0.001 | 0.447 | <0.001 |
| Necrosis | <0.001 | 0.411 | <0.001 |
| Around invasion | <0.001 | 0.357 | <0.001 |
GISTs: Gastrointestinal stromal tumors; Ki-67 LI: Ki-67 labelling index; HPF: High-power fields
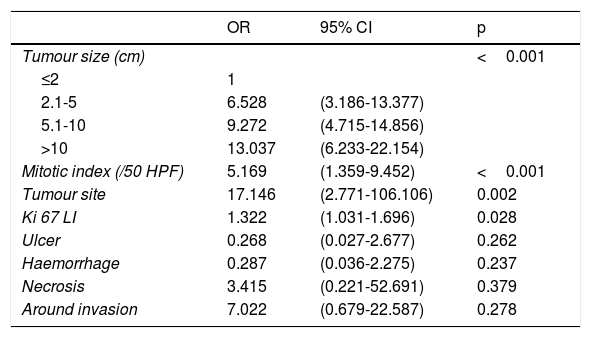
Logistic regression analysis for statistical variables in the GISTs risk classification.
| OR | 95% CI | p | |
|---|---|---|---|
| Tumour size (cm) | <0.001 | ||
| ≤2 | 1 | ||
| 2.1-5 | 6.528 | (3.186-13.377) | |
| 5.1-10 | 9.272 | (4.715-14.856) | |
| >10 | 13.037 | (6.233-22.154) | |
| Mitotic index (/50 HPF) | 5.169 | (1.359-9.452) | <0.001 |
| Tumour site | 17.146 | (2.771-106.106) | 0.002 |
| Ki 67 LI | 1.322 | (1.031-1.696) | 0.028 |
| Ulcer | 0.268 | (0.027-2.677) | 0.262 |
| Haemorrhage | 0.287 | (0.036-2.275) | 0.237 |
| Necrosis | 3.415 | (0.221-52.691) | 0.379 |
| Around invasion | 7.022 | (0.679-22.587) | 0.278 |
OR: Odds ratio; CI: Confidence interval; GISTs: Gastrointestinal stromal tumors; Ki-67 LI: Ki-67 labelling index; HPF: High-power fields
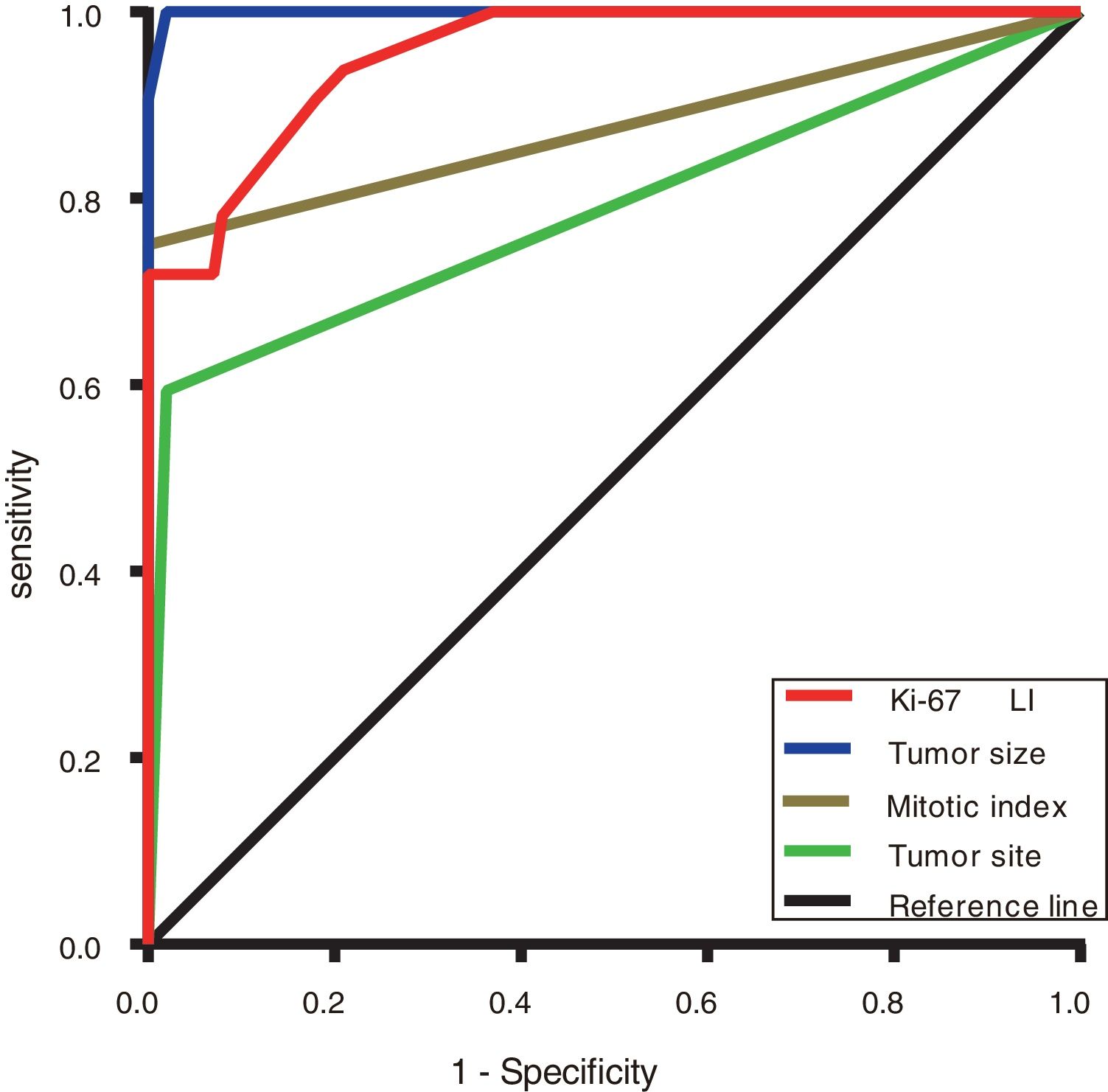
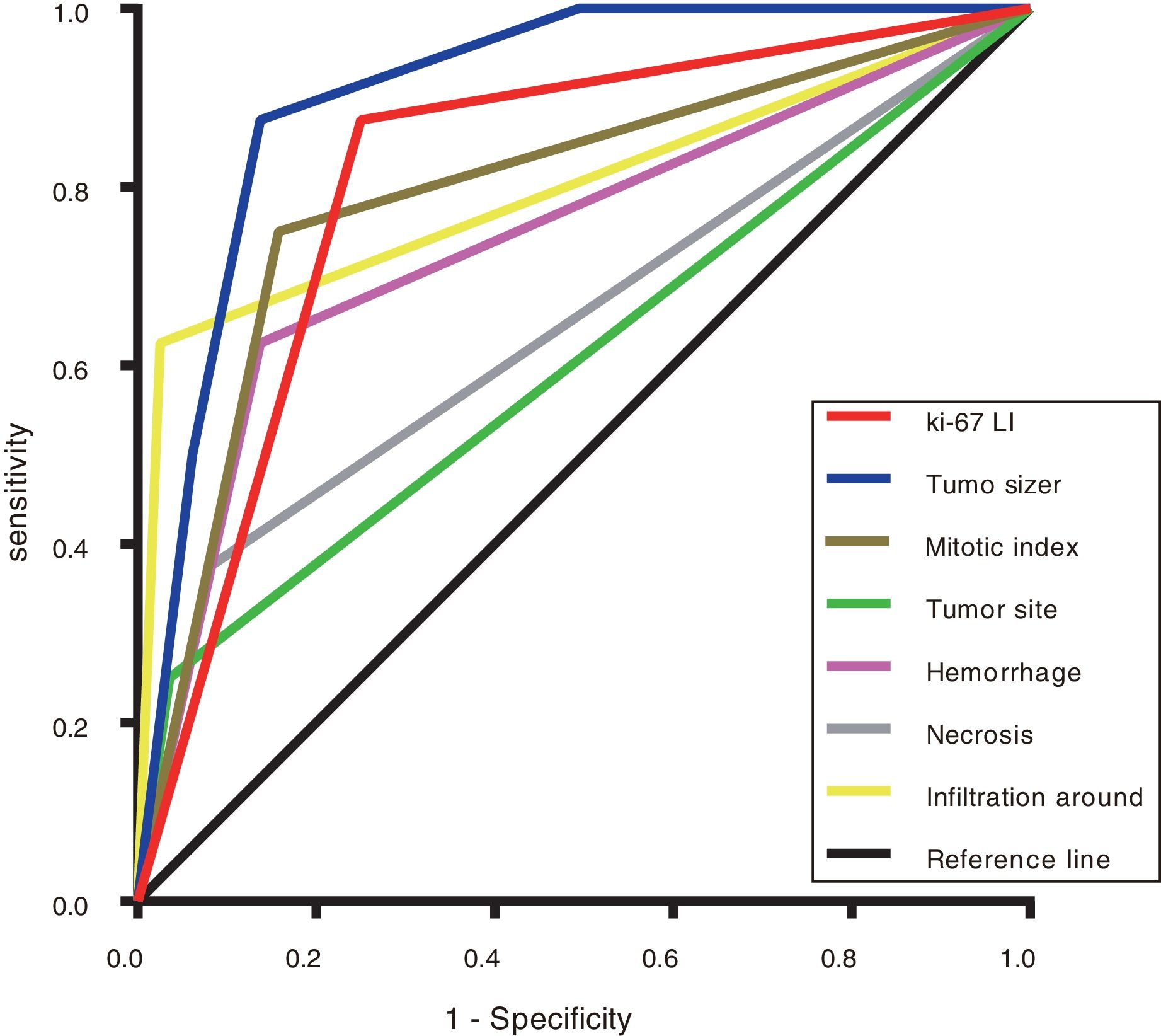
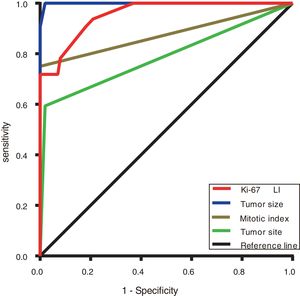
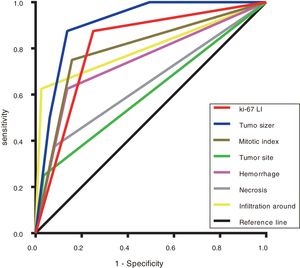
The ROC curve was used to evaluate the discrimination ability of the Ki-67 LI, tumour size, mitotic index, and tumour site in the GISTs risk classification. The area under the curve (AUC) of the Ki-67 LI (0.906) (P <0.001) was smaller than only tumour size (0.973) but larger than that of the mitotic index (0.837) and tumour site (0.768) (Figure 3 and Table 6).
Areas under the ROC curves of evaluating the GISTs risk classification.
| AUC | 95% CI | p | |
|---|---|---|---|
| Tumour size | 0.973 | (0.946-1.000) | <0.001 |
| Ki-67 LI | 0.906 | (0.852-0.961) | <0.001 |
| Mitotic index | 0.837 | (0.745-0.929) | <0.001 |
| Tumour site | 0.768 | (0.660-0.875) | <0.001 |
AUC: Area under the curve; CI: Confidence interval; GISTs: Gastrointestinal stromal tumors; Ki-67 LI: Ki-67 labelling index
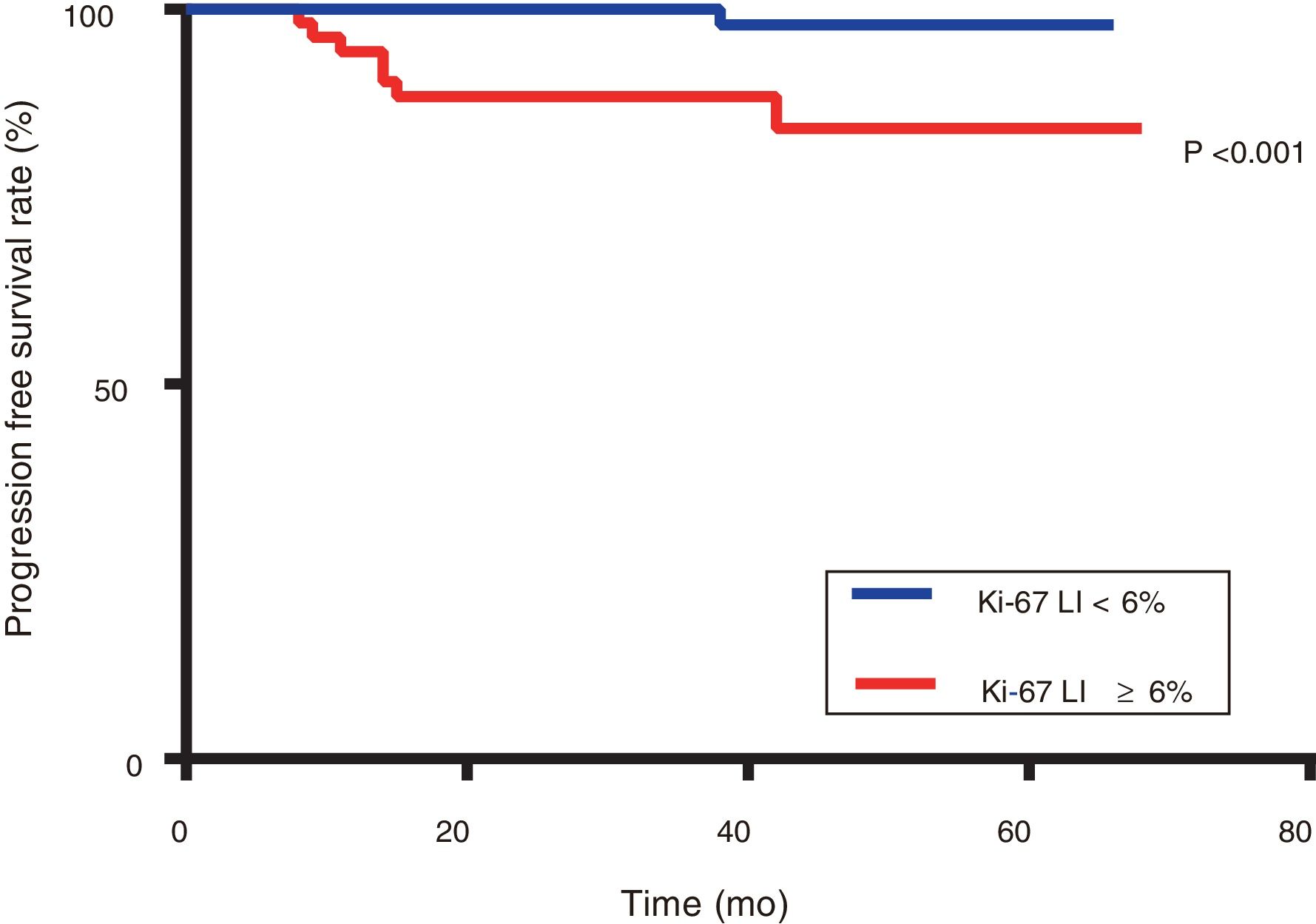
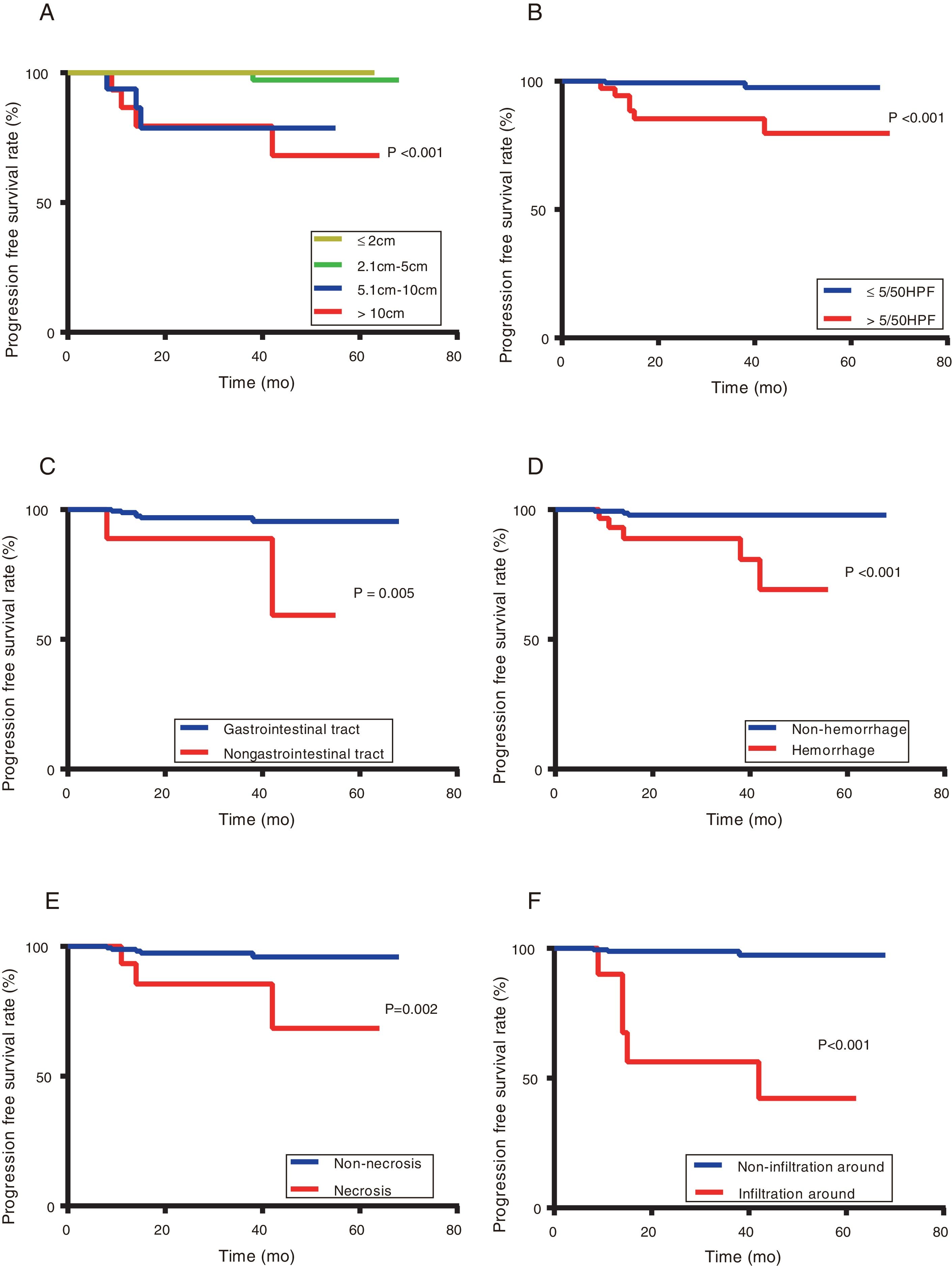
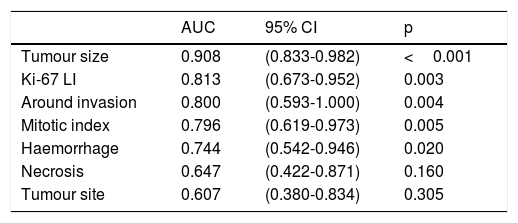
Patients with Ki-67 Li ≥ 6% had significantly poorer PFS than those with Ki-67 Li <6% (87.5% versus 99.3%, respectively; P <0.001) (Figure 4).To explore the relationship between clinicopathological features and prognosis, a survival analysis was performed, which showed that the Ki-67 LI, tumour size, mitotic index, tumour site and tumour with haemorrhage, necrosis, and around invasion were all associated with PFS (P <0.05) (Figures 4 and 5). However, sex, age, tumour with ulcer, and positive rates of CD117, DOG1, and CD34 were not significantly different regarding PFS (P> 0.05). Multivariate Cox regression analyses illustrated that neither the Ki-67 LI nor the modified NIH classification components were independent prognosis indicators for PFS (P> 0.05) (Table 7).
PFS based on tumour size (A), mitotic index (B), tumour site (C), tumour with haemorrhage (D), necrosis (E), and around invasion (F).
Patients with a larger tumour size, higher mitotic index, non-gastrointestinal GISTs, tumour with haemorrhage, necrosis and around invasion had a poorer prognosis (P <0.05).
Univariate and multivariate Cox analyses of prognostic factors for PFS.
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | |
| Age (y) | 0.062 | |||
| ≤59 | 1 | |||
| >59 | 0.135 (0.017-1.101) | |||
| Sex | 0.631 | |||
| Male | 1 | |||
| Female | 1.421 (0.339-5.956) | |||
| Tumour size (cm) | <0.001 | 0.633 | ||
| ≤2 | 1 | 1 | ||
| 2.1-5 | 2.024 (0.669-4.696) | 1.193 (0.578-2.798) | ||
| 5.1-10 | 3.447 (0.722-7.703) | 7.356 (1.575-25.112) | ||
| >10 | 3.817 (0.822-9.201) | 6.822 (0.886-16.245) | ||
| Mitotic index (/50 HPF) | <0.001 | 0.553 | ||
| ≤5 | 1 | 1 | ||
| >5 | 11.868 (2.391-58.908) | 1.936 (0.219-17.156) | ||
| Tumour site | 0.005 | 0.354 | ||
| GI tract | 1 | 1 | ||
| Non- GI tract | 7.177 (1.445-35.643) | 0.292 (0.022-3.946) | ||
| Ki-67 LI | <0.001 | 0.915 | ||
| <6% | 1 | 1 | ||
| ≥6% | 16.416 (2.018-133.546) | 0.842 (0.035-20.022) | ||
| CD117 | 0.718 | |||
| Negative | 1 | |||
| Positive | 21.281 (0.522-33.917) | |||
| DOG1 | 0.633 | |||
| Negative | 1 | |||
| Positive | 22.381 (0.578-78.363) | |||
| CD34 | 0.293 | |||
| Negative | 1 | |||
| Positive | 0.323 (0.040-2.647) | |||
| Ulcer | 0.491 | |||
| No | 1 | |||
| Yes | 0.040 (0.001-3.718) | |||
| Haemorrhage | <0.001 | 0.204 | ||
| No | 1 | 1 | ||
| Yes | 9.990 (2.381-41.919) | 3.119 (0.539-18.040) | ||
| Necrosis | 0.002 | 0.889 | ||
| No | 1 | 1 | ||
| Yes | 6.765 (1.615-28.337) | 1.140 (0.180-7.246) | ||
| Around invasion | <0.001 | 0.033 | ||
| No | 1 | 1 | ||
| Yes | 30.555 (7.281-128.221) | 7.568 (1.174-48.786) | ||
HR: Hazard ratio; CI: Confidence interval; PFS: Progression-free survival; HPF: High-power fields; GI: Gastrointestinal; Ki-67 LI: Ki-67 labelling index
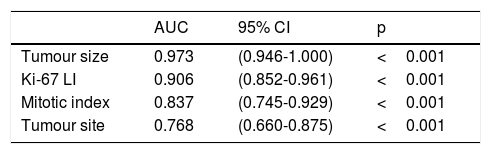
Statistically significant factors identified in the above survival analysis were used to predict postoperative PFS in patients with GISTs via the AUC calculated from ROC curve. Only tumour size had a higher AUC (0.908) than the Ki-67 LI (0.813) (P=0.003), while the AUC of the Ki-67 LI was higher than that of the mitotic index (0.796), tumour site (0.607), and tumour with haemorrhage (0.744), necrosis (0.647) and around invasion (0.800) (Figure 6 and Table 8).
Areas under the ROC curves of predicting the prognosis of GISTs.
| AUC | 95% CI | p | |
|---|---|---|---|
| Tumour size | 0.908 | (0.833-0.982) | <0.001 |
| Ki-67 LI | 0.813 | (0.673-0.952) | 0.003 |
| Around invasion | 0.800 | (0.593-1.000) | 0.004 |
| Mitotic index | 0.796 | (0.619-0.973) | 0.005 |
| Haemorrhage | 0.744 | (0.542-0.946) | 0.020 |
| Necrosis | 0.647 | (0.422-0.871) | 0.160 |
| Tumour site | 0.607 | (0.380-0.834) | 0.305 |
AUC: Area under the curve; CI: Confidence interval; GISTs: Gastrointestinal stromal tumors; Ki-67 LI: Ki-67 labelling index
GISTs originate from gastrointestinal primordial pluripotent stem cells and are caused by an imbalance in cell proliferation and apoptosis. GISTs are potentially malignant tumours, and approximately 10% to 30% can progress to malignancy.14 The digestive tract is the most common site of GISTs. When GISTs occur outside the gastrointestinal tract, they are called extra-GISTs (E-GISTs). E-GISTs usually have the same morphological features, immunohistochemistry and molecular characteristics as traditional GISTs but are more aggressive than gastrointestinal GISTs.15,16 In this study, we found that E-GISTs were associated with a higher risk and lower PFS than gastrointestinal GISTs, which further confirmed previous findings.
In contrast to other mesenchymal tumours, GISTs have been referred to as unique solid tumours in recent decades. They are rare compared with other digestive tract tumours, which limits improvements in their risk classification and prognostic indicators. Radical resection is still the major method used to treat local primary GISTs, but tumour recurrence and metastasis are very common after surgery, especially in high risk patients.1 For aggressive tumours, a precise risk category and effective prognostic factors are critical to help identify high risk patients and develop effective treatment plans. However, in the current modified NIH risk assessment standard, only limited factors, including tumour size, mitotic index, tumour site and tumour rupture, are used to evaluate the invasiveness of GISTs. Hence, more precise research is needed to explore indicators that can assess the risk grade and prognosis of GISTs.
Ki-67, a DNA binding nucleoprotein related to cell mitosis, has been used as a reliable indicator for evaluating the risk classification and prognosis of breast cancer and neuroendocrine tumours.17–19 An increasing number of studies have suggested that high Ki-67 LI is associated with a poor prognosis in many types of malignancies, but the clinical value of the Ki-67 LI in GISTs remains undefined.
A study has shown that the Ki-67 LI is associated with tumour site and is higher in E-GISTs than in gastrointestinal GISTs.20 This conclusion is consistent with our findings. Our results showed that the Ki-67 LI was positively correlated with tumour size and mitotic index, which further supports previous studies.21,22 In addition, our study found that in patients in the same risk category, tumours with pathological histological changes such as ulcer, haemorrhage, necrosis and peripheral invasion were concentrated in the group with high Ki-67 LI and positively correlated with the Ki-67 LI, suggesting that the Ki-67 LI is significantly parallel to the biological behaviours of tumour progression and invasiveness. For GISTs patients with the same risk grade, those with higher Ki-67 LI are prone to a poor prognosis. It was previously reported that high Ki-67 expression indicated a significantly worse prognosis in patients with a high risk grade than in those with low Ki-67 expression,23 which supports our results. Although CD117, DOG1 and CD34 are specific indicators for the diagnosis of GISTs, our study found that the expression of CD117, DOG1, CD34 was not related to the Ki-67 LI, and it could not effectively judge the invasiveness of GISTs or predict the clinical outcomes of patients.
Our study demonstrated that the Ki-67 LI is an independent factor of GISTs risk classification and exhibits high diagnostic value for the invasiveness of GISTs; the higher the Ki-67 LI is, the higher the risk grade of the GISTs. The increased expression of Ki-67 indicates more active cell proliferation, faster growth, worse differentiation, and stronger tumour invasiveness. All of the above findings point out that the Ki-67 LI can be used as a supplement to the NIH risk classification for defining the risk of individual tumours. We recommend that the risk level can be adjusted appropriately by Ki-67 LI, while the risk grade is performed according to the NIH risk classification, in order to avoid missing an effective adjuvant treatment or overtreatment.
The univariate analysis revealed that the Ki-67 LI was associated with prognosis in our study; however, multivariate Cox regression analyses demonstrated that the Ki-67 LI was not an independent predictor of GISTs prognosis. Similarly, some studies have reported that Ki-67 expression is prognostically irrelevant in overall survival.24,25 However, Liu X et al.,23,25 found that the Ki-67 LI is a promising predictor of overall survival in GISTs postoperation. The prognostic significance of the Ki-67 LI was maintained when the stratification analysis was performed based on the NIH risk classification, tumour size, mitotic index, tumour site and histological morphology. Our data also revealed that the Ki-67 LI had a large AUC to predict PFS, which indicates that the Ki-67 LI has a tendency to effectively predict the prognosis of postoperative patients, which may add important prognostic information to patients based on the GISTs risk classification.
The Ki-67 LI stratified analysis showed that patients with Ki-67 LI ≥ 6% had significantly lower PFS than patients with Ki-67 LI <6%, suggesting that GISTs patients with Ki-67 LI ≥ 6% are most likely to experience recurrence and metastasis after the operation. These findings indicate that GISTs with high Ki-67 LI are prone to strong invasiveness and have great chances of metastasis and recurrence. Therefore, it may be necessary to develop individualized follow-up strategies for patients with high Ki-67 LI to extend PFS.
Moreover, our results showed that the Ki-67 LI was superior to the mitotic index in predicting risk grade and prognosis. Both indicators reflect the cell proliferation status, but whether the Ki-67 LI can replace the mitotic index is always controversial. Some scholars believe that Ki-67 is expressed in all phases of the cell cycle except for G0 phase, while the mitotic index is expressed only in M phase; therefore, the Ki-67 LI can represent cell proliferation more comprehensively. Furthermore, the repeatability of the Ki-67 LI count is better than that of the mitotic index because when measuring the mitotic index under a microscope, the results may be inaccurate due to various factors, such as the uneven distribution of the mitotic index and differences among enumerators. Therefore, some researchers believe that the Ki-67 LI can replace the mitotic index.22,26 However, a study has noted that the predictive value of the Ki-67 LI in GISTs is weaker than that of the mitotic index. Only when the mitotic index is less than 50 high-power fields can the Ki-67 LI be used as a supplementary indicator to assess the invasiveness of GISTs.27 We believe that more research is needed to determine whether the Ki-67 LI can replace the mitotic index.
In conclusion, the Ki-67 LI is significantly associated with the progression and poor clinical outcomes of GISTs. It has appreciated value to predict the malignant potential and prognosis of GISTs and can be used as a supplement to the modified NIH classification for establishing individualized risk stratification and predicting prognosis. For tumours with high Ki-67 expression, postoperative follow-up should be strengthened.
FundingThis work was supported by the Health Commission of Hubei Province [grant number WJ2019H082].
Conflict of InterestThe authors declare that they have no conflict of interest.