We report the case of a 33-year-old female patient who had presented two years previously with haemorrhagic diarrhoea and purpuric marks on her legs at a different institution. She was initially treated with plasmapheresis and steroid therapy with a good response. She was monitored as an outpatient on a regular basis. Two years after her initial clinical presentation, she was admitted to our institution to evaluate new purpuric marks on her legs, with no additional symptoms. Initial examination revealed serum platelets less than 5000μL. She was started on plasmapheresis and steroid therapy with a good response.
A week later, the patient suffered an episode of sudden thoracic pain and dyspnoea with haemoptysis. Her chest X-ray showed bilateral infiltration that was interpreted as TRALI (transfusion related acute lung injury); she was treated with oxygen therapy. During her treatment the patient developed acute abdominal symptoms indicative of severe peritonitis, potentially due to cecal perforation, and required emergency surgery. The presumptive diagnosis was that of steroid induced colitis with cecal perforation. The patient underwent a right hemicolectomy surgery followed subsequently by a second emergency surgery due to wound dehiscence.
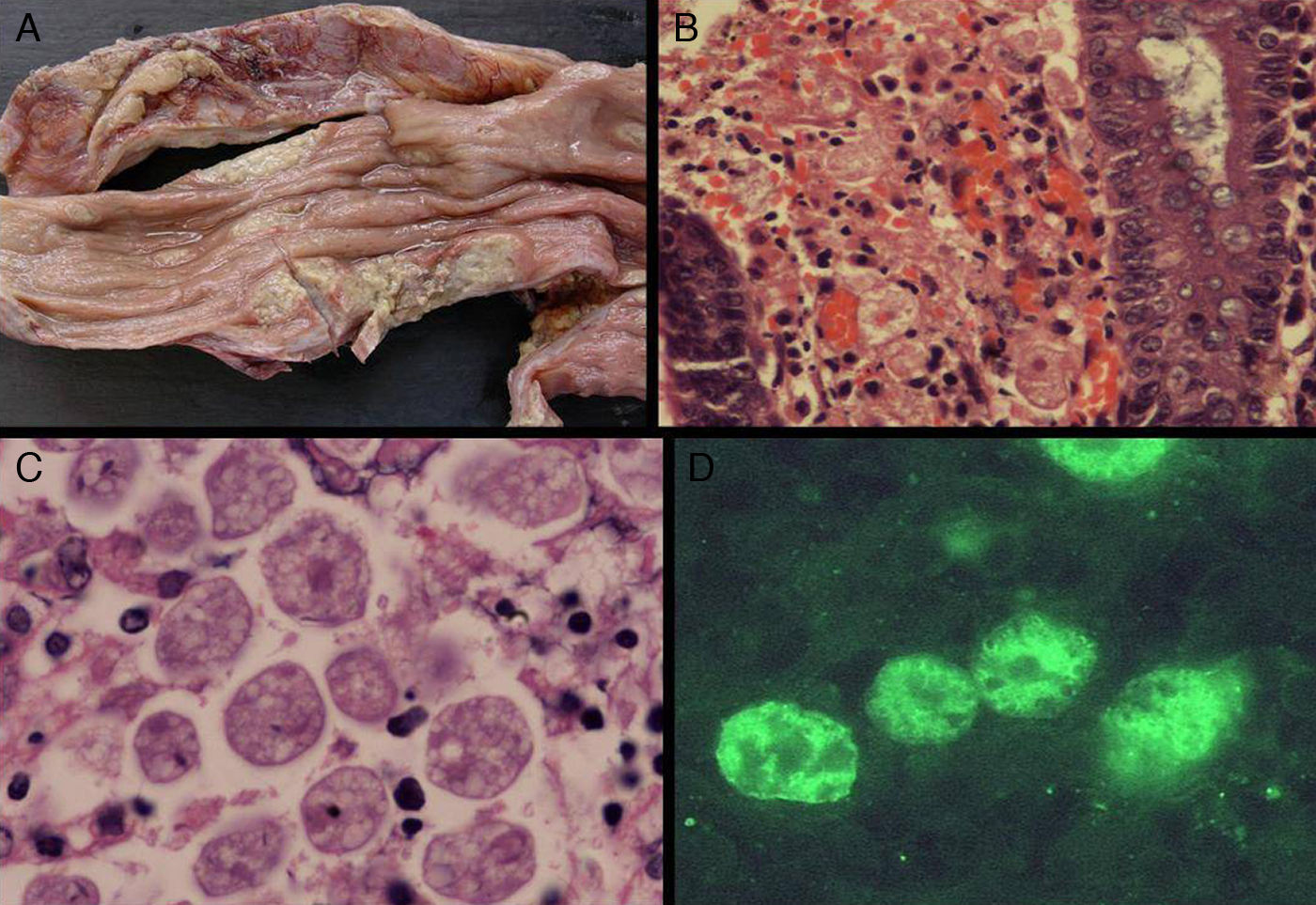
A right hemicolectomy specimen was received at our Pathology Department. Upon opening of the specimen, multiple ulcers were revealed, some covered by fibrinopurulent exudate, ranging from 0.5 to 4cm. An area of transmural perforation at 3.5cm from the ileocecal valve was also observed (Fig. 1A).
Right hemicolectomy specimen showing ulcers covered by an amorphous grey exudate (A) Multiple trophozoites penetrating the lamina propria. (B) Spherical bodies with a single nucleus, surrounded by a thin membrane with a prominent karyosome. (C) Immunofluorescence test using antibody specific for Entamoeba histolytica (D).
Microscopic examination of specimen revealed the presence of superficial and deep ulcers associated with prominent acute and chronic inflammation. Throughout the wall, we identified numerous spherical bodies with a single nucleus containing a small, often eccentric nucleolus (Fig. 1B, 1C). The nucleus was surrounded by a thin membrane. We also identified some spherical bodies containing four small nuclei. These findings were compatible with trophozoites and cysts of Entamoeba histolytica.
A representative paraffin block was sent to CDC, Atlanta, USA. The diagnosis was confirmed as E. histolytica after specific immunofluorescence testing (Fig. 1D). The final diagnosis was that of amoebic colitis caused by E. histolytica.
The patient was re-questioned after full recovery about international travelling. She revealed that her partner used to travel to the Far East and North Africa at least twice a year. A stool specimen from her partner was subsequently tested and E. histolytica parasites were detected.
Our patient received treatment with metronidazole and recovered gradually. After fourteen months of follow up, no evidence of TTP was found. Her partner was treated with paromomycin.
Amoebic colitis is one of the most common parasitic diseases worldwide. However, our case exemplifies a few uncommon features. First of all, our patient had an unusual presentation, with the simultaneous occurrence of TTP and colitis. Additionally, she had an unusually long course for this disease (two years) as well as lack of a recent international travel history, although her partner did travel to endemic areas frequently. The amoebic infection in her partner, without active disease, but with positive stool cultures, demonstrates the importance of individual susceptibility in these cases.1 It is crucial to consider this entity when one confronts a case of a patient with bloody stools, who has travelled recently to an endemic area or with a history of foreign travel of partner or family member. The pathologist has to learn to recognize the amoebic forms, since it is relatively easy to confuse them with macrophages in heavily inflamed areas.1–3 The diagnosis in cases of unsuspected amoebic colitis is often delayed and is frequently only made histologically in specimens obtained during biopsy or autopsy.4
Our patient suffered an episode of bloody stools two years before her most recent admission. The simultaneous occurrence of dramatic purpuric lesions at the time made this the primary presenting symptom, and the focus in her case was on haematological disease as the primary presumptive cause. Although the simultaneous appearance of these symptoms, purpura and bloody diarrhoea, could be the coincidental occurrence of two separate diseases, it is also possible that the amoebic infection is responsible for the TTP. The fact that her purpuric lesions disappeared after specific treatment for E. histolytica makes this a reasonable option. We have not seen any published report in the literature that refers to this association. Our patient will need longer follow up in order to confirm this link, which could be immunologically mediated.
We want to emphasize the importance of an early and accurate diagnosis of amoebiasis in these cases, since it is crucial for planning surgical procedures. The risk of suture breakdown in tissue containing amoeba is high, and anastomosis should be avoided, regardless of the extent of the resected segment. Radical surgery for fulminant amoebic colitis leads to extremely high mortality; however, resective surgery is mandatory if a patient develops massive faecal peritonitis.5
This is a very interesting and challenging case, since it is the first described case of a refractory TTP associated with colitis that resolved after treatment for E. histolytica infection. Amoebic infection needs to be considered as a potential cause of TTP when this disease presents with haemorrhagic diarrhoea. The pathogenesis of this association, if confirmed, will require additional studies.
Conflict of interestsDr. Visvesvara works for the Division of Parasitic Diseases, National Center for Zoonotic, Vector-Borne and Enteric Diseases, Center for Disease Control and Prevention, Atlanta, USA.
The authors thank Rama Sriram for expert technical assistance.