Perivascular epithelioid cell tumors (PEComas) are mesenchymal neoplasms characterized histologically by the proliferation of perivascular epithelioid cells (PEC) and immunohistochemically by expressing melanocytic markers (HBM-45 and Melan-A) and muscular markers (actin and desmin).1 The cells in PEComas are arranged around the blood vessels and appear to form part of its wall, often infiltrating the smooth muscle of the small and medium-sized vessels. Furthermore, in histology the cells have small, round or oval nuclei, occasionally with focal nuclear atypia and eosinophilic cytoplasm. The group known as PEComas includes angiomyolipomas, lymphangioleiomyomatosis, clear cell “sugar” tumors of the lung as well as other rarer types of tumor, among which are falciform ligament clear cell tumors and abdominopelvic sarcoma of perivascular epithelial cells typically associated with tuberous sclerosis, with which it shares genetic anomalies.2 The term PEComa is used to refer to all lesions of this type that are not angiomyolipomas, lymphangioleiomyomatosis or clear cell “sugar” tumors of the lung.
Their behavioral spectrum ranges from benign to clearly malignant, with proposed histological criteria to assess the potential malignancy (mitotic index, vascular proliferation, necrosis). The differential diagnosis may include carcinomas, smooth muscle tumors, other clear cell neoplasms and adipose tissue tumors. PEComas constitute a genetically diverse group that includes neoplasms that harbor TFE3 gene rearrangements with TSC2 mutations, indicating alternative tumorigenic pathways. Recent advances in the treatment of malignant PEComas are related to a greater understanding of the specific genetic changes and their effects on metabolic pathways which are susceptible to specific interventions.
We present the case of a patient with a solid lesion in the body of the pancreas with puncture by endoscopic ultrasound (EUS) with atypia on whom a corporocaudal pancreatectomy with laparoscopic splenectomy was performed. Accordingly, we performed a review of the literature with cases of pancreatic PEComa published to date.
A 50-year-old female with no medical-surgical history of interest was presented. She was referred for a surgical consultation after discovery of a lesion in the body of the pancreas measuring 13mm detected in a study of anemia and abdominal pain. The following complementary tests were provided: EUS: lesion measuring 13mm in body of pancreas closely related to the main pancreatic duct, cytology (puncture) revealed the presence of atypical cells without clear origin. Both the MRI and CT scans revealed a lesion in the pancreatic body measuring 15mm with discretely hypervascular dynamic behavior in the arterial phase that becomes isodense in the portal phase, compatible with primary tumor of pancreatic origin. Due to the suspicion of a malignant lesion, surgical intervention was elected, performing a corporocaudal pancreatectomy with laparoscopic splenectomy. The patient was discharged on the second day after surgery with no associated complications. The anatomopathological study revealed a nodular proliferative mesenchymal neoplasm delimited by a thin fibrous capsule measuring 16mm made up of clear cells, ample cytoplasms, pleomorphic nuclei and occasional fusiform cells without observing necrosis or lymphovascular involvement compatible with a perivascular epithelioid cell tumor (PEComa) of the pancreas. One mitosis per 10 high-power fields was counted. Immunohistochemical techniques show expression of smooth muscle actin, HMB45 and MelanA, with absence of inhibin, CD10, synaptophysin and chromogranin, CEA, HepPar1, CK 7 and 20, or RCC. The mean Ki67 proliferative index is below 1%. At one and a half years after surgery, the patient is asymptomatic and disease-free.
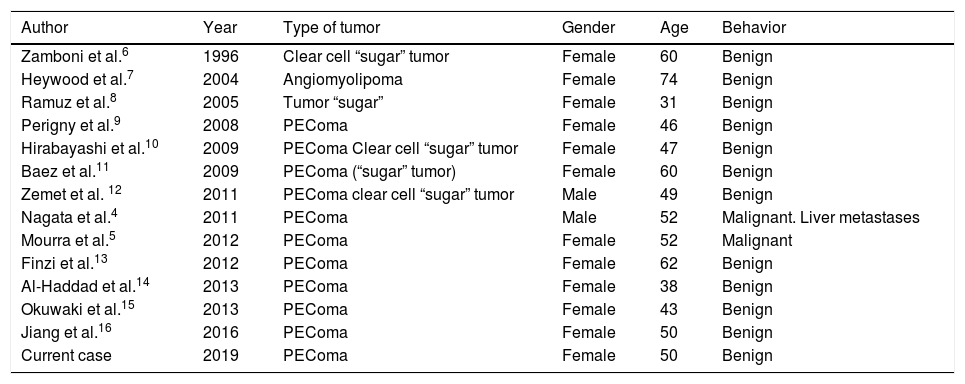
The World Health Organization defines PEComas as a group of mesenchymal neoplasms with histological and immunohistological characteristics typical of PECs.3 Pancreatic PEComa is an extraordinarily rare entity with only 13 cases published in the literature to date and up to the time of this work (Table 1). Although benign behavior is the norm, there are two cases reported with malignant behavior, one with liver metastasis of a metachronous nature 27 months after surgery on the primary tumor and another a lesion measuring 6cm in the head of the pancreas with vascular involvement and abundant necrosis in the histological study.4,5 There is a strong predisposition in females (12 of the 14 patients reported, including the present case). Although PEComas are usually associated with genetic mutations with tuberous sclerosis, none of the cases reported with pancreatic location, including our case, have presented this association. Surgery is currently the only treatment option for both benign and malignant cases. The data to define malignancy are in relation to the presence of factors of poor prognosis in the histological study, such as a high mitotic index or pattern of infiltrative vascular growth with presence of necrosis.4 The final diagnosis is made with histological and immunohistochemical criteria from the resection specimen. With preoperative imaging, no test (EUS, MRI, CT) offers characteristic data that would allow for a differential diagnosis with other malignant pancreatic lesions to be made (ductal adenocarcinoma). In our case, the presence of atypia in the histological study of the EUS-guided fine-needle aspiration, together with the appearance of the hypovascular lesion in both MRI and CT scans made surgical resection necessary. The laparoscopic approach enabled rapid recovery with an early discharge after two days with no associated complications. Being a rare tumor and mostly being a benign disease (12 of the 14 cases reported), no adjuvant oncological therapies have been developed.
Description of the 14 published cases of pancreatic PEComa.
| Author | Year | Type of tumor | Gender | Age | Behavior |
|---|---|---|---|---|---|
| Zamboni et al.6 | 1996 | Clear cell “sugar” tumor | Female | 60 | Benign |
| Heywood et al.7 | 2004 | Angiomyolipoma | Female | 74 | Benign |
| Ramuz et al.8 | 2005 | Tumor “sugar” | Female | 31 | Benign |
| Perigny et al.9 | 2008 | PEComa | Female | 46 | Benign |
| Hirabayashi et al.10 | 2009 | PEComa Clear cell “sugar” tumor | Female | 47 | Benign |
| Baez et al.11 | 2009 | PEComa (“sugar” tumor) | Female | 60 | Benign |
| Zemet et al. 12 | 2011 | PEComa clear cell “sugar” tumor | Male | 49 | Benign |
| Nagata et al.4 | 2011 | PEComa | Male | 52 | Malignant. Liver metastases |
| Mourra et al.5 | 2012 | PEComa | Female | 52 | Malignant |
| Finzi et al.13 | 2012 | PEComa | Female | 62 | Benign |
| Al-Haddad et al.14 | 2013 | PEComa | Female | 38 | Benign |
| Okuwaki et al.15 | 2013 | PEComa | Female | 43 | Benign |
| Jiang et al.16 | 2016 | PEComa | Female | 50 | Benign |
| Current case | 2019 | PEComa | Female | 50 | Benign |
In conclusion, the pancreatic PEComa is a rare tumor, with a strong predominance among females in the 4th and 5th decade of life, with a generally benign behavior of difficult differential diagnosis using imaging tests, and for which surgical resection is the treatment of choice. With this case, there are only 14 patients reported in the literature.
Please cite this article as: Colón Rodríguez A, Calleja Kempin J, Quirós Higueras E, Botella ER, Castillo J. Tumour de células epiteliales perivasculares (PECOma) de origen pancreático. Descripción de un caso y revisión de la literatura. Gastroenterol Hepatol. 2020;43:257–259.