The aim of this study was to perform a systematic review and meta-analysis to assess the safety and efficacy of interventional treatment for Budd-Chiari syndrome (BCS) complicated by Inferior Vena Cava thrombosis (IVCT) patients.
MethodsWe evaluated the published studies on interventional treatment for BCS complicated by IVCT. Meta-analysis was used to calculate the combined effect size and their 95% confidence intervals (CI) based on random effect. The publication bias was assessed by Begg's test.
ResultsSixteen studies on interventional treatment for BCS complicated by IVCT patient were selected for meta-analysis, a total of 767 BCS complicated by IVCT patients were included. The combined effect size (95% CI) were 99% (98–100%) for the total successful rate of IVC recanalization, 15% (11–21%) for the rate of IVC restenosis after initial operation, 92.0% (86–97%) for the rate of clinical improvement, 76% (68–84%) for the rate of thrombus clearance and 0.00% (0–1%) for the incidence of pulmonary embolism (PE). Through subgroup meta-analysis about the rate of thrombus clearance, we got the pooled results (95% CI) of individualized treatment strategy (ITS) group and non-individualized treatment strategy (non-ITS) group, were 81% (71–92%) and 73% (63–83%), respectively.
ConclusionsThe interventional treatment for BCS complicated by IVCT patients is safe and effective with low incidence of PE, high thrombus clearance rate, high technically successful rate, good patency, and high clinical improvement rate. Moreover, subgroup analysis indicated that management based on the type and extent of the thrombus is proposed.
El objetivo de este estudio fue realizar una revisión y un metaanálisis sistemáticos para evaluar la seguridad y la eficacia del tratamiento intervencionista en los pacientes con el síndrome de Budd-Chiari (SBC), agravado por trombosis de la vena cava inferior (TVCI).
MétodosEvaluamos los estudios publicados sobre el tratamiento intervencionista del SBC agravado por TVCI. Se utilizó el metaanálisis para calcular el tamaño del efecto combinado y los intervalos de confianza (IC) del 95%, basados en el efecto aleatorio. El sesgo de publicación se evaluó con la prueba de Begg.
ResultadosPara el metaanálisis se seleccionaron 16 estudios sobre el tratamiento intervencionista de pacientes con SBC agravado por TVCI; se incluyó un total de 767 pacientes con SBC agravado por TVCI. El tamaño del efecto combinado (IC del 95%) fue del 99% (98-100%) para la tasa de éxito global de la recanalización de la vena cava inferior (VCI), un 15% (11-21%) para la tasa de reestenosis de la VCI después de la operación inicial, un 92% (86-97%) para la tasa de mejora clínica, un 76% (68-84%) para la tasa de eliminación de trombos y un 0% (0-1%) para la incidencia de embolia pulmonar. En el metaanálisis de subgrupos de la tasa de eliminación de trombos, los resultados combinados (IC del 95%) para el grupo de estrategia de tratamiento individualizado y el grupo de estrategia de tratamiento no individualizado fueron del 81% (71-92%) y del 73% (63-83%), respectivamente.
ConclusionesEl tratamiento intervencionista de pacientes con SBC agravado por TVCI es seguro y eficaz, con una baja incidencia de embolia pulmonar, una alta tasa de eliminación de trombos, una alta tasa de éxito técnico, una buena permeabilidad y una tasa elevada de mejora clínica. Además, el análisis de subgrupos reveló que el mejor enfoque es el tratamiento basado en el tipo y la extensión del trombo.
BCS is a group of hepatic vascular disorders characterized by the obstruction of the hepatic venous outflow tract in the absence of right heart failure or constrictive pericarditis.1 The obstruction causing primary BCS is usually located in the main hepatic vein (HV) or in the suprahepatic portion of IVC or both.2
In western countries, the vascular occlusion is involved HV alone for the majority of BCS cases, which caused by myeloproliferative neoplasms, etc.3 By comparison, a combined occlusion of HV and IVC is the most common type of primary BCS in China, and about 80% have membranous obstruction or short segmental obstruction of the IVC and HV.4 IVCT had been reported in about 20% of BCS patients, there are many reasons for its formation, such as blood stasis, turbulent, and reverse bloodstream caused by the obstruction of the IVC.5,6 For BCS complicated by IVCT patients, it is mainly concerned about PE caused by thrombus falling off into the pulmonary circulation system after opening IVC.7,8 It has been reported that about 12% of patients with venous thrombosis (include IVCT) may cause PE in United States.9 Hence, IVCT was for a time considered as a contraindication of interventional treatment on account of potential risk of fatal PE.10
In 1992, Japanese scholars reported the first successful endovascular treatment experience of BCS complicated by IVCT patient, suggested the combination of local thrombolytic therapy, percutaneous transluminal balloon angioplasty (PTBA), and stent placement can be useful in the treatment of BCS complicated by IVCT patient.11 With the development of interventional radiology, more and more nonsurgical treatments were used for this kind of disease, such as pre-dilation,12,13 retrieval stent filter,12,14,15 agitation thrombolysis,12 transcatheter thrombolysis5,12 and thrombus aspiration.5,16–20
The purpose of this study was to summarize and analyze the therapeutic effect of BCS complicated by IVCT by calculating the rate of each study:(1) the successful rate of IVC recanalization; (2) the rate of IVC restenosis (including IVC reocclusion) after initial operation during follow-up; (3) the incidence of PE; (4)the thrombus clearance rate; (5) the rate of clinical improvement.
Materials and methodsSearch strategyStudies were identified in the PubMed, EMBASE, Cochrane Library, CNKI and WanFang databases by two interventional radiologists with experience of 13 and 9 years respectively. Search items as follows: (Budd-Chiari Syndrome[Title/Abstract]) OR Budd Chiari Syndrome[Title/Abstract]) OR Hepatic Venous Outflow Obstruction[Title/Abstract]) OR Chiari's Syndrome[Title/Abstract]) OR Chiari Syndrome[Title/Abstract]) OR Chiaris Syndrome[Title/Abstract]) OR Hepatic Vein Thrombosis[Title/Abstract]) OR Hepatic Vein Thromboses[Title/Abstract]) OR Thromboses, Hepatic Vein[Title/Abstract]) OR Vein Thromboses, Hepatic Vein Thrombosis, Hepatic[Title/Abstract]) OR Thrombosis, Hepatic Vein[Title/Abstract])) AND (((Inferior vena cava Thrombus[Title/Abstract]) OR Inferior vena cava Thrombosis[Title/Abstract]) OR Inferior vena cava Thromboses[Title/Abstract]). The last search was performed on December 1, 2019. In addition, we read the reference lists from selected articles carefully to search potential relevant studies. When the similar data were reported in more than one publication, only the studies with more complete data and more extensive interval of enrollment were included in this study. To ensure data integrity as much as possible, we extracted partial valid data from two articles.
Eligibility criteriaEach searched study was separately reviewed by two researchers (two interventional radiologists with experience of 13 and 9 years respectively) to determine if it was suitable for inclusion in this study. The inclusion criteria were as follows: (1) the participants were diagnosed with primary BCS complicated by IVCT;(2) detailed information (treatment plan, clinical outcome, etc.) were provided; (3) all observational studies regardless of retrospective or prospective study; (4) the publication date, publication language, or publication status were not restricted. Exclusion criteria such as case reports (<10 patients), nursing related, surgical treatment, comment, review, diagnostic, dissertation, conference paper, animal studies, etc. If the two researchers did not reach an agreement about eligibility of the article, the third reviewer participated in consensus building.
Data extractionData were extracted by two reviewers independently; disagreements were adjudicated by the third interventional radiologist with experience of 29 years. The following valid data were collected from all 16 studies: first author, publication year, number of sample, demographic data (age and gender), thrombus management, thrombus property, follow-up duration, stent type, thrombus detection methods, anticoagulation strategy, duration of BCS, clinical manifestations, study results (the successful rate of IVC recanalization, the rate of IVC restenosis after initial operation during follow-up, the incidence of PE, the thrombus clearance rate, and the rate of clinical improvement).
Statistical analysisBased on the sample size of individual studies, exact binomial confidence intervals were calculated for each study, and pooled measure was calculated as along with an equal weighted average rate (weighted by each study's sample size) in all samples. The Q test and I2 were used to assess heterogeneity among studies. The ‘leave one out’ sensitive analysis was carried out using I2 >50% and p<0.1 as the criteria to evaluate the studies with substantial impact on between-study heterogeneity. Publication bias was estimated by Begg's test. All statistical analyses were performed with STATA version 15 (Stata Corporation, College Station, Texas, USA). All reported probabilities (p values) were two-sided, with p<0.05 considered statistically significant.
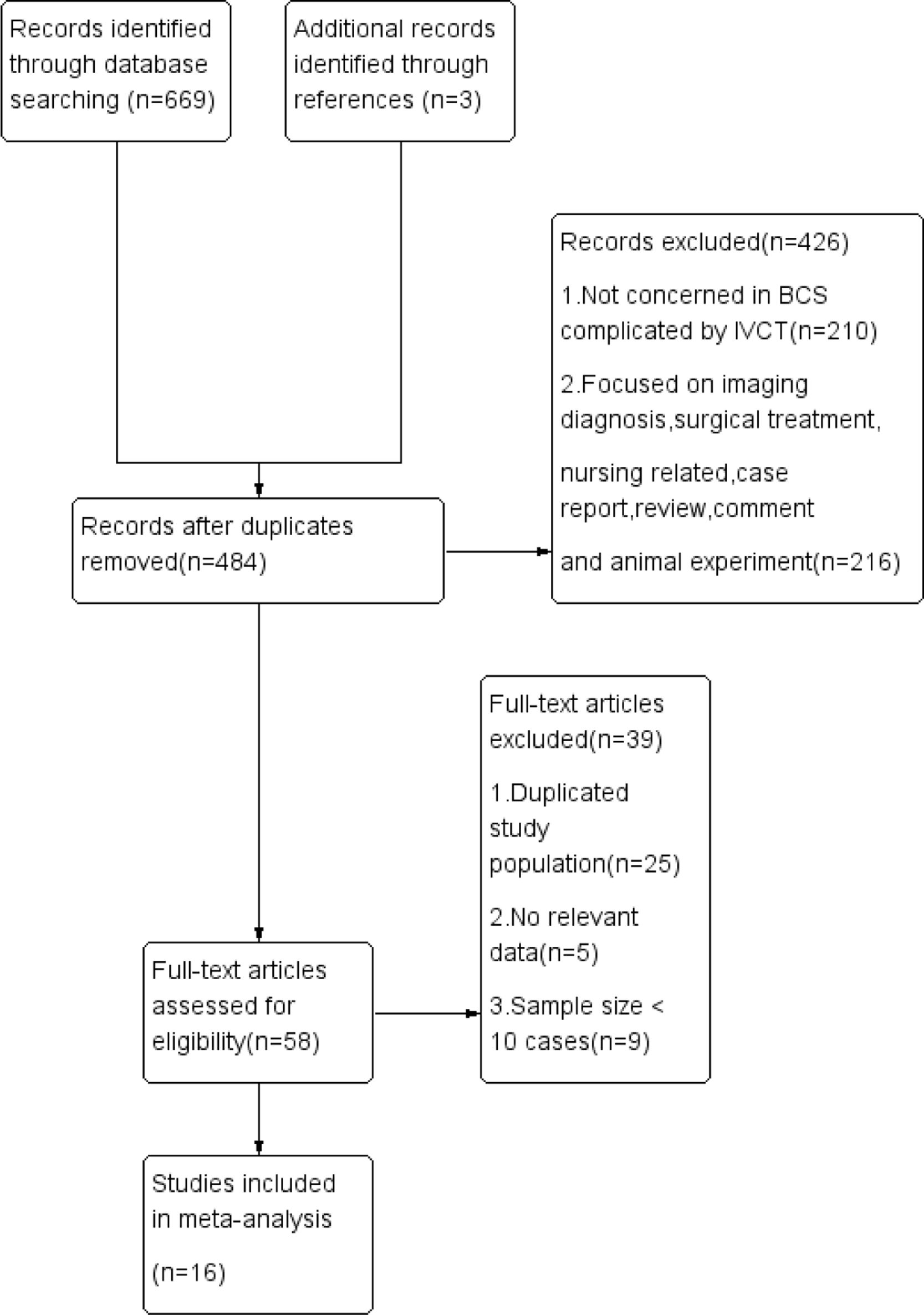
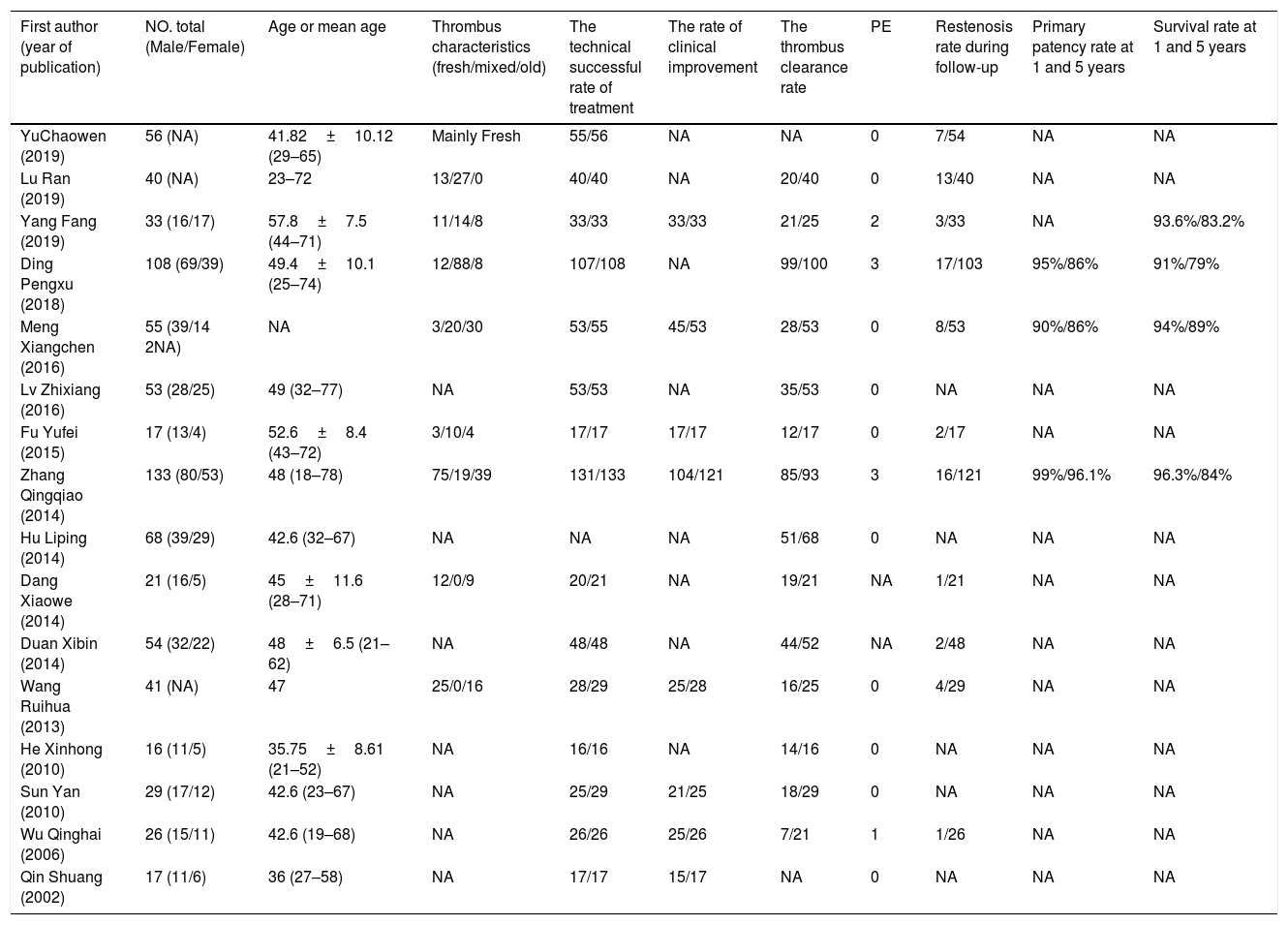
ResultsStudy characteristicsThe study identification and selection process are shown in Fig. 1. Sixteen eligible studies which conformed the inclusion criteria included 767 BCS complicated by IVCT patients treated by interventional treatment in our meta-analysis. 7 studies were reported in Chinese language among these studies. Baseline characteristics of included studies are shown in Table 1. Clinic data such as thrombus management, thrombus property, stent type, thrombus detection methods and anticoagulation strategy are shown in Table 2. Clinical manifestations pre- and post-treatment of included studies are shown in Table 3. Six of 16 literatures choose treatment plan based on thrombus type and range were classified as ITS group, and the remaining 10 articles did not consider the nature of thrombus when choosing the treatment plan were classified as non-ITS group.
Baseline characteristics of included studies of interventional treatment with BCS complicated by IVCT.
| First author (year of publication) | NO. total (Male/Female) | Age or mean age | Thrombus characteristics (fresh/mixed/old) | The technical successful rate of treatment | The rate of clinical improvement | The thrombus clearance rate | PE | Restenosis rate during follow-up | Primary patency rate at 1 and 5 years | Survival rate at 1 and 5 years |
|---|---|---|---|---|---|---|---|---|---|---|
| YuChaowen (2019) | 56 (NA) | 41.82±10.12 (29–65) | Mainly Fresh | 55/56 | NA | NA | 0 | 7/54 | NA | NA |
| Lu Ran (2019) | 40 (NA) | 23–72 | 13/27/0 | 40/40 | NA | 20/40 | 0 | 13/40 | NA | NA |
| Yang Fang (2019) | 33 (16/17) | 57.8±7.5 (44–71) | 11/14/8 | 33/33 | 33/33 | 21/25 | 2 | 3/33 | NA | 93.6%/83.2% |
| Ding Pengxu (2018) | 108 (69/39) | 49.4±10.1 (25–74) | 12/88/8 | 107/108 | NA | 99/100 | 3 | 17/103 | 95%/86% | 91%/79% |
| Meng Xiangchen (2016) | 55 (39/14 2NA) | NA | 3/20/30 | 53/55 | 45/53 | 28/53 | 0 | 8/53 | 90%/86% | 94%/89% |
| Lv Zhixiang (2016) | 53 (28/25) | 49 (32–77) | NA | 53/53 | NA | 35/53 | 0 | NA | NA | NA |
| Fu Yufei (2015) | 17 (13/4) | 52.6±8.4 (43–72) | 3/10/4 | 17/17 | 17/17 | 12/17 | 0 | 2/17 | NA | NA |
| Zhang Qingqiao (2014) | 133 (80/53) | 48 (18–78) | 75/19/39 | 131/133 | 104/121 | 85/93 | 3 | 16/121 | 99%/96.1% | 96.3%/84% |
| Hu Liping (2014) | 68 (39/29) | 42.6 (32–67) | NA | NA | NA | 51/68 | 0 | NA | NA | NA |
| Dang Xiaowe (2014) | 21 (16/5) | 45±11.6 (28–71) | 12/0/9 | 20/21 | NA | 19/21 | NA | 1/21 | NA | NA |
| Duan Xibin (2014) | 54 (32/22) | 48±6.5 (21–62) | NA | 48/48 | NA | 44/52 | NA | 2/48 | NA | NA |
| Wang Ruihua (2013) | 41 (NA) | 47 | 25/0/16 | 28/29 | 25/28 | 16/25 | 0 | 4/29 | NA | NA |
| He Xinhong (2010) | 16 (11/5) | 35.75±8.61 (21–52) | NA | 16/16 | NA | 14/16 | 0 | NA | NA | NA |
| Sun Yan (2010) | 29 (17/12) | 42.6 (23–67) | NA | 25/29 | 21/25 | 18/29 | 0 | NA | NA | NA |
| Wu Qinghai (2006) | 26 (15/11) | 42.6 (19–68) | NA | 26/26 | 25/26 | 7/21 | 1 | 1/26 | NA | NA |
| Qin Shuang (2002) | 17 (11/6) | 36 (27–58) | NA | 17/17 | 15/17 | NA | 0 | NA | NA | NA |
Data are presented as n (%); BCS, Budd-Chiari syndrome; IVC, Inferior Vena Cava; IVCT, Inferior Vena Cava thrombosis; PE, pulmonary embolism; NO. number; NA, not available.
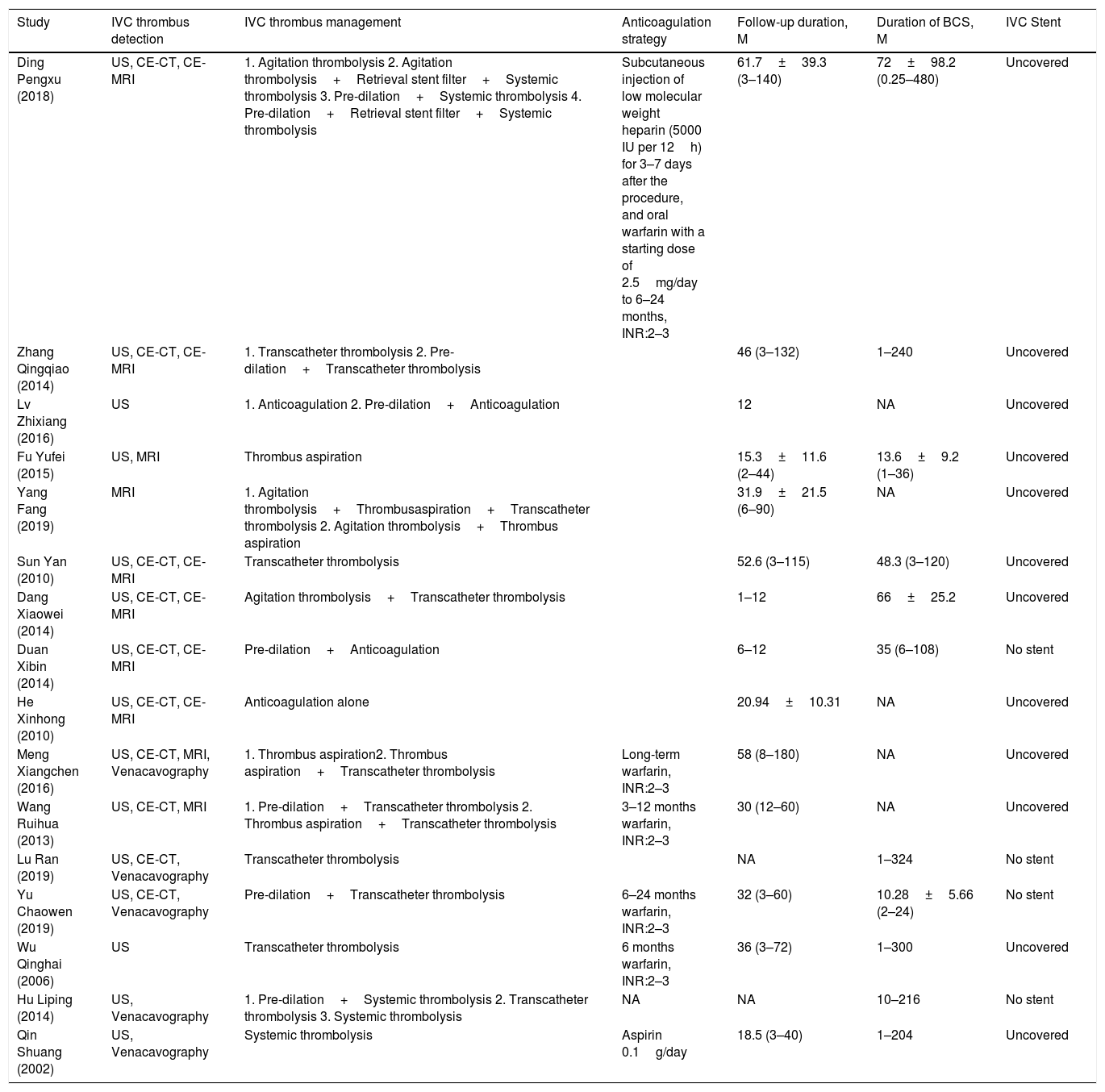
Clinical data of the included studies.
| Study | IVC thrombus detection | IVC thrombus management | Anticoagulation strategy | Follow-up duration, M | Duration of BCS, M | IVC Stent |
|---|---|---|---|---|---|---|
| Ding Pengxu (2018) | US, CE-CT, CE-MRI | 1. Agitation thrombolysis 2. Agitation thrombolysis+Retrieval stent filter+Systemic thrombolysis 3. Pre-dilation+Systemic thrombolysis 4. Pre-dilation+Retrieval stent filter+Systemic thrombolysis | Subcutaneous injection of low molecular weight heparin (5000 IU per 12h) for 3–7 days after the procedure, and oral warfarin with a starting dose of 2.5mg/day to 6–24 months, INR:2–3 | 61.7±39.3 (3–140) | 72±98.2 (0.25–480) | Uncovered |
| Zhang Qingqiao (2014) | US, CE-CT, CE-MRI | 1. Transcatheter thrombolysis 2. Pre-dilation+Transcatheter thrombolysis | 46 (3–132) | 1–240 | Uncovered | |
| Lv Zhixiang (2016) | US | 1. Anticoagulation 2. Pre-dilation+Anticoagulation | 12 | NA | Uncovered | |
| Fu Yufei (2015) | US, MRI | Thrombus aspiration | 15.3±11.6 (2–44) | 13.6±9.2 (1–36) | Uncovered | |
| Yang Fang (2019) | MRI | 1. Agitation thrombolysis+Thrombusaspiration+Transcatheter thrombolysis 2. Agitation thrombolysis+Thrombus aspiration | 31.9±21.5 (6–90) | NA | Uncovered | |
| Sun Yan (2010) | US, CE-CT, CE-MRI | Transcatheter thrombolysis | 52.6 (3–115) | 48.3 (3–120) | Uncovered | |
| Dang Xiaowei (2014) | US, CE-CT, CE-MRI | Agitation thrombolysis+Transcatheter thrombolysis | 1–12 | 66±25.2 | Uncovered | |
| Duan Xibin (2014) | US, CE-CT, CE-MRI | Pre-dilation+Anticoagulation | 6–12 | 35 (6–108) | No stent | |
| He Xinhong (2010) | US, CE-CT, CE-MRI | Anticoagulation alone | 20.94±10.31 | NA | Uncovered | |
| Meng Xiangchen (2016) | US, CE-CT, MRI, Venacavography | 1. Thrombus aspiration2. Thrombus aspiration+Transcatheter thrombolysis | Long-term warfarin, INR:2–3 | 58 (8–180) | NA | Uncovered |
| Wang Ruihua (2013) | US, CE-CT, MRI | 1. Pre-dilation+Transcatheter thrombolysis 2. Thrombus aspiration+Transcatheter thrombolysis | 3–12 months warfarin, INR:2–3 | 30 (12–60) | NA | Uncovered |
| Lu Ran (2019) | US, CE-CT, Venacavography | Transcatheter thrombolysis | NA | 1–324 | No stent | |
| Yu Chaowen (2019) | US, CE-CT, Venacavography | Pre-dilation+Transcatheter thrombolysis | 6–24 months warfarin, INR:2–3 | 32 (3–60) | 10.28±5.66 (2–24) | No stent |
| Wu Qinghai (2006) | US | Transcatheter thrombolysis | 6 months warfarin, INR:2–3 | 36 (3–72) | 1–300 | Uncovered |
| Hu Liping (2014) | US, Venacavography | 1. Pre-dilation+Systemic thrombolysis 2. Transcatheter thrombolysis 3. Systemic thrombolysis | NA | NA | 10–216 | No stent |
| Qin Shuang (2002) | US, Venacavography | Systemic thrombolysis | Aspirin 0.1g/day | 18.5 (3–40) | 1–204 | Uncovered |
Data are presented as n; Data are medians, ranges or combined; M, months; INR, international normalized ratio; US, ultrasound; CE-CT, contrast enhanced computed tomography; CE-MRI, contrast enhanced magnetic resonance imaging; IVC, Inferior Vena Cava; BCS, Budd-Chiari syndrome; NA, not available.
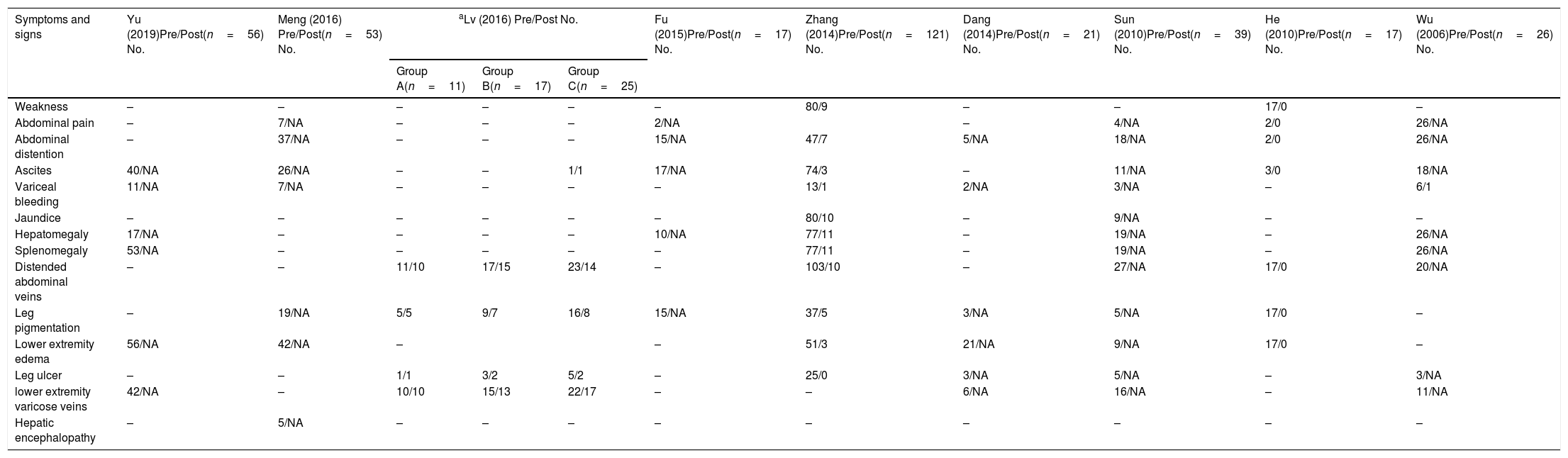
Comparison of clinical manifestations pre- and post-treatment of the included studies.
| Symptoms and signs | Yu (2019)Pre/Post(n=56) No. | Meng (2016) Pre/Post(n=53) No. | aLv (2016) Pre/Post No. | Fu (2015)Pre/Post(n=17) No. | Zhang (2014)Pre/Post(n=121) No. | Dang (2014)Pre/Post(n=21) No. | Sun (2010)Pre/Post(n=39) No. | He (2010)Pre/Post(n=17) No. | Wu (2006)Pre/Post(n=26) No. | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Group A(n=11) | Group B(n=17) | Group C(n=25) | |||||||||
| Weakness | – | – | – | – | – | – | 80/9 | – | – | 17/0 | – |
| Abdominal pain | – | 7/NA | – | – | – | 2/NA | – | 4/NA | 2/0 | 26/NA | |
| Abdominal distention | – | 37/NA | – | – | – | 15/NA | 47/7 | 5/NA | 18/NA | 2/0 | 26/NA |
| Ascites | 40/NA | 26/NA | – | – | 1/1 | 17/NA | 74/3 | – | 11/NA | 3/0 | 18/NA |
| Variceal bleeding | 11/NA | 7/NA | – | – | – | – | 13/1 | 2/NA | 3/NA | – | 6/1 |
| Jaundice | – | – | – | – | – | – | 80/10 | – | 9/NA | – | – |
| Hepatomegaly | 17/NA | – | – | – | – | 10/NA | 77/11 | – | 19/NA | – | 26/NA |
| Splenomegaly | 53/NA | – | – | – | – | – | 77/11 | – | 19/NA | – | 26/NA |
| Distended abdominal veins | – | – | 11/10 | 17/15 | 23/14 | – | 103/10 | – | 27/NA | 17/0 | 20/NA |
| Leg pigmentation | – | 19/NA | 5/5 | 9/7 | 16/8 | 15/NA | 37/5 | 3/NA | 5/NA | 17/0 | – |
| Lower extremity edema | 56/NA | 42/NA | – | – | 51/3 | 21/NA | 9/NA | 17/0 | – | ||
| Leg ulcer | – | – | 1/1 | 3/2 | 5/2 | – | 25/0 | 3/NA | 5/NA | – | 3/NA |
| lower extremity varicose veins | 42/NA | – | 10/10 | 15/13 | 22/17 | – | – | 6/NA | 16/NA | – | 11/NA |
| Hepatic encephalopathy | – | 5/NA | – | – | – | – | – | – | – | – | – |
Data are presented as n; a, Patients in this study were divided into three groups: group A warfarin anticoagulation alone; group B 6-mm balloon pre-dilation+warfarin; group C 10-mm balloon pre-dilation+warfarin; NO. number; NA, not available.
Pre-dilation means dilation of IVC with a small balloon (5–10mm in diameter) for partial reconstruction IVC blood flow before thrombolysis. Agitation thrombolysis means using pigtail catheter and guidewire to break up the thrombus in combination with pulse-spray thrombolysis. Transcatheter thrombolysis means inserting a thrombolytic catheter to the thrombus location, then continue to pump urokinase through catheter with a micro-infusion pump when back to the ward. Thrombus aspiration was performed by a 6F-12F catheter, and it was moved back and forth and synchronously rotated to facilitate aspiration of IVC thrombus when it was set at the level of the thrombus. Thrombus clearance is defined as complete or near complete disappearance of thrombus after thrombolysis. Clinical improvement means BCS-related symptoms and signs (such as variceal bleeding, ascites, abdominal pain, lower extremity edema, etc.) disappear or alleviate obviously after treatment.
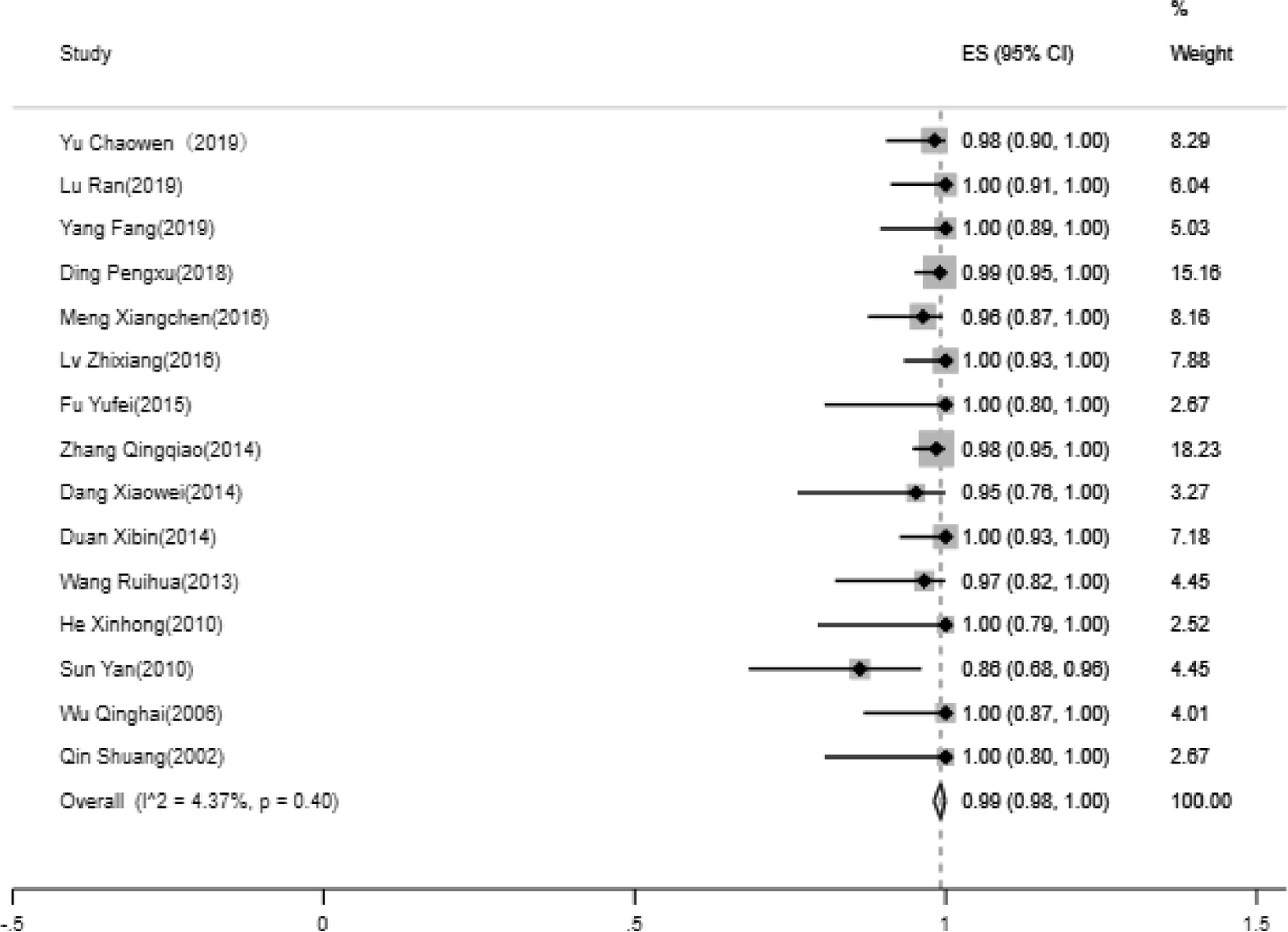
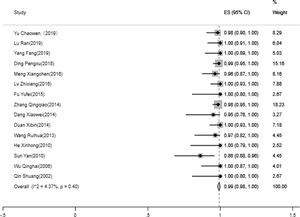
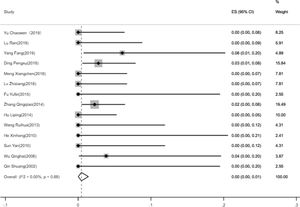
The technically successful rate of IVC recanalization15 papers were analyzed for the technically successful rate of IVC recanalization, including 9 in non-ITS group and 6 in ITS group. Heterogeneity test indicated that there is no significant heterogeneity between the included 15 literatures. Based on the meta-analysis of random effect, the total effect quantity of 15 studies was 0.99, and the 95% confidence interval was 0.98–1.00, which was statistically significant (z=67.99, p<0.05) (Fig. 2). Come to the pooled result (95% CI) of the total rate of clinical improvement was 99.0% (98–100%).
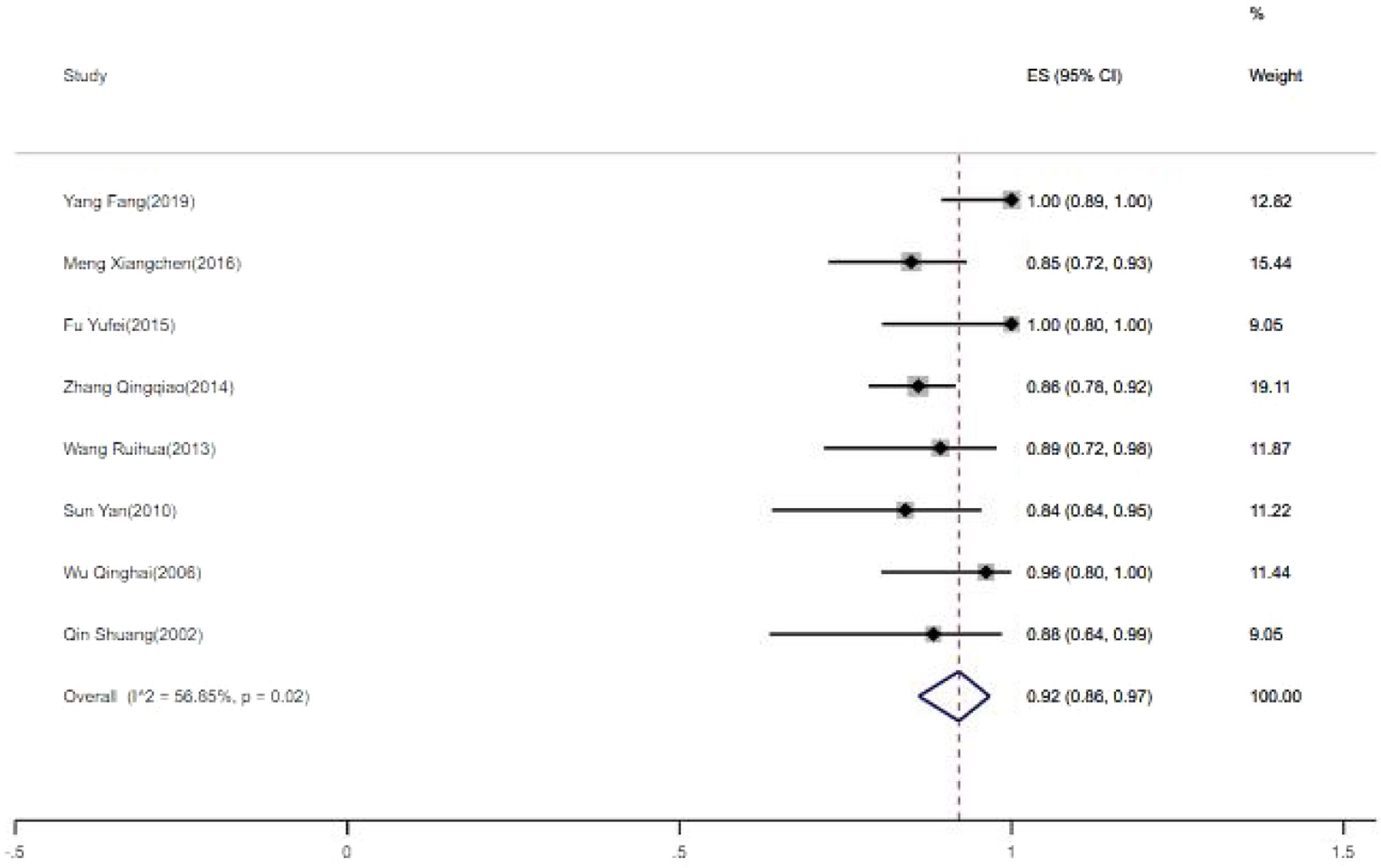
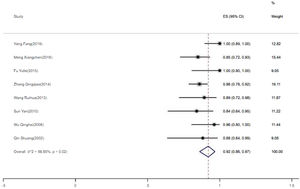
The rate of clinical improvement8 papers were analyzed for the rate of clinical improvement. Heterogeneity test suggested that there is significant heterogeneity between the included 8 literatures. In order to ensure the accuracy and stability of the study, sensitivity analysis was conducted. Sensitivity analysis shows none of 8 literatures caused great interference to the results of this meta-analysis, which means that this study has good stability. Based on the meta-analysis of random effect, the total effect quantity of 8 studies was 0.92, and the 95% confidence interval was 0.86–0.97, which was statistically significant (z=25.43, p<0.05) (Fig. 3). Come to the pooled result (95% CI) of the total rate of clinical improvement was 92.0% (86–97%).
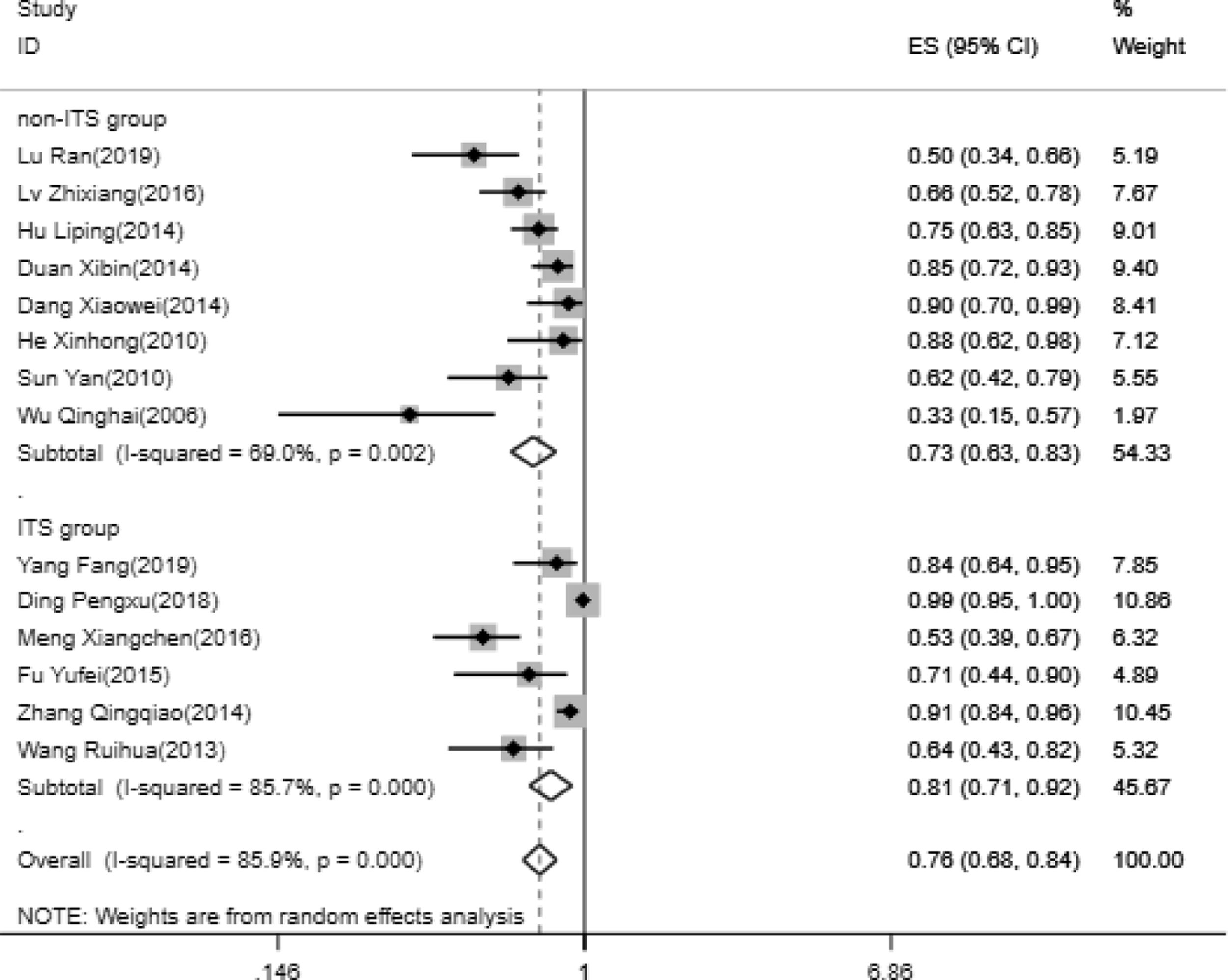
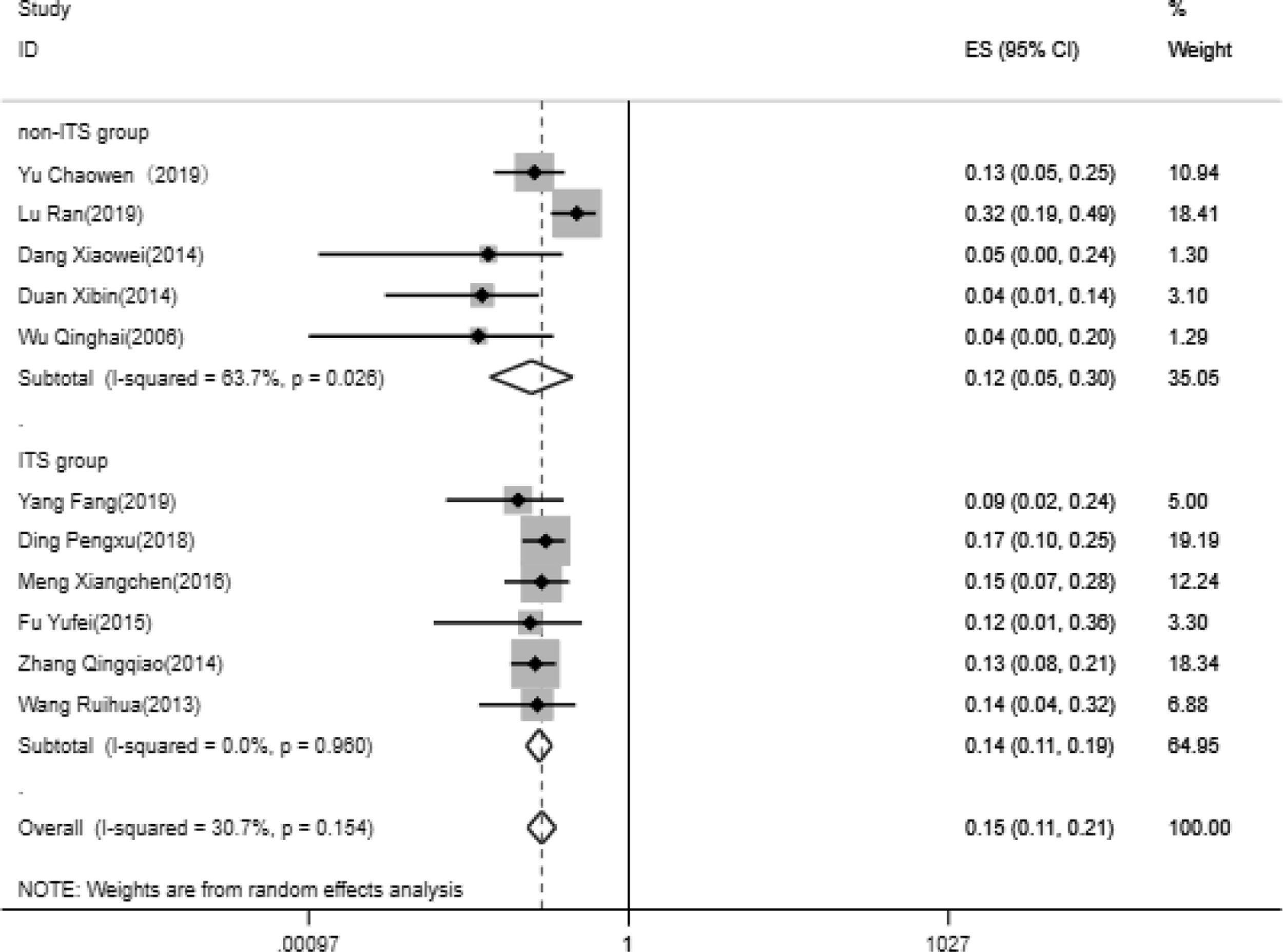
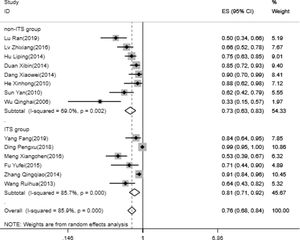
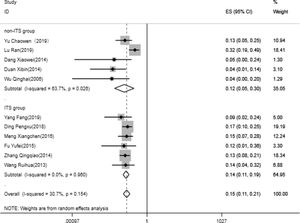
The rate of thrombus clearance14 papers were analyzed for the rate of thrombus clearance, including 8 in non-ITS group and 6 in ITS group. Heterogeneity test suggested that there is significant heterogeneity between the included 14 literatures in this study. In order to ensure the accuracy and stability of the study, sensitivity analysis was conducted. Sensitivity analysis shows none of 14 literatures caused great interference to the results of this meta-analysis, which means that this study has good stability. Based on the meta-analysis of random effect, the total effect quantity of 14 studies was 76%, and the 95% confidence interval was 68–84%, which was statistically significant (z=14.8, p<0.05) (Fig. 4). Subgroup analysis showed the pooled results (95% CI) of ITS group and non-ITS group, were 81% (71–92%) and 73% (63–83%), respectively.
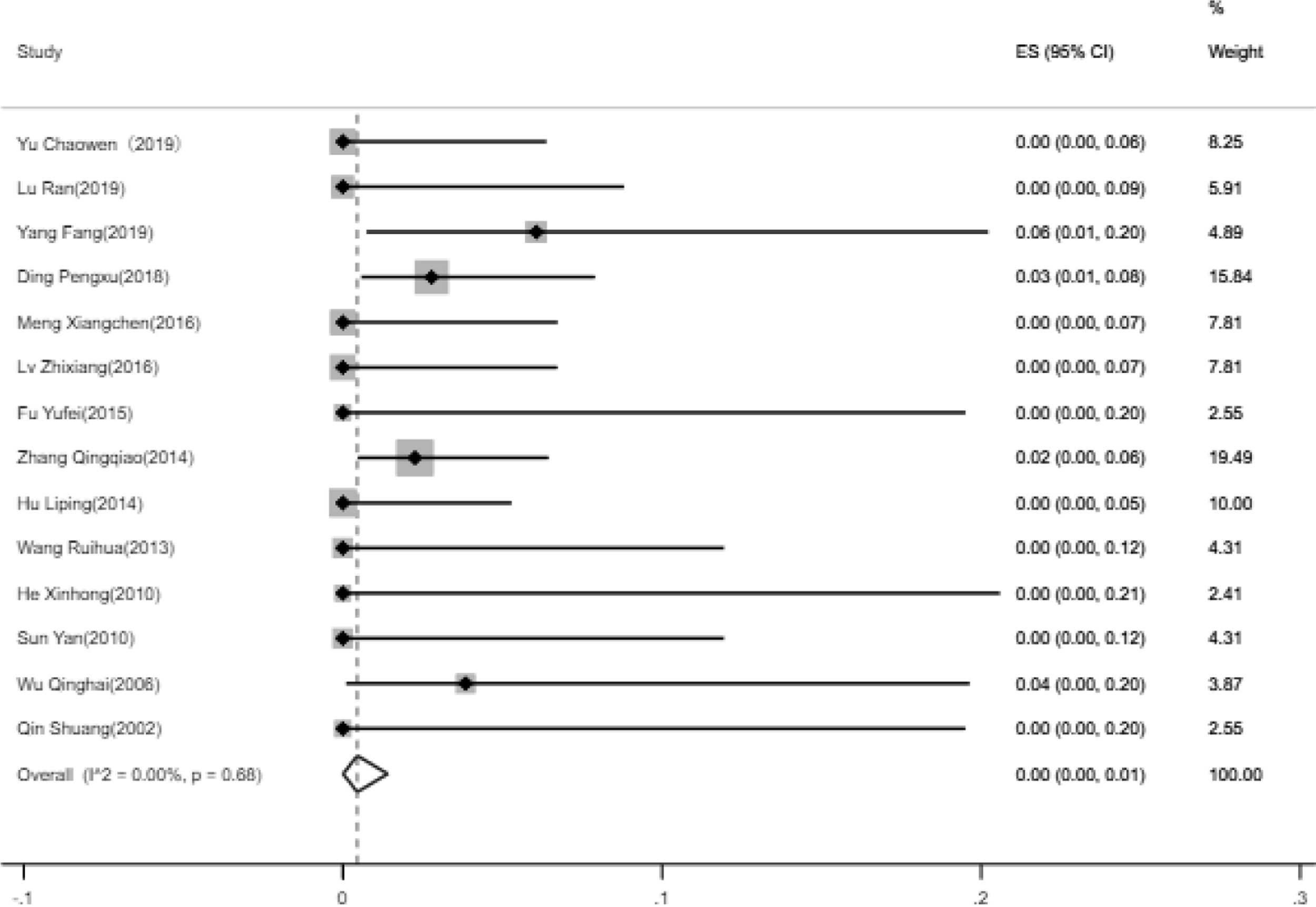
The incidence of pulmonary embolism14 papers were analyzed for the incidence of PE. Heterogeneity test suggested that there is no significant heterogeneity between the included 14 literatures, Based on the meta-analysis of random effect, the total effect quantity of 14 studies was 0.00, and the 95% confidence interval was 0.00–0.01, which was statistically significant (z=2.07, p<0.05)(Fig. 5). Come to the pooled result (95% CI) of the total incidence of PE was 0.00% (0–1%).
The rate of IVC restenosis after initial operation during follow-up11 papers were analyzed for the rate of thrombus clearance, including 5 in non-ITS group and 6 in ITS group. Heterogeneity test suggested that there is significant heterogeneity between the included 11 literatures in this study. In order to ensure the accuracy and stability of the study, sensitivity analysis was conducted. Sensitivity analysis shows none of 11 literatures caused great interference to the results of this meta-analysis, which means that this study has good stability. Based on the meta-analysis of random effect, the total effect quantity of 11 studies was 15%, and the 95% confidence interval was 11–21%, which was statistically significant (z=9.63, p<0.05) (Fig. 6). Subgroup analysis got the pooled results (95% CI) of ITS group and non-ITS group, were 14% (11–19%) and 12% (5–30%), respectively.
Publication biasBegg's test was applied to assess publication bias of the results in the studies. It indicated that there was no publication bias on the successful rate of IVC recanalization (p=0.428), the thrombus clearance rate (p=0.545), the rate of IVC restenosis (p=0.276), the rate of clinical improvement (p=0.319), the incidence of pulmonary embolism (p=0.139).
DiscussionAs far as we know, the present study was the first meta-analysis to evaluate the effect of interventional treatment for BCS complicated by IVCT patients. The findings from this meta-analysis indicate that interventional treatment of IVCT according to the property and involvement range of thrombus for the majority of BCS complicated by IVCT patients is safe and efficiency with low incidence of PE, high thrombus clearance rate, high technically successful rate, good patency, and high clinical improvement rate.
16 articles were included in the present study, 767 such patients had received interventional therapy, of course, there may be more such patients not reported publicly. In this study, through meta-analysis we got the total successful rate of IVC recanalization and the rate of clinical improvement were 99% and 92.0%, respectively. Such good results are attributed to the continuous development of interventional radiology, the innovation of interventional instruments, and the unremitting efforts of interventional radiologists. As a result, minimal invasive treatment such as PTBA with or without stent placement has been recently recommended as the first-line treatment for IVC lesion of primary BCS patients.21,22 At the same time, the step-wise management proposed by European scholars has gradually gained consensus in the industry.23,24 Step-wise strategy includes anticoagulation, pathogenesis treatment, percutaneous recanalization of occluded HV/IVC and transjugular intrahepatic portosystemic shunt (TIPS) to re-establish HV drainage, and orthotopic liver transplantation was conducted in unresponsive patients.24
IVCT can be divided into three types: fresh thrombus, mixed thrombus and old thrombus, based on the organization degree of thrombus. Gross examination, fresh thrombus contained mainly fresh, dark red, soft blood clot that could be easily aspirated, mixed thrombus was often a small amount of gray-white thrombi that could not easily be thoroughly aspirated.5,19 Because IVC combined HV type is the most common BCS type in China, so IVCT frequently seen in Chinese BCS patients. All the patients in this study were from China, which can also prove this. It is very important to make a correct judgment on the nature of thrombus before treatment. It determines the choice of treatment options. According to the preoperative imaging examination (ultrasonography, computed tomography venography, magnetic resonance venography), intra-operative venography, and combined with the medical history, we can roughly determine the type of thrombus. Of course, it is more reliable to judge the type of thrombus according to gross examination of the captured thrombus. Zhang et al.19 and Yang et al.20 took transcatheter aspiration of the thrombus first to determine the nature of thrombus, then they chose direct transcatheter thrombolysis or transcatheter thrombolysis after pre-dilation according to the type of thrombus. In their studies, the thrombus clearance rates were 91% and 84%, respectively, which were higher than the total thrombus clearance rate (76%) obtained by meta-analysis in present study. It is suggested that accurate evaluation of thrombus properties can improve the clinical efficacy.
Analysis the clinical results of each treatments according to different thrombus types may lead to the best treatment for each thrombus type. Through careful reading of 16 literatures, we found that 2 of the 16 included literatures selected the treatment plan and provided effective data according to the fresh, mixed and old property of thrombus separately. Fresh thrombus and mixed thrombus were classified into one group and treated with the same treatment scheme in 4 literatures, separated from old thrombus. The remaining 10 articles did not consider the nature of thrombus when choosing the treatment plan. We cannot analyze sub-categories of treatments for each different thrombus type. But we divided the literatures into two groups (ITS group and non-ITS group) according to whether they choose treatment plan based on thrombus type and range. Through subgroup meta-analysis about the rate of thrombus clearance, we got the pooled results of ITS group and non-ITS group, were 81% and 73%, respectively. It is suggested that individualized treatment based on thrombus type and range is more beneficial to thrombus clearance. For the fresh and mix thrombus, treatments as transcatheter aspiration, transcatheter thrombolysis, agitation thrombolysis, and pre-dilation are all good choices.12,17,19,20 For the old thrombus, considering its tissue organization and strong adhesion with the vascular wall, many studies adopted direct PTBA with or without stent placement.12,18 Stent for compressing thrombus maybe a safe and effective choice for patients who are not suitable for anticoagulation and thrombolysis (such as with gastrointestinal bleeding), but there is a risk of obstruction of the HV or accessory HV.
The most concerned problem in the treatment of BCS complicated by IVCT patients is that thrombus falls off into pulmonary artery and causes serious PE after IVC is opened. In the present study, the pooled incidence of PE was 0%. In the included 16 studies, 695 patients underwent IVC recanalization, only 9 cases of PE were reported (7 cases of symptomatic PE were cured after drug treatment, 1 case of asymptomatic PE, 1 case death). It is suggested that endovascular therapy is safe for BCS complicated by IVCT patients.
Restenosis occurs in all types of BCS, which consequently determines symptom recurrence, ensuing treatment and patient outcome. How to prevent restenosis is an urgent clinical problem. In this study, the pooled rate of IVC restenosis was 15%. Subgroup analysis got the pooled results (95% CI) of ITS group and non-ITS group, were 14% (11–19%) and 12% (5–30%), respectively. The rate of restenosis was similar between the two groups. We consider that restenosis maybe not related to the treatment of thrombus, but to the IVC lesion itself (membranous or segmental occlusion). Recent research shows that IVC segmental occlusion was an independent risk factor for re-occlusion in IVC type BCS patients.25 Li et al.26 described IVC stent placement in 172 IVC type BCS patients, the median duration of follow-up was 32.8 months, and 28 patients experienced restenosis during follow-up, restenosis rate was 16.3%. Restenosis rate determines patency rate. Ding et al.,12 Meng et al.5 and Zhang et al.19 reported the primary patency rate was 86%, 86% and 96.1% at 5 years, respectively. Aim to study whether stent placement can reduce restenosis rate, Wang et al. designed a prospective RCT clinical trial,27 partial public data from their study display the rate of recanalized veins restenosis were significantly lower in angioplasty plus routine stenting group than in angioplasty-only group (0% vs. 24% at 1 year and 4% vs. 40% at 3 years), respectively. It is suggested that stent placement can reduce the restenosis rate.
With the application of interventional therapy in BCS complicated by IVCT patients, most such patients can be cured by minimally invasive treatment now. However, different thrombus nature and range in IVC induce some variance existing in different interventional means for BCS complicated by IVCT. Through meta-analysis of the subgroups, we can see that ITS group is better than non-ITS group in thrombus clearance rate, but they are equal in IVC restenosis rate. Thus, patients with BCS complicated by IVCT should be managed on an individualized basis, according to the thrombus type and range involvement.
Our study had a few limitations. Firstly, we cannot analyze sub-categories of treatments for different thrombus types due to the limitation extractable data. But we divided the literatures into two groups (ITS group and non-ITS group) according to whether they choose treatment plan based on thrombus type and range. And meta-analysis of the subgroups was carried out. Secondly, the rational selection of interventional methods, thrombolytic drugs dosage, and the operational proficiency all influenced the treatment outcomes. Thirdly, most of the literatures included in this meta-analysis are single arm studies, part of the heterogeneity came from this. Heterogeneity also can be introduced because of methodological differences among studies, including selection bias. The studies about the rate of IVC restenosis, the thrombus clearance rate, the rate of clinical improvement are significant heterogeneity between the selected literatures, but we carried out sensitivity analysis, and none of the inclusive literatures caused great interference to the results of this meta-analysis, which means that these studies have good stability. We also carried out Begg's test for each group and found no publication bias.
In summary, findings from this meta-analysis indicate that the interventional treatment for BCS complicated by IVCT patients is safe and effective with low incidence of PE, high thrombus clearance rate, high technical successful rate of IVC recanalization, good patency, and high clinical improvement rate. Moreover, treatment based on the type and range of the thrombus is proposed.
Conflict of interestThe authors declare no conflict of interest.
This study was supported by National Natural Science Foundation of China (81471769) and the Chinese PLA Scientific Foundation of the Twelve-Five Program (BWS11J028).