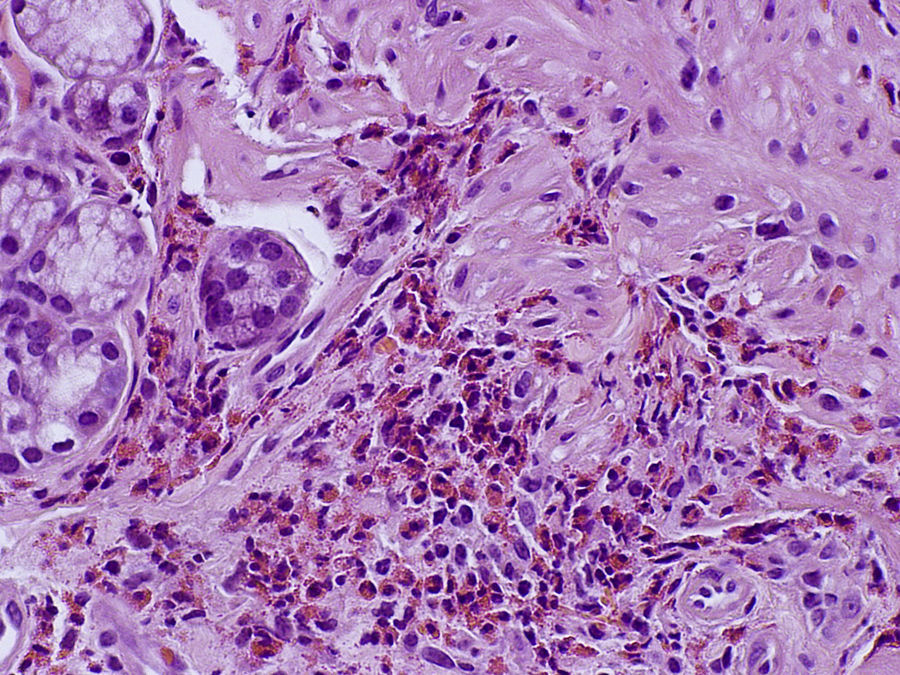
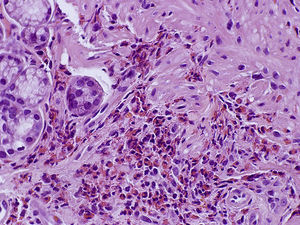
A previously healthy 33-year-old woman presented to the emergency department with a 2-week history of epigastric pain, vomiting, diarrhea and abdominal distention. She had had a non-complicated pregnancy and delivery 7 weeks earlier. The patient denied recent travel, new medication, atopy, allergies, diet changes or ill contact prior to the symptoms. Physical examination showed abdominal distention and shifting dullness. Gynecological examination was normal. Laboratory evaluation revealed an elevated white blood cell count of 14,900μL with 41.7% eosinophils (6.200μL), PCR 1.3mg/dL (normal<1.0mg/dL), hypoproteinemia (5.7g/dL), hypoalbuminemia (3.0g/dL) and an increased IgE level (240KUI/L). Hemoglobin, red blood cell count, coagulation studies, serum electrolytes, creatinine, alpha-1 antitrypsin, immunoglobulins, thyroid and liver function tests were within normal range. Antinuclear and anti-neutrophil cytoplasmatic antibodies were negative. Stool ova and parasites, stool, urine and blood cultures and Toxocara serology were all negative. On abdominal and transvaginal ultrasonography there was a large amount of abdominal and pelvic ascites. A diagnostic paracentesis was performed and revealed an exsudative type of ascites with protein level 4.1g/dL, albumin 2.0g/dL and raised leukocytes (3600μL) but unfortunately cellular differential count was not made. Bacteriological culture and adenosine deaminase were negative. Computed tomography scan showed pyloric antrum, duodenum and jejunum wall thickening and large volume ascites (Fig. 1). Esophagogastroduodenoscopy revealed pyloric enlarged folds and colonoscopy was unremarkable. Duodenal biopsy showed focal fold shortening with eosinophilic infiltration in lamina propria consistent with eosinophilic gastroenteritis (Fig. 2). She was treated with oral prednisolone 40mg daily following a taper scheme. During this period, the patient was under careful surveillance and was always asymptomatic with normal eosinophil count. Four weeks after she stopped glucocorticoid therapy, she returned to the emergency room with abdominal pain, nausea, vomiting and diarrhea. Laboratory data revealed eosinophilia with 3680μL. As a result, oral prednisolone was restarted in the same initial dose. At the end of the second tapering period, on a every other day 5mg dose, she experienced the same symptoms together with a slow increase in eosinophil count. The patient is currently, 4 years after the initial episode, under a 5mg daily-dose, with no symptoms.
Eosinophilic gastroenteritis is an uncommon disorder characterized by eosinophilic infiltration of the gastrointestinal tract. Any area can be affected, from the esophagus to the rectum, in a diffuse or focal form. Clinical manifestations are mainly related with the involvement of the different layers of the digestive wall. Klein et al. classified the disease in three patterns according to specific symptoms: a mucosal form characterized by abdominal pain, nausea, vomiting, diarrhea and protein-losing enteropathy; a muscular form where perforation or obstruction can occur; and a subserosal form where patients present with ascites (the rarest type of presentation). The pathogenesis is still unclear although it may have an allergic component.1 In 1990, Talley et al. suggested the diagnostic criteria that are still in use.2 These includes: the presence of gastrointestinal symptoms, eosinophilic infiltration in biopsy specimens or suggestive imagiologic findings and no evidence of parasitic disease or systemic involvement. The diagnosis may be suspected in the presence of raised peripheral eosinophil count (although some patients have normal counts), gastrointestinal symptoms, imagiologic and endoscopic studies with suggestive appearance though nonspecific (as thickening of the wall), after exclusion of other causes of eosinophilia (such as allergy, parasitic infection, neoplasm or connective tissue disease). The definitive diagnosis is established by the presence of eosinophilic infiltration on biopsies specimens from gastrointestinal tract wall or eosinophilic ascitic fluid in the absence of other causes of eosinophilia. Malabsorption with hypoalbuminemia and elevated total IgE may be present. The knowledge of the disease is limited to case reports and small series and therapeutic management is based in clinical experience.3,4 Systemic glucocorticoid is the main therapy, usually prednisolone in the daily initial dose of 20–40mg for 6–8 weeks, followed by a tapering scheme. Some patients have a complete remission, but many require long term maintenance therapy to prevent relapses. Other drugs (as cromolyn and montelukast) have been used in patients with recurrent or refractory disease, however the lack of trials make its use off-label.3 Long-term outcomes are not well defined.4 The most important complications are malnutrition, intestinal obstruction and perforation and those associated with long term glucocorticoid therapy.
Eosinophilic gastroenteritis in post-partum is an extremely rare condition, with only 5 cases previously reported in the literature.5–9 Of these, three presented with ascites such as seen in our patient. One of the previous cases describe a woman who experienced symptoms suggestive of eosinophilic gastroenteritis after her two labors that occurred 8 years apart.5 In the other 4 cases no relapse was reported.6–9 To our knowledge, this case is the only one reporting a post-partum eosinophilic gastroenteritis with relapse in the same episode. This case raises the possibility of pregnancy acting as a trigger to eosinophilic gastroenteritis.
Conflict of interestThe authors disclose no conflicts.
Informed consentInformed consent was obtained from the patient for the publication of her information and imaging.