To understand the current state of endoscopic ultrasonography (EUS) in Spain.
MethodsDescriptive analysis from a national survey with 11 questions: 10 related to technique and 1 to the training and experience of the endoscopists.
ResultsSixty endoscopists from 48 of the 97 (49.5%) hospitals that perform EUS in Spain responded to the survey. A total of 28,678 procedures (20,311 diagnostic, 7446 with puncture and 921 therapeutic) were recorded over the course of one year. Approximately 64% of the hospitals perform between 300 and 999 tests per year. All have radial and sectorial echoendoscopes, with a median of 2 (2–8) scopes. For cytological diagnosis, the 22-gauge needle is the most commonly used (98%) and, for histological diagnosis, the Procore (72%). The study of the pancreas and bile duct is the most common indication for diagnostic EUS (60%), followed by the staging of digestive tract neoplasms (20%). Approximately 72% of the hospitals perform on-site cytopathology evaluations and sedation is administered in equal parts by both endoscopists and anaesthetists. In terms of experience, 45% of echoendoscopists perform fewer than 300 annual exams and the median training duration is 6 months (0.5–36).
ConclusionsEUS is adequately implemented in Spain and good equipment is available. However, it is necessary to establish a standardised EUS training programme since the one undertaken by many echoendoscopists could prove insufficient according to the standards established by Scientific Societies.
Conocer el estado actual de la ultrasonografía endoscópica (USE) en España.
MétodosAnálisis descriptivo a partir de una encuesta nacional con 11 preguntas: 10 relativas a la técnica y una a la formación y experiencia de los ecoendoscopistas.
ResultadosContestaron 60 endoscopistas correspondientes a 48 de los 97 (49,5%) hospitales que realizan USE en España. Se contabilizaron en un año 28.678 exploraciones (20.311 diagnósticas, 7.446 con punción y 921 terapéuticas). Un 64% de los hospitales realiza entre 300 y 999 pruebas por año. Todos los centros disponen de ecoendoscopio radial y sectorial, con una mediana de 2 por hospital (2-8). La aguja de citología que más se usa es la de 22 gauges (98%) y de histología la Procore (72%). El estudio del páncreas y la vía biliar es la indicación más frecuente de USE diagnóstica (60%), seguido de la estadificación de neoplasias del tubo digestivo (20%). El 72% de los hospitales dispone de un citopatólogo en la sala y la sedación es administrada a partes iguales por los endoscopistas y anestesistas. En cuanto a la experiencia, el 45% de los ecoendoscopistas realizan menos de 300 exploraciones anuales y la mediana de tiempo de formación es de 6meses (0,5-36).
ConclusionesLa USE está adecuadamente implementada en España y se dispone de buen equipamiento. Sin embargo, es necesario establecer un programa estandarizado de formación en USE, ya que la de muchos ecoendoscopistas podría ser insuficiente según los estándares establecidos por las Sociedades Científicas.
Since its introduction more than 30 years ago, endoscopic ultrasonography (EUS) has become a fundamental diagnostic and therapeutic tool in the management of numerous disorders both inside and outside the gastrointestinal tract. The addition of fine needle aspiration (EUS-FNA) has enabled cytological diagnosis of all lesions located within a radius of 8cm of the gastrointestinal tract and it is now the method of choice due to its low morbidity rates and high degree of efficacy.1 Moreover, the very recent development of therapeutic procedures guided by EUS in the bile duct and pancreas has awakened the interest of numerous endoscopists and has expanded the indications of EUS.2,3
Despite the increasing availability of EUS in Spain, there are no data on the indications for which the technique is most commonly performed, on the therapeutic procedures carried out at each hospital, or on the type of material the different endoscopists use. We also have little idea of how many endoscopists perform EUS in each hospital or how they were trained. These data are important to determine whether or not the number of scans performed individually is sufficient to maintain a good level of experience. In a survey conducted among residents in advanced endoscopy in the United States, it was found that the training could be inadequate due to the small number of cases overall and, as a consequence, the small number of procedures performed by each person.4
The aim of this study is to find out the current status of EUS in Spain.
Patients and methodsIn September 2017, we sent a survey by email to all endoscopists who perform EUS in Spain. We used the email addresses from the Grupo Español de Ecoendoscopia Digestiva [Spanish Gastrointestinal Endoscopic Ultrasonography Group] database. In addition, an active attempt was made to obtain the addresses of the endoscopists who were not listed. After two rounds of emails, we contacted by telephone all the hospitals where the endoscopists who did not respond to the survey worked, inviting them to respond before the end of November 2017.
The survey consisted of 10 questions referring to the technique and one question about the training of endoscopists (Appendix). The data obtained were entered into an IBM SPSS Statistics 23 database for further analysis. Quantitative variables were expressed as median and range, and qualitative variables as percentages.
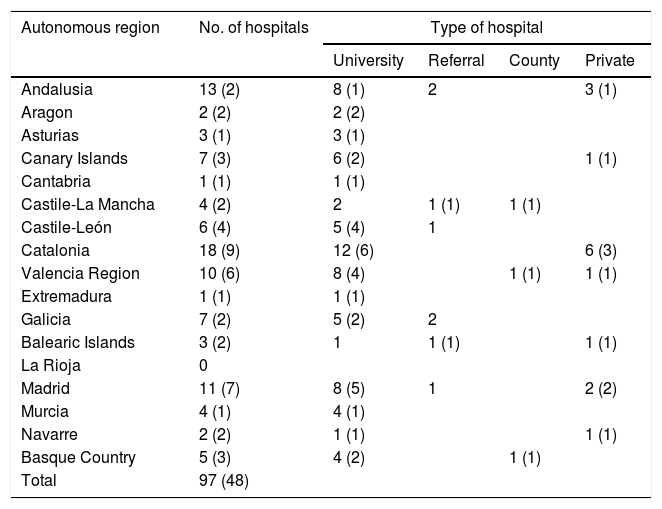
ResultsHospitalsDuring the two-month period, a total of 60 endoscopists from 48 of the 97 (49.5%) Spanish hospitals in which EUS was performed answered the survey, with a great variation in participation in the different autonomous regions. Table 1 shows the number and types of hospitals distributed by autonomous region. It should be noted that the majority of centres where EUS is used are university hospitals (80%). Taking into account that the Spanish population in 2016 was 46.56 million, we infer that EUS is available in 2.1 hospitals per million people.
Number and types of hospitals distributed by autonomous region in which EUS is used. The number in brackets corresponds to the number of hospitals whose endoscopists answered the survey.
| Autonomous region | No. of hospitals | Type of hospital | |||
|---|---|---|---|---|---|
| University | Referral | County | Private | ||
| Andalusia | 13 (2) | 8 (1) | 2 | 3 (1) | |
| Aragon | 2 (2) | 2 (2) | |||
| Asturias | 3 (1) | 3 (1) | |||
| Canary Islands | 7 (3) | 6 (2) | 1 (1) | ||
| Cantabria | 1 (1) | 1 (1) | |||
| Castile-La Mancha | 4 (2) | 2 | 1 (1) | 1 (1) | |
| Castile-León | 6 (4) | 5 (4) | 1 | ||
| Catalonia | 18 (9) | 12 (6) | 6 (3) | ||
| Valencia Region | 10 (6) | 8 (4) | 1 (1) | 1 (1) | |
| Extremadura | 1 (1) | 1 (1) | |||
| Galicia | 7 (2) | 5 (2) | 2 | ||
| Balearic Islands | 3 (2) | 1 | 1 (1) | 1 (1) | |
| La Rioja | 0 | ||||
| Madrid | 11 (7) | 8 (5) | 1 | 2 (2) | |
| Murcia | 4 (1) | 4 (1) | |||
| Navarre | 2 (2) | 1 (1) | 1 (1) | ||
| Basque Country | 5 (3) | 4 (2) | 1 (1) | ||
| Total | 97 (48) | ||||
With the data from the survey, we can say that EUS was introduced in Spain in 1996. EUS-FNA was first used in 1999 and the first cases of therapeutic EUS were in 2002. Rioja is the only autonomous region that does not currently have EUS.
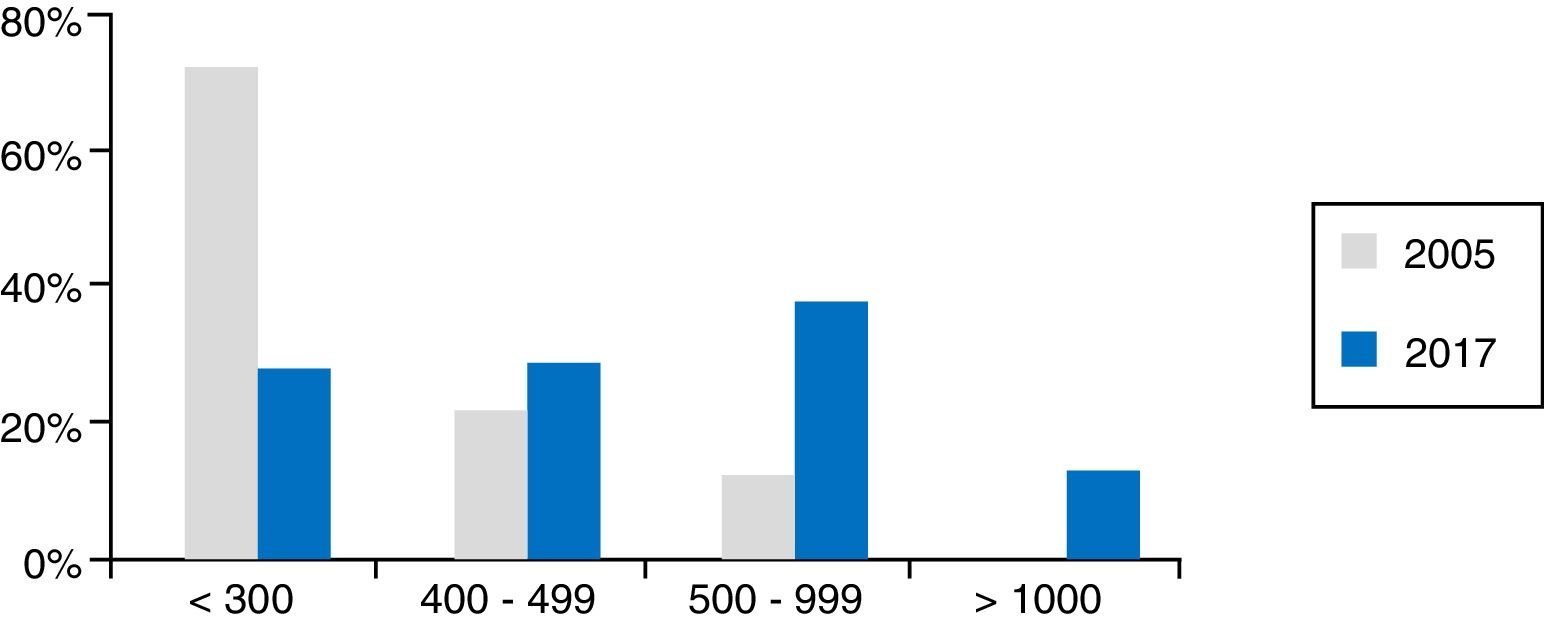
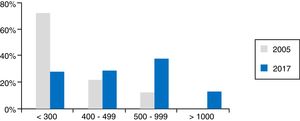
Technical dataThe total number of EUS scans performed in one year in Spain was 28,678 (20,311 diagnostic, 7446 EUS-FNA and 921 therapeutic EUS). This represents a median per hospital per year of 450 (35–2396), with 300 diagnostic (18–1994), 105 EUS-FNA (2–667) and 11 therapeutic (0–130). In fact, 25.5% of hospitals perform fewer than 300 tests a year and 64% perform from 300 to 999; 46% of hospitals actually perform 500 or more. Fig. 1 shows these activity data compared to those from 2005 presented at the meeting of the European Group for EUS (EGEUS).
Data for activity in 2017 according to the survey results. The grey columns represent the activity in 2005 according to data presented at the EGEUS (European Group for Endoscopic UltraSonography) meeting (Paris, 2005). As can be seen, activity has increased; there has been a huge reduction in the number of hospitals performing fewer than 300 scans a year.
The median of endoscopists/hospital who perform EUS is 2 (1–4). Therefore, calculating the number of scans performed by each endoscopist, slightly less than half (45%) perform <300, 25% from 300 to 499, 24% from 500 to 999 and 6% >1000.
In terms of equipment, all the centres presently have a radial and sector echoendoscope, with a median of 2 (2–8). The most used brand is Olympus (58.7%), followed by Pentax (32.6%) and Fujifilm (8.7%). Only one hospital has equipment of more than one brand and only one uses miniprobes (specifically, 30 intraductal miniprobes/year), although in the past 24% had them.
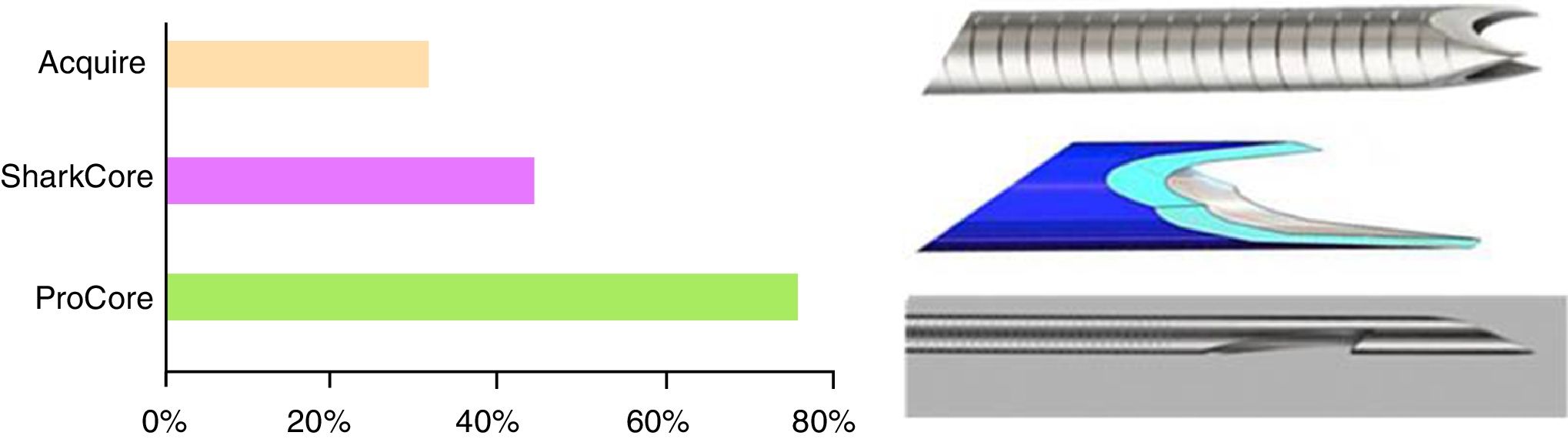
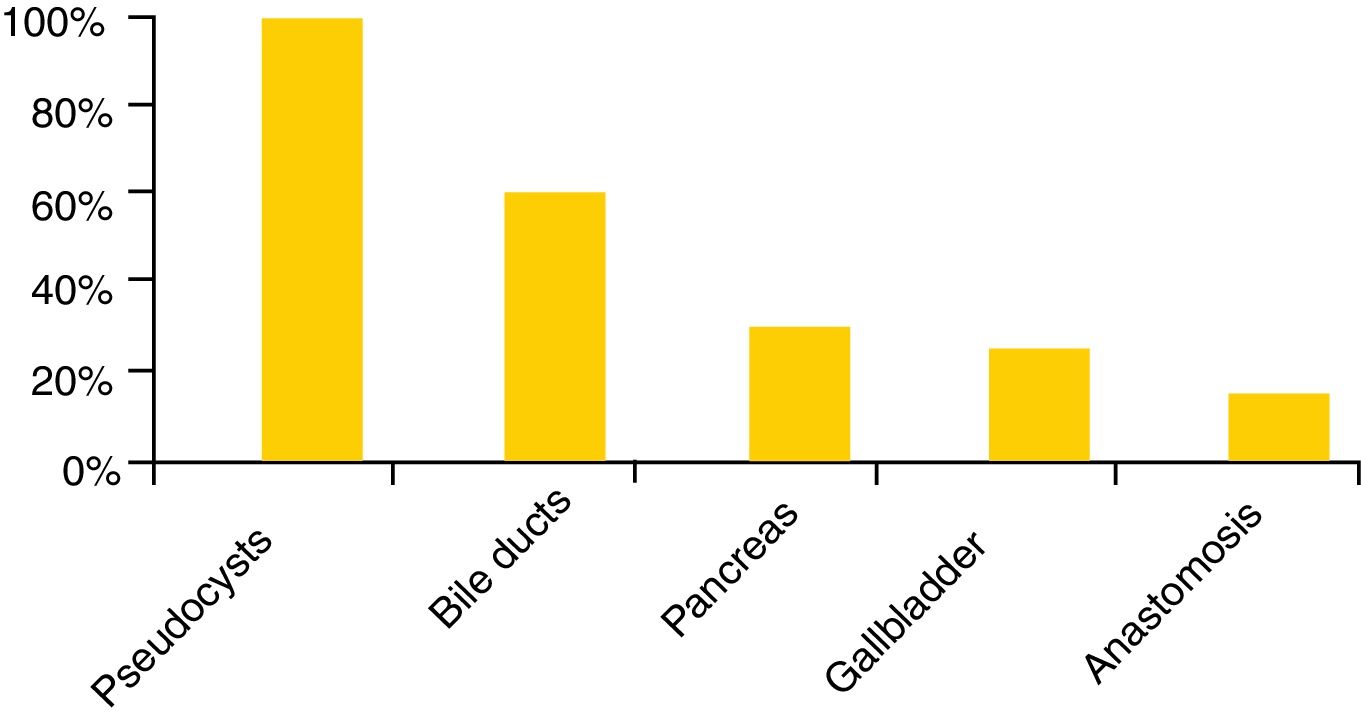
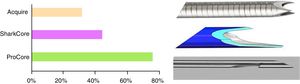
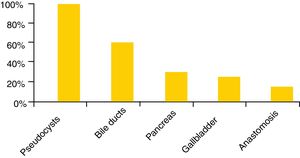
The puncture needles available are very varied, with the 22 gauge needle being the most widely used (98%), although 87% and 83% of the centres also have 19 and 25 gauge needles, respectively. Cook Medical and Boston Scientific are the most popular brands (83% and 67% respectively), followed by Olympus (37%) and Medi-Globe (15%). Spanish hospitals not only have cytology needles but also histological needles (EchoTip ProCore®, Cook Medical, 72%; SharkCore®, Medtronic, 41%; and Acquire®, Boston Scientific, 28%) (Fig. 2). In terms of the types of investigations, EUS and EUS-FNA are performed in all hospitals and in 85% there is also some type of therapeutic EUS, the most common being drainage of pseudocysts (93%), and the least common, the creation of gastrointestinal anastomoses (9%) (Fig. 3).
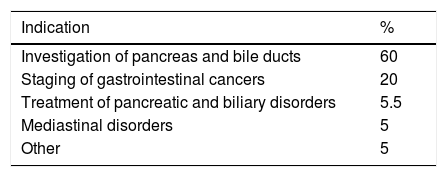
The indications for diagnostic EUS are set out in Table 2, with the study of the pancreas and the bile duct being the most common (a median of 60% of all indications), followed by the staging of gastrointestinal cancers (20%).
Rectal EUS is only available in 63% of Spanish hospitals. In the remaining 37%, surgeons perform this type of investigation.
Some 72% of hospitals have a cytopathologist/cytotechnologist in the ultrasound room to assess the sample obtained in situ (Rapid On Site Evaluation [ROSE]) during the procedure.
As far as sedation is concerned, this is administered by the endoscopist in 42% of the centres, by the anaesthetist in another 42% and, in 16%, it is given by one or the other depending on the characteristics of the patient and anaesthetist availability.
Information on the experience and training of the endoscopistAlmost 3/4 (72.7%) of endoscopists have more than 5 years of experience in EUS and EUS-FNA and, understandably because it was introduced more recently, 60% began performing therapeutic EUS 5 years ago. The median number of years of experience is 10 (1–21) for EUS, 10 (1–18) for EUS-FNA and 8 (1–15) for therapeutic EUS.
The median length of training is 6 months (0.5–36). While 45% have trained for over 6 months, 30% have less than 3 months of training. All the endoscopists have spent time training at other centres with experience in EUS, and only one stated that they were self-taught.
DiscussionThis is the first survey to be published which informs us about the current status of EUS practice in Spain; overall, it reflects widespread implementation of the technique, as it is available in most tertiary hospitals. The total number of EUS procedures performed is 28,678/year, representing 616 scans per million population. When comparing our data with those of two surveys conducted in the United States and Belgium, published in 20165 and 2005,6 respectively, more investigations are carried out each year in Spain than in the United States (5.89/million population) but fewer than in Belgium (1111/million population). These differences may be explained, at least partly, by the different way the health service is organised in the case of the United States and the important and long tradition of EUS practice in French-speaking countries, although that last statement should be verified with more recent data than those we were working with. Our activity is also greater than that reported in Asia, where less than 50% of hospitals perform more than 300 EUS/year.7 In our case, we should point out that in three hospitals fewer than 100 examinations are performed each year and, in one of these, there were only 35. As is the case in the United States, Asia and the rest of Europe, in Spain, EUS is performed mainly in university hospitals.
At present, all Spanish centres have both types of ultrasound endoscopes (radial and sector) and EUS-FNA represents 26% of all investigations, while in the United States it is only 15% of the total.5 One possible explanation could be the large differences in the costs of procedures in the two countries and the fact that health insurance is not universal in the United States. The number of EUS-FNA has progressively increased in Spain in recent years, following the trend observed in other European countries (according to data presented during the EGEUS 2017, but not published [www.egeus.org]). As far as therapeutic EUS is concerned, the number of procedures is much lower because it was implemented far more recently and also because the indications are more restricted. This makes it very difficult to acquire the necessary experience to carry out therapeutic EUS with sufficient guarantees. For this reason, there is consensus that, except for some technically simpler procedures, it should only be carried out in highly specialised centres. With that in mind, it is surprising that 85% of the hospitals in our survey carry out this type of procedure.
Miniprobes need to be discussed separately. These devices were initially designed for the staging of superficial cancers of the gastrointestinal tract, and therefore have high working frequencies (20MHz) which allow a greater precision in the visualisation of the layers of the wall. These devices were never designed for N staging and it is well known that miniprobes should not be used for this purpose, because the field of ultrasound vision is considerably reduced by the high frequencies. Moreover, a miniprobe with low frequencies would not provide any benefit to the conventional ultrasound endoscope. Despite the fact that, according to our data, 22% of Spanish hospitals had them in the past, they have now practically fallen into disuse. This may be due to the small number of cases in which they are indicated in our area and to their expiry date, which is determined not only by the date of acquisition but also by the number of times they are used. In addition, and very importantly, improvements in the images from conventional endoscopes mean that a good endoscopic examination is more useful for predicting how deep a cancer may have spread (T staging) than examination with a miniprobe.8 All the above reasons explain the gradual moving away from this technology in most indications, with the exception of intraductal EUS, which continues to have a role in the assessment of bile duct disorders in very specific cases. According to our survey, only one hospital in Spain currently has miniprobes, and these are the intraductal type.
In terms of indications, diagnostic EUS is used primarily for assessment of the biliary-pancreatic area, and then mainly for gastrointestinal tract cancer staging. These data are very similar to those obtained in the survey conducted in Belgium in 20056 and those presented at the last EGEUS congress in Turin in 2017. Other indications, such as study of the mediastinum, subepithelial tumours, portal hypertension and lymphadenopathy, are still valid, as EUS is better than the other imaging techniques, particularly if combined with FNA.9 However, only 63% of centres perform rectal EUS. The logical explanation for this is that rectal and anal disorders are usually managed surgically and patients are assessed and followed up by surgeons who have rigid endoscopic ultrasound probes.10 Within the indications of therapeutic EUS, drainage of pancreatic collections is the most common (93% indications), followed by biliary drainage (53%). Other indications, such as coeliac plexus neurolysis and vascular interventionism, are less prevalent, and gastrointestinal anastomosis is still in the development stages.
Spanish hospitals are well equipped to perform EUS-FNA, as they have needles of different types (cytology and histology) and of different sizes (19, 22 and 25 gauge). As in other countries in Europe, the United States and Asia, the 22 gauge needle is still the most used.7 In addition, 72% of our hospitals have a cytologist/cytotechnician in the room to perform ROSE, which helps to reduce the number of passes and the need for repeat investigations, with the consequent reduction in costs and greater safety for the patient.11 In the United States, practically all endoscopists (98%) have ROSE, but only 55% do so in Asia.7
Another aspect which varies greatly from one continent to another is the type of sedation used. In the United States, propofol administered by anaesthetists for deep sedation is the most common scenario (83%), while conscious sedation/anxiolysis is used in Europe and Asia. In Spain, in almost half of cases, sedation is administered by the EUS endoscopists themselves, who use propofol.7
Despite the large number of investigations each year and the fact that overall activity has increased in all centres, our survey shows that a significant number of EUS endoscopists (45%) performed fewer than 300 procedures a year, while in the United States, 69% of EUS endoscopists perform fewer than 100 a year.5 The American survey found that the number of EUS endoscopists per centre was two at the most, while in Spain the median is two and there are as many as four in some hospitals. Moreover, a quarter of them have less than 5 years’ experience. The fact that the practice of EUS is becoming more generalised is, in principle, positive. However, more endoscopists performing EUS in the same centre and introduction of the technique in centres with few patients could have a negative impact; the number of cases performed annually by each individual may be insufficient to maintain an adequate level of experience. As we mentioned earlier, this point is particularly important in the case of more complex procedures with a smaller volume of cases, such as some of the indications for therapeutic EUS. There are no formal recommendations at present regarding the number of procedures per year necessary to maintain a level of competence, and this needs to be discussed by an expert consensus group.
Last of all, one aspect which is crucial is how to ensure good training in EUS. The American Society for Gastrointestinal Endoscopy (ASGE) establishes a minimum of 150 supervised cases (75 of the bile duct and pancreas and 50 with FNA) to achieve accreditation in EUS.12 However, there is a lack of consensus on whether or not this is sufficient to become fully competent.4,13,14 The guidelines of the European Society of Gastrointestinal Endoscopy (ESGE) recommend from 6 to 24 months in a specialised centre to perform EUS-FNA.15 In general, it is agreed that 3–6 months of training should be sufficient to provide an acceptable level of competence, but 31% of Spanish endoscopists had a shorter training period. Specifically in Spain, there is no teaching of EUS during Gastrointestinal System specialisation. EUS is covered after doctors have finished their residency, without any specific accreditation programme, which means that the learning curve varies. However, there are currently two university academic programmes of theoretical and practical training to develop these skills from the University of Alcalá de Henares and the Universitat Oberta de Catalunya (UOC) [Open University of Catalonia]. Both courses require additional external rotation in specialised centres to guarantee autonomy in practical skills. Similarly, in the United States, the ASGE offers a joint training programme in EUS and ERCP (endoscopic retrograde cholangiopancreatography), and the French Club Francophone d’Echoendoscopie (EUS Endoscopy Club) has an Interuniversity Diploma.
The most important limitation of this study is that we do not have information on all Spanish hospitals, only those that responded to the survey. We cannot therefore be absolutely certain that the results can be generalised. The great variation in participation was surprising (for example, only 15% in one of the autonomous regions with the most centres equipped with EUS), particularly considering that most of the Spanish EUS endoscopists are members of the EUS Endoscopy Group of the SEED (Sociedad Española de Endoscopia Digestiva [Spanish Society for Gastrointestinal Endoscopy]). In any event, 49% participation is quite reasonable and in line with that obtained in other similar studies.7 Another limitation was that the type of questions asked did not allow us to analyse how EUS has evolved since its introduction in the early nineties. It would also be interesting to know what percentage of all endoscopic procedures is represented by EUS and, in order to estimate future needs, whether or not there has been an increase over time. However, the survey did not include these data. We can say that at Barcelona's Hospital Clínic EUS represented 4% of all endoscopic procedures in 2016. That rate is higher than the 1.66% reported in the American study.5 One last limitation is that we did not include any questions related to the practice of endobronchial ultrasound bronchoscopy in our hospitals, so we have no information on the extent to which this technique has been implemented (as there are no published data).
In conclusion, EUS is adequately implemented in Spain and good equipment is available. However, there is a high number of EUS endoscopists per centre, which decreases the number of cases performed individually and could be a problem in terms of maintaining the required level of skill, particularly in relation to therapeutic EUS. Lastly, a standardised training programme needs to be established for EUS, as the training of many EUS endoscopists may be insufficient when compared to the standards established by other Scientific Societies.
Conflicts of interestThe authors declare that they have no conflicts of interest.
The CERCA (Centres de Recerca de Catalunya [Catalan Research Centres]) programme of the Generalitat de Catalunya (Catalan Autonomous Government).
Please cite this article as: García-Rodríguez A, Fernández-Esparrach G, Sendino O, Ginès A, en representación del Grupo de Ecoendoscopia de la SEED. Estado de la ecoendoscopia en España en 2017. Gastroenterol Hepatol. 2018;41:672–678.