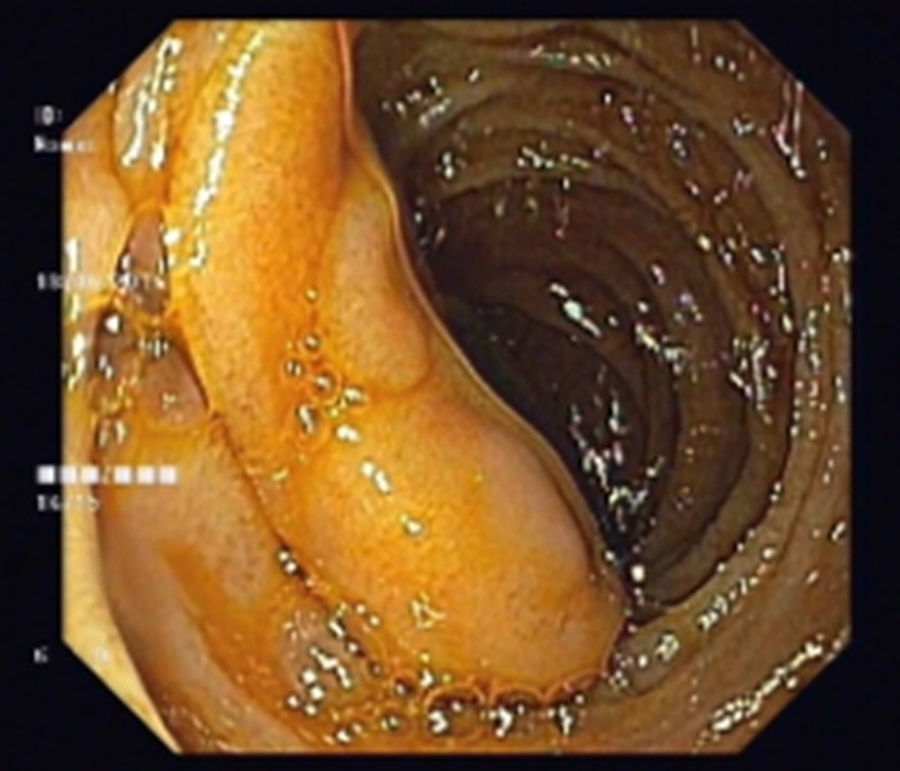
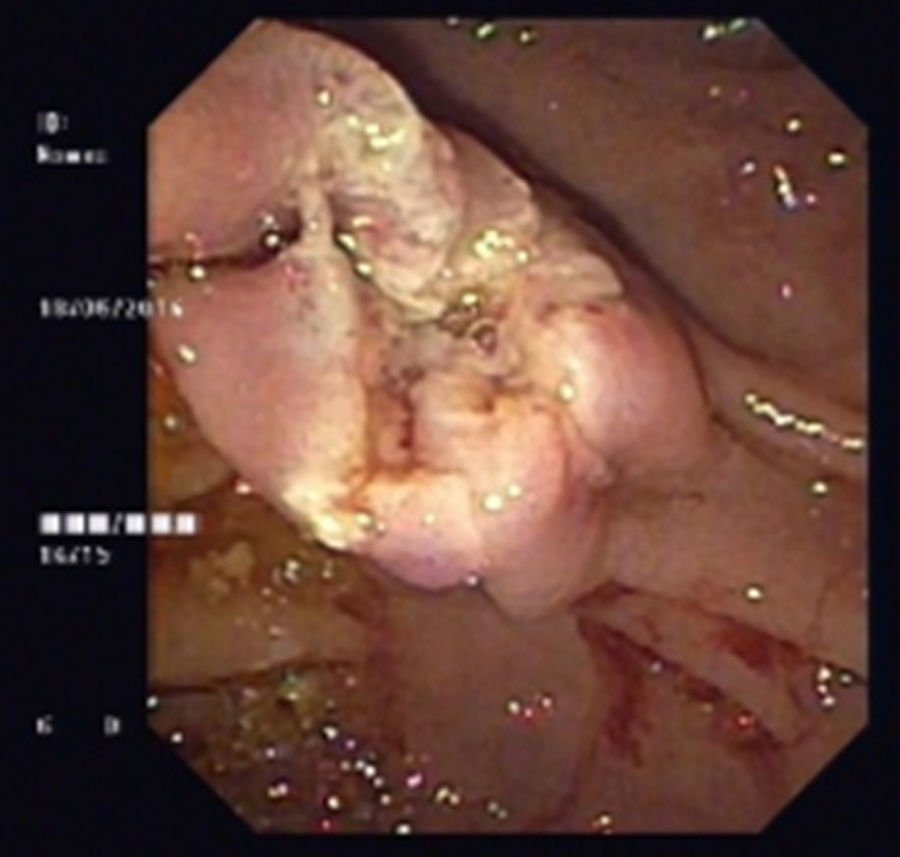
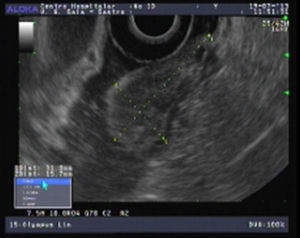
An 80-year-old man was referred to our department due to a duodenal mass found on upper endoscopy, performed for evaluation of ferropenic iron anemia. History taking revealed no particular issues other than antihypertensive medication. He had no abdominal pain, weight or blood loses and his physical examination was uneventful. Laboratory blood tests revealed a hemoglobin of 9.3g/dl, serum iron of 21μg/dl, ferritin of 12.3ng/ml and transferrine of 9.1%. In our department, endoscopic re-evaluation showed, immediately proximal to the ampulla, a 3cm pedunculated and ulcerated subepithelial lesion (Fig. 1). Endoscopic ultrasound (EUS) revealed a well-circumscribed, homogeneous and hypoechoic mass with origin in the submucosal layer, with no lymph nodes (Fig. 2). No lymph node or other organ affection was found on abdominal and pelvic CT. After a multidisciplinary discussion an endoscopic approach was decided. A snare polypectomy was performed (Fig. 3) and the histopathological and immunochemical evaluation revealed a gangliocytic paraganglioma (GP). No evidence of endoscopic and histological recurrence was observed on follow-up EGD after one year. No iron deficiency was present at this time.
GP is a rare submucosal tumor that occurs most frequently in the second portion of the duodenum, near the ampulla of Vater. The most common clinical manifestation is gastrointestinal bleeding (45.1%), followed by abdominal pain (42.8%) and anemia (14.5%).1
There are no endoscopic or echoendoscopic pathognomonic findings of GP. The most common endoscopic features of GPs, such as ulcerations and the presence of a peduncle are also present in other types of submucosal tumors of the duodenum.2 In endoscopic ultrasound (EUS), GP is described as a hypoechoic, heterogeneous tumor with smooth margins, originating from the submucosal layer.3 EUS provides accurate information about the local and regional staging and possibility of local tumor ressection.2
Diagnosis is usually made after surgical or endoscopic resection. Endoscopic biopsy for an accurate diagnosis may be challenging due to the submucosal nature of GP, with a diagnostic rate of 11.4%.1 The characteristic triphasic pattern with a variable mixture of spindle cells, ganglion cells and epithelioid cells is the most important diagnostic feature and is usually appropriate to exclude other potential entities.4
These tumors are considered to be benign. However, there are some cases reporting regional lymph nodes or distant metastasis.5 Surgical excision or endoscopic resection represent available therapeutic alternatives. Most cases reported in literature include surgical treatment.6,7 However, endoscopic resection is increasingly being considered and it is appropriate in most of cases.8 Endoscopic resection is relatively safe and simple when compared surgical resection and it also allows the definite diagnosis of an unknown duodenal mass.2 When clearly pedunculated, even large tumors (more than 2cm) can be resected by endoscopy.2 EUS and CT can define the endoscopic resectability and exclude lymph node involvement and metastatic lesions.
After resection, recurrence has been reported in especially large tumors (>2cm) and in those exceeding the submucosal layer. Specific histologic features to predict malignant potential have not been yet defined. Nevertheless, pancreaticoduodenectomy with lymph node dissection has been proposed as a better option in tumors with nuclear pleomorphism, high mitotic activity, and infiltrative margins.7 Considering the chance of aggressive behavior and the lack of predictive markers, close surveillance is advised.
In this clinical case, endoscopic resection of a 3cm pedunculated tumor with no lymph nodes involvement or metastasis, was possible and safe, avoiding potential morbidity associated with a surgical resection. One year following endoscopic treatment, our patient showed no endoscopic or imaging evidence of tumor recurrence.
Conflict of interestThe authors declare no conflict of interest.