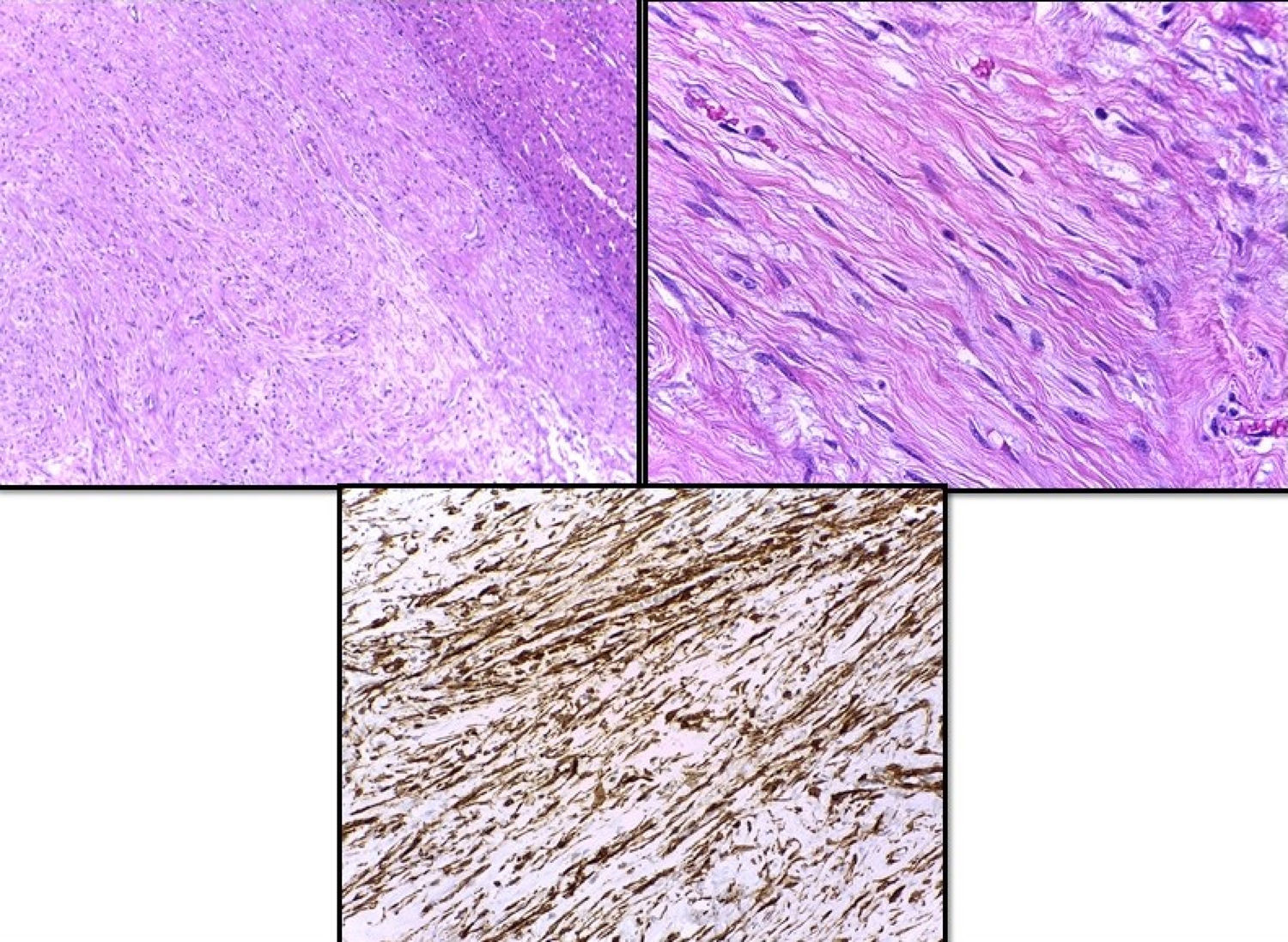
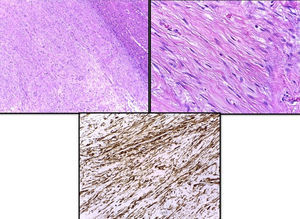
34-Year-old woman with a liver tumour found during a non-specific abdominal pain examination. History of oral contraceptive use and physical examination, with no palpable abdominal mass. The abdominal ultrasound revealed a solid vascularised mass, with no calcifications, measuring 85mm in the IV segment of the left lobe of the liver. The assessment was completed with magnetic resonance imaging (MRI), evidencing an encapsulated lesion with well-defined edges, with T1 homogeneous signal and T2 and T2-STIR hypointense signal, emphasising a small site of greater intensity within the lesion in T2 (Fig. 1). After the injection of the contrast medium, filling of the early and late arterial phases of the tumour occurred, suggestive of hepatic adenoma. The blood tests, including liver function and tumour markers (AFP, CEA and CA 19.9), were normal. In light of the suspected diagnosis of hepatic adenoma and the large size of the tumour, it was decided to perform surgery without conducting a biopsy due to the risk of bleeding. We made a large right subcostal incision, finding a tumour 10cm in diameter in the IVb segment of the liver, with 70% of its surface free. Tumour resection and cholecystectomy were performed. The anatomopathological study confirmed the diagnosis of a smooth muscle neoplasm with a mitotic index below one mitotic figure/10 fields. The immunohistochemical analysis confirmed positivity for Ki-67 below 1% and positive nuclear staining for oestrogen and progesterone receptors (Fig. 2). After the histological result, a pelvic ultrasound was performed to rule out uterine fibroids, as well as an abdominal computerised axial tomography (CT scan) to rule out gastrointestinal stromal tumour (GIST).
Leiomyoma is a benign smooth muscle mesenchymal tumour of uncertain malignant potential, which tends to manifest in the genitourinary system and the gastrointestinal tract.1,2 However, it may also arise in the muscularis mucosae of the gastrointestinal tract or in the tunica media of the blood vessels, meaning that it could manifest in any organ or tissue of the human body.3 Primary hepatic leiomyomas (PHLs) are rare tumours that predominantly affect girls and women, with reported cases in both children and adults alike.1 Only 36 cases have been published to date in the scientific literature. The aetiology is not fully understood, although immunosuppression has been described as a causal factor. One possible explanation for this is the susceptibility of these patients to new malignancies due to the impaired immune system of the host and the resulting development of tumours.2 However, immunosuppression alone does not explain the pathogenesis of these tumours as they also occur in immunocompetent patients. As a result, it is hypothesised that it may be associated with Epstein–Barr virus (EBV) infection based on the theory of virus-induced oncogenesis, as it has been reported that EBV may be involved in the pathogenesis of smooth muscle tumours.2
The clinical presentation of PHL is similar to other hepatic malignancies. The most common symptom is abdominal pain, whilst on rare occasions they may manifest as a palpable abdominal mass or with abdominal discomfort, dyspepsia and liver failure.
A diagnostic study of a liver tumour should include blood and imaging tests. If a definitive diagnosis cannot be established, a liver biopsy may be performed for confirmation. In PHL, tumour markers are generally negative. Imaging tests cannot always be used for diagnostic purposes as there are no typical radiological findings. Nevertheless, a CT scan may reveal hypervascular lesions with enhancement during the arterial and portal phases with no evidence of washout during the late phases, while the MRI may evidence T1-hypointense lesions and T2-hyperintense lesions with non-homogeneous contrast uptake. Because PHL is so rare, a definitive diagnosis is not usually established, often requiring a liver biopsy to be performed to confirm the diagnosis. However, given the clinical suspicion of hepatic adenoma and the size of the tumour in our case, we decided to resect the tumour to establish the diagnosis and treatment and to minimise the risk of bleeding.
To consider hepatic leiomyoma to be a primary tumour, Hawkins et al.4 proposed the following diagnostic criteria: the tumour must be made up of leiomyocytes with no evidence of leiomyoma at other intra-abdominal sites, such as the uterus and the gastrointestinal tract. For confirmation, a comprehensive preoperative examination must be performed. However, given the rarity of these lesions, PHL is almost always diagnosed after anatomopathological study. As such, imaging tests should be conducted after surgery to rule out leiomyoma at other sites, as occurred in our case.
There are no definitive histological criteria to differentiate between benign and malignant smooth muscle tumours of the gastrointestinal tract. Documented metastatic disease is the only way to diagnose malignancy,4 and it is believed that the potential malignancy of benign leiomyomas increases with tumour size.
Liver resection confirming the presence of negative margins is the treatment of choice, and has become a relatively standardised and safe procedure. Operative mortality of less than 5% has been reported.2 Laparotomy is the classic approach, but laparoscopic surgery may also be performed safely, as reported by Perini et al.5 for the first time. The laparoscopic approach allows safe oncological margins to be maintained and avoids the complications that may arise with laparotomy, such as pain, infection of incisional hernias, which are particularly relevant complications in immunosuppressed patients.5 Although dependent on the presence of metastasis and patients’ immunodeficiency, the prognosis of these patients seems to be excellent.
Please cite this article as: Blas Laina JL, González Ruiz Y, Gonzalvo González E, Sanz Moncasi MP, Rodríguez Borobia A. Leiomioma hepático primario: una rara causa de tumoración hepática. Gastroenterol Hepatol. 2017;40:617–619.