Use of immunosuppressive therapy with thiopurines is very common in inflammatory bowel disease.1,2 We present the case of a submandibular sialadenitis in a patient with Crohn's disease (CD) related to the use of azathioprine (AZA) and mercaptopurine (MP). As this is the first time such a side effect has been reported, we believe it is very important for it to be published.
This was a case of a 39-year-old man with CD diagnosed in September 2016; A2 L3 B1 according to the Montreal classification. In February 2017, as the patient met the criteria for steroid dependence, treatment was started with AZA at a dose of 2.5mg/kg. Two weeks later he went to the emergency department complaining of general malaise and severe submandibular pain. Physical examination detected bilateral inflammation of the submandibular glands and blood analysis showed leucocytosis and hugely elevated C-reactive protein (CRP) at 179mg/l (normal values: <5). The patient was prescribed empirical antibiotic therapy with amoxicillin/clavulanic acid (875/125mg/8h) and prednisone (50mg/day followed by descending regimen for 10 days), the azathioprine was discontinued, and his condition completely improved.
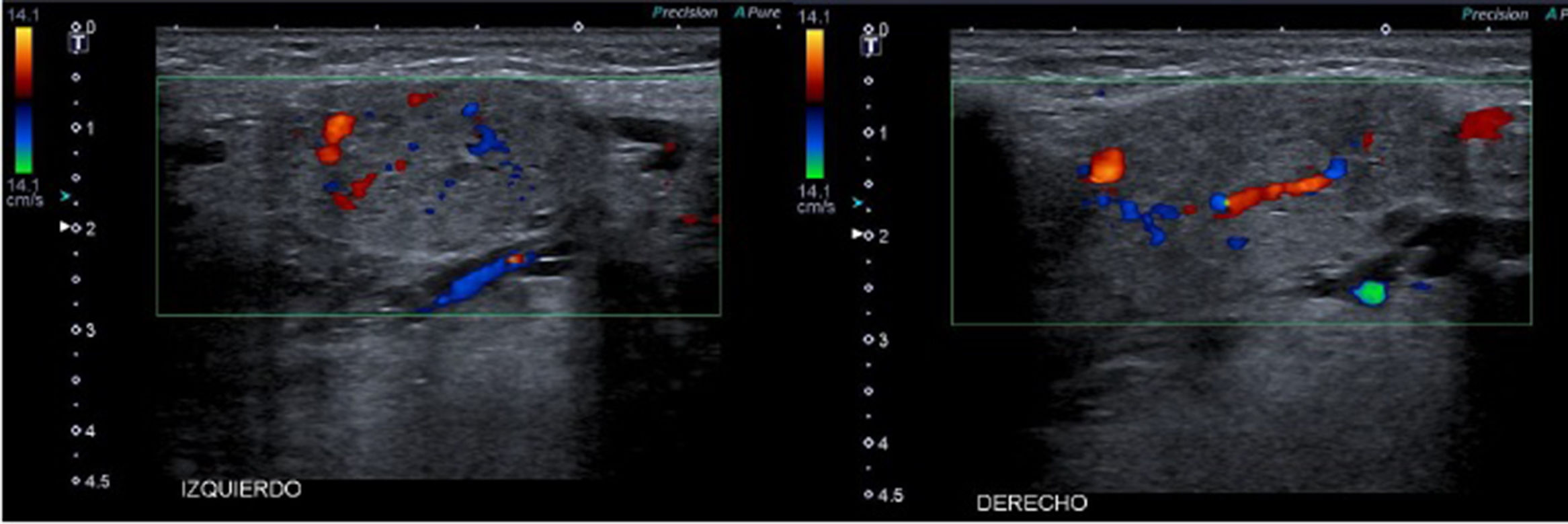
At follow-up, two months later, he was asymptomatic from the ear, nose and throat (ENT) point of view, with no pain and no signs of inflammation in the salivary glands on physical examination. However, he had begun to suffer once again from diarrhoea and right iliac fossa pain, and blood tests showed altered acute phase reactants. It was therefore decided, in the absence of reports of any other cases of sialadenitis with azathioprine, to start treatment with mercaptopurine as an immunomodulator. After the first dose of 50mg of MP, prescribed along with oral budesonide, the patient again developed pain and inflammation in both submandibular glands, with no pyrexia or other signs of infection. Ultrasound showed a bilateral increase in the size of the submandibular glands, with no lithiasis, cysts or other abnormalities (Fig. 1). Serology for mumps virus, cytomegalovirus and Epstein-Barr virus showed past infection, with positive IgG and negative IgM.
The Naranjo algorithm, a useful tool for assessing the causality of an adverse drug reaction, includes data such as the existence of a temporal relationship with the administration of the drug, the resolution after withdrawal of the drug, the recurrence of the adverse effect after re-exposure and the absence of another alternative cause. The score obtained on this scale was 7, which was compatible with probable cause,3 so the decision was made to definitively discontinue the MP. The patient subsequently made satisfactory progress. The patient has been started on biological therapy with infliximab, with good control of his disease and no new complications to date.
DiscussionSide effects related to taking AZA and MP are divided into dose-dependent, such as myelotoxicity, and idiosyncratic, such as acute pancreatitis.4 Up to 17% of patients have to stop treatment as a consequence of pharmacological toxicity.5 The most common cause of acute inflammation of the submandibular glands is sialolithiasis, but other aetiologies include infections, autoimmune or allergic processes and, less frequently, drugs; the condition having been associated with nitrofurantoin, captopril, nifedipine and methimazole.6–8 We have reported the first case related to administration of azathioprine and mercaptopurine; this case should be classified as idiosyncratic and not dose-dependent.
Please cite this article as: Guerra Romero A, Pérez Calle JL, López Serrano P. Submaxilitis aguda secundaria a la toma de azatioprina en paciente con enfermedad de Crohn. Gastroenterol Hepatol. 2018;41:570–571.