IgG4-related cholangiopathy is the most common extra-pancreatic manifestation of type 1 autoimmune pancreatitis (AIP) and both fall under the umbrella of systemic IgG4-related disease.1 It is characterised by the appearance of biliary stenosis and the most common presentation is obstructive jaundice (70–80%).1 It is diagnosed through clinical suspicion, imaging tests, serum IgG4 levels and histological analysis.2–4 It is important to rule out a neoplastic origin for the biliary stenosis; hence, cholangioscopy may be very useful, although there are few published data in this regard.5 Treatment with corticosteroids may help to confirm the diagnosis if disease remission is demonstrated.2
We present the case of a 67-year-old patient with the following signs and symptoms for the past two months: steatorrhoeic faeces, early satiety and weight loss. A computed tomography scan showed “sausage pancreas” with peripheral ring enhancement. This typical image, together with serum IgG4 levels twice the upper limit of normal (3110 mg/l [80–1400 mg/l]), confirmed a diagnosis of type 1 AIP3,4 with associated exocrine pancreatic insufficiency. Treatment was therefore started with pancreatic enzymes.
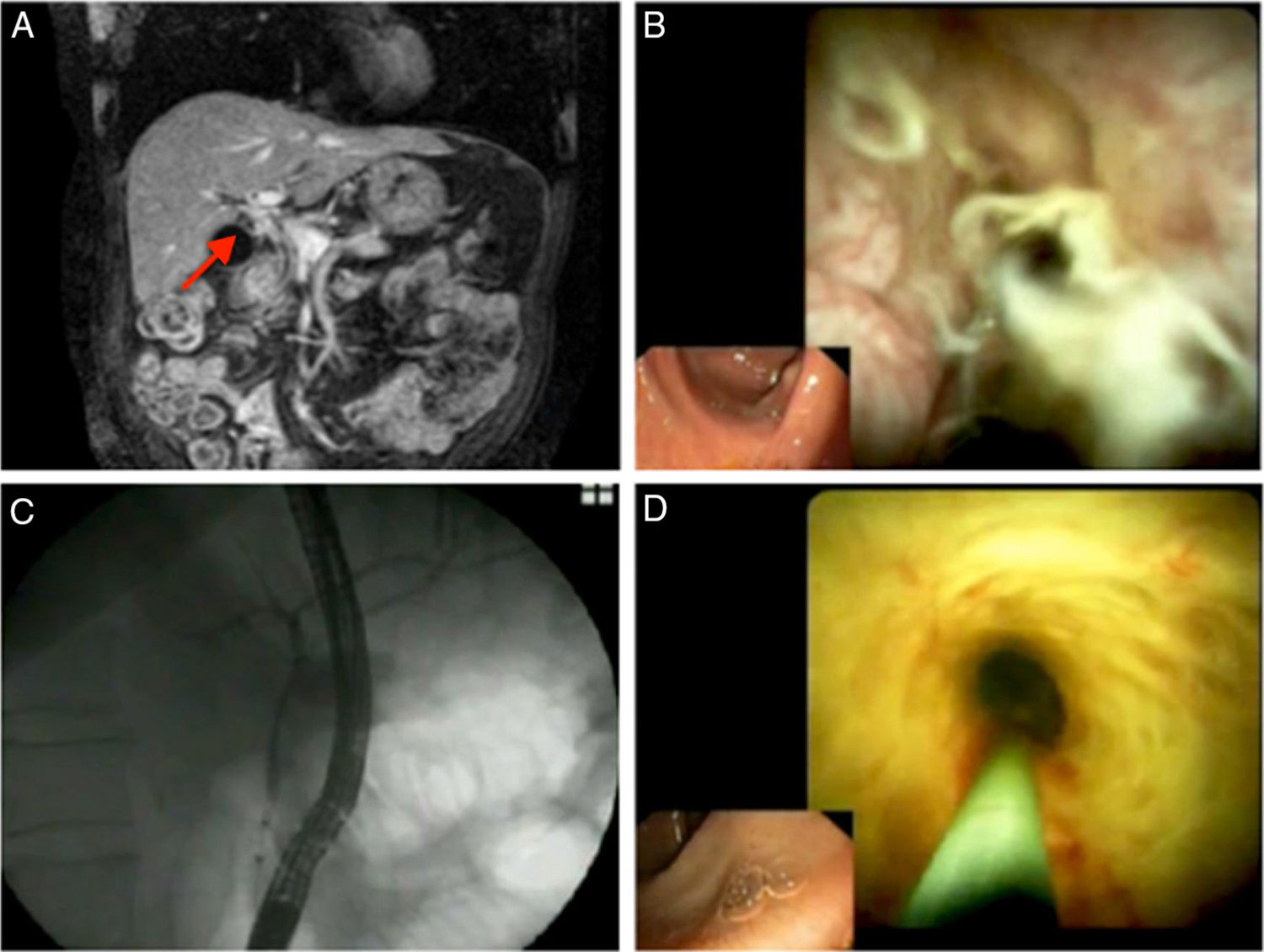
After remaining asymptomatic for 10 months, he went in for epigastric pain which had started three days previously, choluria and 5 kg of weight loss. Laboratory testing revealed increased cholestatic enzymes and transaminases. Three weeks later, his signs and symptoms as well as his laboratory values had improved, and his IgG4 levels were normal (631 mg/l). He underwent magnetic resonance cholangiopancreatography (MRCP) which showed a filiform main pancreatic duct and dilation of the intrahepatic bile duct with no representation of the common hepatic duct (CHD) and adjacent enhancement (Fig. 1). Cholangiocarcinoma could not be ruled out.
(A) Magnetic resonance cholangiopancreatography showing the absence of representation of the common bile duct with contrast enhancement adjacent to its path. (B) First cholangioscopy: image of the common bile duct showing an epithelium with an inflammatory appearance, with diffuse erythema, a papillary–granular pattern and dilated, tortuous vessels. (C) Normal cholangiogram following treatment with corticosteroids. (D) Cholangioscopic image of the common bile duct following treatment showing a “honeycomb” pattern with depressed areas having a fibrotic appearance resulting from scarring.
Endoscopic retrograde cholangiopancreatography (ERCP) revealed several stenoses with dilation of the intrahepatic ducts and filiform stenosis in the CHD. Cytology detected epithelial cells with atypical nuclei initially suggestive of cholangiocarcinoma, although they may also be seen in other inflammatory processes. Ultimately, following review by two pathologists, a diagnosis of cholangiocarcinoma could not be confirmed.
Given the suspicion of cholangiopathy associated with AIP, it was decided to start treatment with oral prednisone (0.6 mg/kg/day). This achieved complete resolution of symptoms and normal laboratory values. However, to rule out cholangiocarcinoma entirely, a cholangioscopy (SpyGlass DS®, Boston Scientific) was performed when treatment was started. This showed the CHD and common bile duct to have erythematous walls, with a papillary–granular pattern and dilated, tortuous vessels (Fig. 1), with a soft consistency on biopsy (SpyBite®, Boston Scientific). Pathology analysis confirmed the absence of malignancy and demonstrated the presence of severe lymphoplasmacytic infiltration, fibrosis of the lamina propria and scant plasma cells with IgG4 (two per high-power field [HPF]).
Four months later, after the cycle of corticosteroids had been completed, ERCP (SpyGlass DS®) was repeated and revealed a strictly normal cholangiogram with disappearance of stenosis and a common bile duct with a “honeycomb” image, with a fibrotic–scarring appearance (Fig. 1).
The presence of biliary stenosis, the prior diagnosis of type 1 AIP and the patient’s improvement with corticosteroids confirmed a diagnosis of IgG4-related cholangiopathy.2
IgG4-related cholangiopathy should be included in the differential diagnosis in cases of masses and biliary stenosis, in which histological analysis is essential to rule out cholangiocarcinoma.2 Initially, most samples were obtained from surgical procedures due to suspicion of tumour disease; now there is greater disease identification and it is possible to perform a cholangioscopy, which enables bile duct biopsies to be taken.5
However, histological confirmation, which requires more than 10 IgG4-positive cells per HPF, may be difficult. There are still limitations due to discontinuous biliary involvement, insufficient samples and a drop in IgG4-positive cells in stages of fibrosis and following treatment.1
To arrive at a diagnosis of IgG4-related cholangiopathy, it is important to correlate histological findings with the patient’s signs and symptoms, serology and imaging tests. If the other criteria are fulfilled, then histological confirmation is not essential for diagnosis. However, it is necessary to rule out cholangiocarcinoma; hence, cholangioscopy plays an important role.
Please cite this article as: Sanahuja Martínez A, Pascual Moreno I, Peña Aldea A, Sánchiz Soler V, Mora Miguel F. Utilidad de la colangioscopia digital en el diagnóstico de la colangiopatía por IgG4 y en la exclusión de colangiocarcinoma. Gastroenterol Hepatol. 2019;42:625–627.