Glomus tumours are mesenchymal neoplasms originating in the glomus bodies. Glomus bodies are arteriovenous shunts responsible for the regulation of body temperature and homeostasis. They are located mainly in the nail beds and it is uncommon to find them in the gastrointestinal tract. Gastric glomus tumours (GGT) represent less than 1% of all mesenchymal tumours of the stomach and preoperative diagnosis is a challenge given the difficulty of obtaining adequate samples for pathological study.1
We present the case of a 41-year-old woman with no relevant previous history who consulted for epigastric pain. Gastroscopy and endoscopic ultrasound (EUS) were performed, showing a subepithelial antral lesion measuring 19×19mm, on which transgastric puncture was performed with 22G SharkCore needle guided by EUS.
The pathology report noted the presence of cell proliferation, without atypia, arranged around dilated vessels, with glomus tumour morphology and immunophenotype. Absence of metastatic disease was confirmed by extension computed tomography (CT).
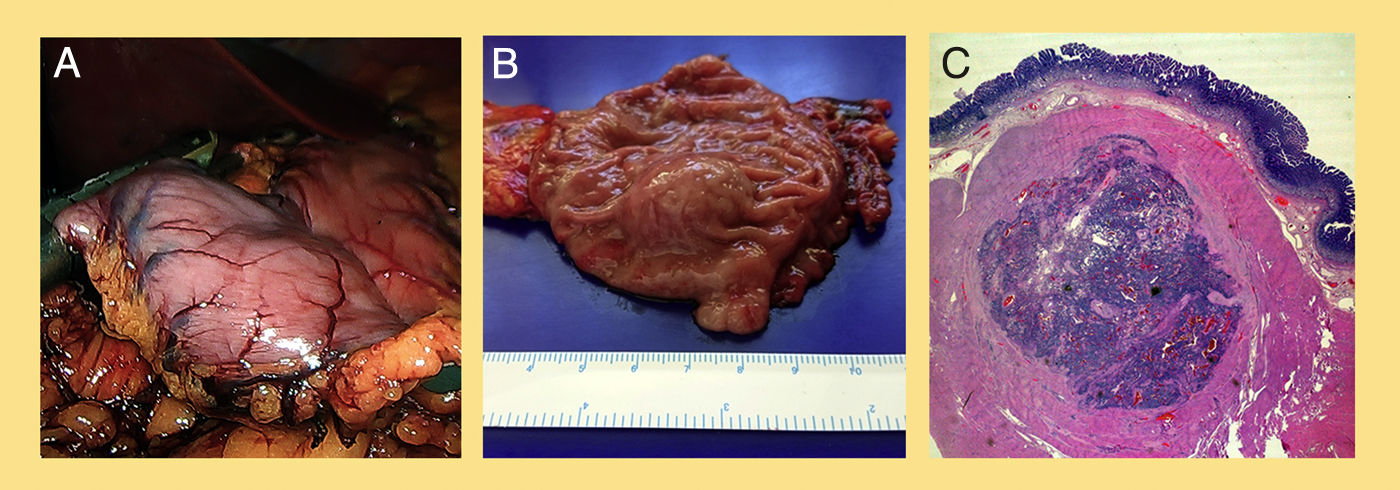
The patient was operated on laparoscopically, and, in view of the proximity to the pylorus, we opted for antrectomy and Roux-en-Y reconstruction (Fig. 1A, B). The postoperative period was uneventful, and the definitive histological study confirmed the preoperative diagnosis of GGT measuring 1.5cm, and free resection borders, without lymphovascular invasion or perineural infiltration (Fig. 1C). Immunohistochemistry was positive for calponin, caldesmon, collagen IV and smooth muscle actin, and negative for chromogranin, desmin and synaptophysin. The patient is currently asymptomatic.
(A) Image from the surgery in which a distal section is being made to the tumour with endostapler. (B) Fresh surgical specimen, with antral subepithelial lesion. (C) Microscopic image: tumour dependent on the submucosa, nodular and well-delimited, with proliferation of cells arranged around dilated vessels.
Glomus tumours are extremely uncommon in the gastrointestinal tract.2 In the gastric antrum, the most common types of tumour are adenocarcinoma and gastrointestinal stromal tumours (GIST).3 GIST are the most common submucosal gastric tumours.4
The rate of GGT is estimated to be 100 times lower than that of GIST. The prevalence of GGT is highest in females between the ages of 40 and 60.4
In the few published series, they tend to first manifest clinically with upper gastrointestinal bleeding and ulcerative symptoms with or without nausea or vomiting.3 Typically, they present as a solitary submucosal nodule that most often affects the greater curvature, the antrum and the pylorus, as was the case with our patient. They arise from the submucosal or muscle layer of the gastric wall and generally respect the mucosa.4
The diagnosis of these lesions is usually based on imaging techniques such as CT and EUS. EUS enables identification of the layer of tumour origin, observing a well-defined hypoechoic mass, dependent on the third and/or fourth EUS layer. However, immunohistochemical study allows the definitive diagnosis of GGT to be made, which in most cases is performed on the surgical specimen.
Nonetheless, the real challenge is to be able to diagnose this tumour preoperatively in order to plan the treatment strategy. The difficulty lies in obtaining adequate pathology samples, given their location in the deepest layers.2,4 Despite these limitations, our patient was diagnosed preoperatively by EUS-guided puncture of the lesion.
The differential diagnosis should be made with carcinoid tumours, with epithelioid-type GIST and with gastric lymphomas, and all these were ruled out by the immunohistochemical study performed. GIST is typically positive with c-KIT (CD117), carcinoid tumours are positive with chromogranin and gastric lymphoma is positive with the common leucocyte antigen, unlike the GGT, which would be negative with all these markers and characteristically positive with smooth muscle actin.3
The usual treatment is surgical resection. The largest study on glomus tumours in the gastrointestinal tract was conducted by Miettinem in 2002 and described a good prognosis in general for this type of tumour, except for one isolated case with malignant behaviour which was associated with the presence of spindle cell foci, slight atypia and vascular invasion. In our case, taking into account the histological characteristics described, we can expect a good clinical outcome.3
We wanted to use our case to highlight the challenge of diagnosing this uncommon condition preoperatively, as in most cases it is not diagnosed until after the pathology study of the surgical specimen. In our patient, preoperative diagnosis meant we were able to determine the prognosis beforehand and assess the most appropriate treatment strategy.
Please cite this article as: Arias-Romano AJ, Puya-Gamarro M, Rodríguez-Lobalzo SA, Bercedo-Martínez J. Tumor glómico gástrico: un reto en el diagnóstico preoperatorio de las lesiones subepiteliales del estómago. Gastroenterol Hepatol. 2018;41:670–671.