Meckel's diverticulum (MD) is a true intestinal diverticulum containing all layers of the small intestine, resulting from the failure of the vitelline duct to obliterate. MD occurs so infrequently that most articles have reported either small series or isolated cases.1 Crohn's disease (CD) is a disorder of uncertain etiology characterized by ulceration and transmural inflammation of the gastrointestinal tract. We present a case in which acid-secreting MD mimic Crohn's ileitis.
Case reportA 21-year-old male presented a 4-day history of gastrointestinal bleeding (passage of bloody stool). He had no significant previous medical history, was on no regular medication, had no allergies known and had no family history of gastrointestinal pathology. He denied abdominal pain, episodes of diarrhea or use of non-steroidal anti-inflammatory drugs.
Physical examination revealed paleness of the skin and mucosae and sinus tachycardia with normal blood pressure. Rectal examination revealed red blood in stools.
Laboratory data showed severe anemia with hemoglobin level of 3.8g/dl. Platelet count, coagulation parameters and inflammatory markers were normal. Nasogastric tube insertion showed a clear aspirate. He required transfusion of 5 units of red blood cells and hemoglobin level raised to 7.7g/dl.
An oesophagogastroduodenoscopy (OGD) was performed, but it was negative. A colonoscopy was also performed and revealed about ten ulcers (<20mm) in the terminal ileum, with red blood in the ileum coming proximally, and digested blood in the colon. Biopsies of the ileum and colon were undertaken.
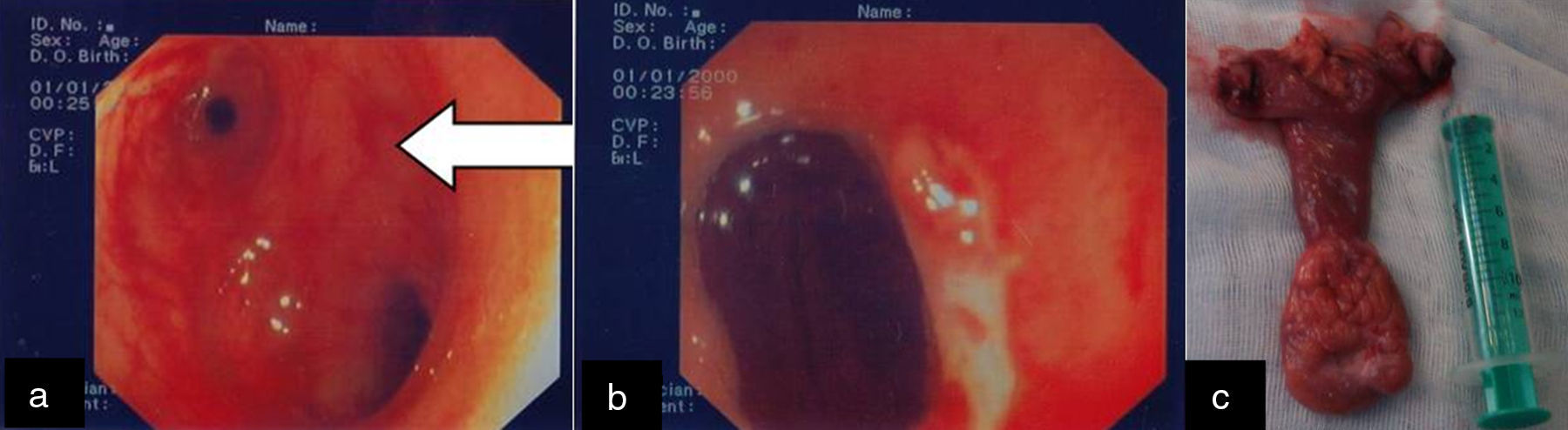
Although hemodynamically stable, he kept bleeding intermittently and had to receive 3 more units of red cells. He underwent a small bowel capsule endoscopy, although this procedure was incomplete, fresh blood was seen in the distal ileum, without identification of any lesion. At this time, a single-balloon enteroscopy (SBE) by anal route was proposed to clarify these findings. It revealed some ulcers in the distal ileum, one of those serpiginous (Fig. 1), with apparent hematin pigmentation and no fresh blood was seen in the lumen. The preliminary diagnosis of regional enteritis (Crohn's disease) was assumed.
However, the patient presented a massive recurrent bleeding within 24h and was decided to perform another SBE. It revealed large amounts of fresh blood not allowing the procedure. The patient became hypovolemic and was submitted to an intraoperative enteroscopy.
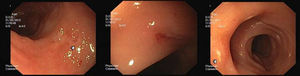
A large Meckel's diverticulum was recognized 80cm from the ileocaecal valve and intraoperative enteroscopy (Fig. 2a) identified a peri-diverticulum ulcer with visible vessel (Fig. 2b), (Anexo-video). An enterectomy with resection of the diverticulum was carried out (Fig. 2c). Pathology confirmed the presence of a Meckel's diverticulum with focal ectopic gastric mucosa.
The patient did well postoperatively, with no recurrent episodes of bleeding, and was discharged seven days after surgery.
Biopsies at first colonoscopy revealed non-specific ileitis. He has since remained asymptomatic.
DiscussionCongenital gastrointestinal malformations make up to 6% of all congenital anomalies and of these MD is the most common.2 MD was described in detail by Hohann Friedrick Meckel in 1808, and bears his name.3
Anatomically MD is a true intestinal diverticulum containing all layers of the small intestine, resulting from the failure of the vitelline duct to obliterate in the first trimester of gestation, in the antimesenteric border of the ileum.2 MD is usually asymptomatic, only about 2–4% develop a complication over the course of their life. The most common complications are hemorrhage, small bowel obstruction, and diverticulitis, which occur more frequently in children rather than in adults. Sixty percent of those who become symptomatic are under 10 years old.4
Hemorrhage is reported in the majority of symptomatic cases of MD in children (over 50% of cases) but is unusual in adult patients (only 11.8%).5 As we show in our case report, bleeding is usually painless and can be massive and fast, presenting fresh red blood in stool. Furthermore, the patient can develop hypovolemic shock.
Heterotopic tissue is present in approximately 50% of resected diverticula, with gastric mucosa being the most common tissue type found (23–50% of cases). The main mechanism of bleeding is the acid secretion from heterotopic gastric mucosae, which leads to ulceration of adjacent ileal mucosa in 62–100% of cases. However ulceration can be seen in cases without gastric heterotopic tissue, and may be explained by either ischemia and/or trauma.5 In our case, the pathology showed gastric mucosa in the MD and our patient presented ulceration of ileal mucosa adjacent to the diverticulum with visible vessel resulting in massive bleeding culminating in hypovolemic shock, being this presentation unusual in this age group.
The traditional diagnostic test of choice for MD has been scintigraphy using 99Tcm pertechnetate with an accuracy of 90% in children. However, in adults the accuracy is only 46%.4
In our case report the presence of multiple ulcers, some of those serpiginous, in the terminal ileum and the fact that single-balloon enteroscopy did not detect MD, conducted to a false hypothesis of inflammatory bowel disease (IBD). Inaccurate diagnoses with single-balloon enteroscopy may result from a small opening of the diverticulum and/or the absence of active bleeding during the procedure or massive active bleeding that influences the endoscopic view.6
Meckel's ileitis is an uncommon manifestation of MD.7 Levesque et al.8 reported in 2011 a case of a 60-year-old man who presented brisk obscure gastrointestinal bleeding and ileal ulcerations on capsule endoscopy, but no pathologic evidence of IBD and who was diagnosed with CD. After an extensive revision of the case a laparoscopy was performed and MD was resected, with resolution of the symptoms. The authors suggest that “Meckel's ileitis” is an alternative diagnosis to CD in patients with gastrointestinal bleeding, ulcerations in capsule endoscopy but no pathologic evidence of CD.8 As far as we know few cases8–10 have been reported, in adults, in which ulcerated MD mimic Crohn's ileitis. Preoperative detection of symptomatic MD requires a high index suspicion, and arrangement of the diagnostic tests.1
The treatment of symptomatic MD is surgical resection. In cases where an inflammatory or ischemic process involves the adjacent ileum, intestinal resection with the diverticulum and anastomosis may be necessary.2 In our case the presence of ileal ulcerations, led to an enterectomy with diverticulectomy, without complications.
In conclusion, the commonest cause of ulceration in the terminal ileum is IBD, however as we demonstrated the rare condition of “Meckel's ileitis” can be misdiagnosed as CD in adults. In cases of isolated small bowel ulceration alternative etiologies to CD should be carefully investigated since IBD treatments carry significant costs and side effects for patients.8 As this case report shows despite being the most prevalent congenital anomaly of the gastrointestinal tract, MD continues to be a diagnostic challenge. Therefore, it is important for clinicians to keep this entity in mind when looking at cases of gastrointestinal bleeding even in adults.
Conflict of interestThe authors declare no conflict of interest.