To assess the efficacy and safety of gastric peroral endoscopic myotomy for the treatment of gastroparesis.
MethodsPubMed, Embase, Cochrane Library and Web of Science databases were searched from their earliest records to May 2018. The evaluation of clinical efficacy and safety was based on gastric emptying scintigraphy normalization, the improvement in clinical symptoms and adverse event rate. R 3.5.0 software was used to calculate the pooled estimate rates by meta-analysis. The improvement rate of the Gastroparesis Cardinal Symptom Index score was analyzed at different follow-up times.
ResultsFourteen studies with a total of 276 patients were included in this systematic review. The pooled gastric emptying scintigraphy normalization rate was 61.3% (95% CI, 51.5–70.8%) and clinical symptom improvement rate was 88.2% (95% CI, 83.6–93.1%). Intra-operative complications were found in about 3.2% (95% CI, 0.1–4.2%) of all included patients, and postoperative adverse events in 2.1% (95% CI, 0.3–4.8%). The mean Gastroparesis Cardinal Symptom Index score improvement rate was about 90.2% at one month follow-up, 83.3% at three months, 70.3% at six months, 52.4% at twelve months and 57.1% at eighteen months.
DiscussionOur systematic review demonstrates that gastric peroral endoscopic myotomy is a safe and effective treatment for gastroparesis. Though the short-term outcomes are promising, prospective, randomized, controlled studies with large sample size and long-term follow-up are required to further confirm these results.
Evaluar la eficacia y seguridad de la miotomía endoscópica gástrica por vía oral para el tratamiento de la gastroparesia.
MétodosSe realizaron búsquedas en las bases de datos de PubMed, Embase, Cochrane Library y Web of Science desde sus primeros registros hasta mayo de 2018. La evaluación de la eficacia y la seguridad clínicas se basó en la normalización de la gammagrafía gástrica, la mejora de los síntomas clínicos y la tasa de episodios adversos. Se utilizó el software R 3.5.0 para calcular las tasas de estimación combinadas mediante un metaanálisis. La tasa de mejora de la puntuación del índice de síntomas cardinales de la gastroparesia se analizó en diferentes tiempos de seguimiento.
ResultadosCatorce estudios con un total de 276 pacientes se incluyeron en esta revisión sistemática. La tasa de normalización combinada de la gammagrafía gástrica fue del 61,3% (IC 95% 51,5-70,8) y la tasa de mejoría de los síntomas clínicos fue del 88,2% (IC 95% 83,6-93,1). Se encontraron complicaciones intraoperatorias en, aproximadamente, el 3,2% (IC 95% 0,1-4,2) de todos los pacientes incluidos y los episodios adversos postoperatorios fueron del 2,1% (IC 95% 0,3-4,8%). La tasa de mejora de la puntuación del índice de síntomas cardinales de la gastroparesia media fue de alrededor del 90,2% a un mes de seguimiento, del 83,3% a los 3 meses, del 70,3% a los 6 meses, del 52,4% a los 12 meses y del 57,1% a los 18 meses.
DiscusiónNuestra revisión sistemática demuestra que la miotomía endoscópica gástrica por vía oral es un tratamiento seguro y eficaz para la gastroparesia. Aunque los resultados a corto plazo son prometedores, se requieren estudios prospectivos de distribución aleatoria controlados con un tamaño de muestra grande y un seguimiento a largo plazo para continuar confirmando estos resultados.
Gastroparesis is a chronic motility disorder of the stomach characterized by delayed gastric emptying with no evidence of mechanical obstruction.1 The causes of gastroparesis are multifactorial, including diabetes mellitus (DM), post-surgical intervention, infection, neuropathy, myopathy and unknown etiology (idiopathic).2 Among all, DM is the most common cause, as gastroparesis accounts for more than 50% of DM patients with gastrointestinal symptoms.3 Typical clinical symptoms of gastroparesis include early satiety, nausea, vomiting, bloating, postprandial fullness and abdominal pain.4 Patients with gastroparesis often have a reduced quality of life. Therefore, it is essential to find a safe and effective therapy. Traditional therapies of gastroparesis include the correction of malnutrition and medical treatments such as prokinetic, antiemetic, and analgesic agents.1 However, these medications are often associated with certain side effects that some people may not tolerate, which often lead to suboptimal outcomes. Due to the low therapeutic efficacy and limited medical treatment options, a variety of surgical methods have been developed, such as gastric electrical stimulation, laparoscopic pyloroplasty, botulinum toxin intramuscular pyloric injections, jejunostomy and venting gastrostomy.5–7 A novel endoscopic procedure termed gastric per-oral endoscopic myotomy (G-POEM) was recently introduced for the treatment of gastroparesis.
G-POEM is a minimally invasive endoscopic technique to resect the muscular layer in the pylorus.8 It was initially used for the treatment of achalasia. The first human G-POEM for gastroparesis was successfully performed by Khashab et al. in 2013.8 Following the rapid development of this technique, clinical studies involving about 280 patients have demonstrated that G-POEM is an effective method in managing gastroparesis. However, the reported clinical effective rate and adverse event rate vary across the studies and no consensus on the technical aspects of the procedure has been reached currently. Moreover, many studies possess potential bias as they were not randomized controlled trials and involved only a relatively small number of patients. For a better understanding of the available data, we conducted a systematic review to evaluate the efficacy and safety of G-POEM for gastroparesis.
MethodsSearch strategyA computer-based online search was conducted in PubMed, Embase, Cochrane Library and Web of Science databases from their earliest records to May, 2018. The key words “Gastroparesis” in combination with “Gastric Peroral endoscopic myotomy” or “Pyloromyotomy” and “Endoscopic treatment of gastroparesis” were used in the search. All the retrieved references were hand-searched to find additional eligible studies.
Study selectionThe studies included in this systematic review must meet all the following inclusion criteria: (1) evaluation of the G-POEM treatment of gastroparesis in humans; (2) sufficient data available to calculate the treatment efficiency and incidence of adverse events; (3) written in English or Chinese. Studies published as abstract, full text and conference papers were all included regardless of study design. Of note, considering that some studies were conducted by the same research group, we determined whether a few patients were repeatedly included in different studies by carefully screening the research period, the description of endoscopic procedure and other details. We also communicated with the original authors to get needed information when relevant data were not clearly described.
Data extraction and quality assessmentTwo authors (Hong Zhang and Jiudan Zhang) independently extracted data from each of the included studies and a consensus was achieved for all data collected. The following information was obtained: (1) name of the author; (2) year of publication; (3) country of origin; (4) patients’ characteristics, including number of cases in the study, age, sex, and etiology; (5) study design and use of control; (6) surgical procedure, including mucosotomy site, myotomy length, procedure time, hospitalization days and success rate; (7) GCSI score, half emptying time on GES (HGET) and percent of gastric retention at 4h (RPH4) before and after G-POEM9,10; (8) number of patients with improved clinical symptoms and GES normalization; (9) follow-up period; (10) number of adverse and recurrent events. The main outcomes were clinical effectiveness and safety. All reported intra and post procedure adverse events were documented for safety assessment. GES normalization rate and clinical symptom improvement rate were used as the two main indexes to evaluate the clinical efficacy. GES normalization was defined as <10% retention at 4-hour.9 The improvement of clinical symptoms was measured by different standards in various studies. The GCSI score was the most commonly used indicator,10 which was decreased in eleven studies.11–21 The GCSI score was calculated by averaging the mean score of three subscales: (1) post-prandial fullness/early satiety, (2) nausea/vomiting, and (3) bloating. The definition of the improvement in GCSI score was a decrease in at least one averaged point in the total GCSI score and more than 25% decrease in at least two subscales.10 In contrast to GCSI score, other methods were used in some of the studies, for example, Malik et al.22 used the Clinical Patient Grading Assessment Score (CPGAS), Khashab et al.23 used a patient's self-reporting system to document the amount of gastroparetic symptoms and recurrent hospitalization, and Shlomovitz et al.24 used a gastroparesis symptom monitor worksheet (Medtronic, Minneapolis, MN-GSMK) to evaluate the severity and frequency of gastroparesis symptoms. The Quality Assessment Tool for Case Series Studies from the National Institutes of Health (NIH) was used to evaluate the quality of including studies.25 We analyzed nine quality parameters mentioned in the checklist to assess the quality of each study.
Statistical synthesisR 3.5.0 software was used to determine the pooled estimate rate of GES normalization, clinical symptom improvement and adverse event in reported studies by meta-analysis. Heterogeneity was assessed using the I2 test with a significance level set at I2 over 50%. If there was no heterogeneity (I2<50%), we selected the fixed effect model. Otherwise, the random effects model was used. Publication bias was explored using the Egger's test. Sensitivity analysis was performed by separately removing each single study. We also analyzed the improvement of GCSI score, HGET and RPH4 after G-POEM, by describing the mean, minimum and maximum values.
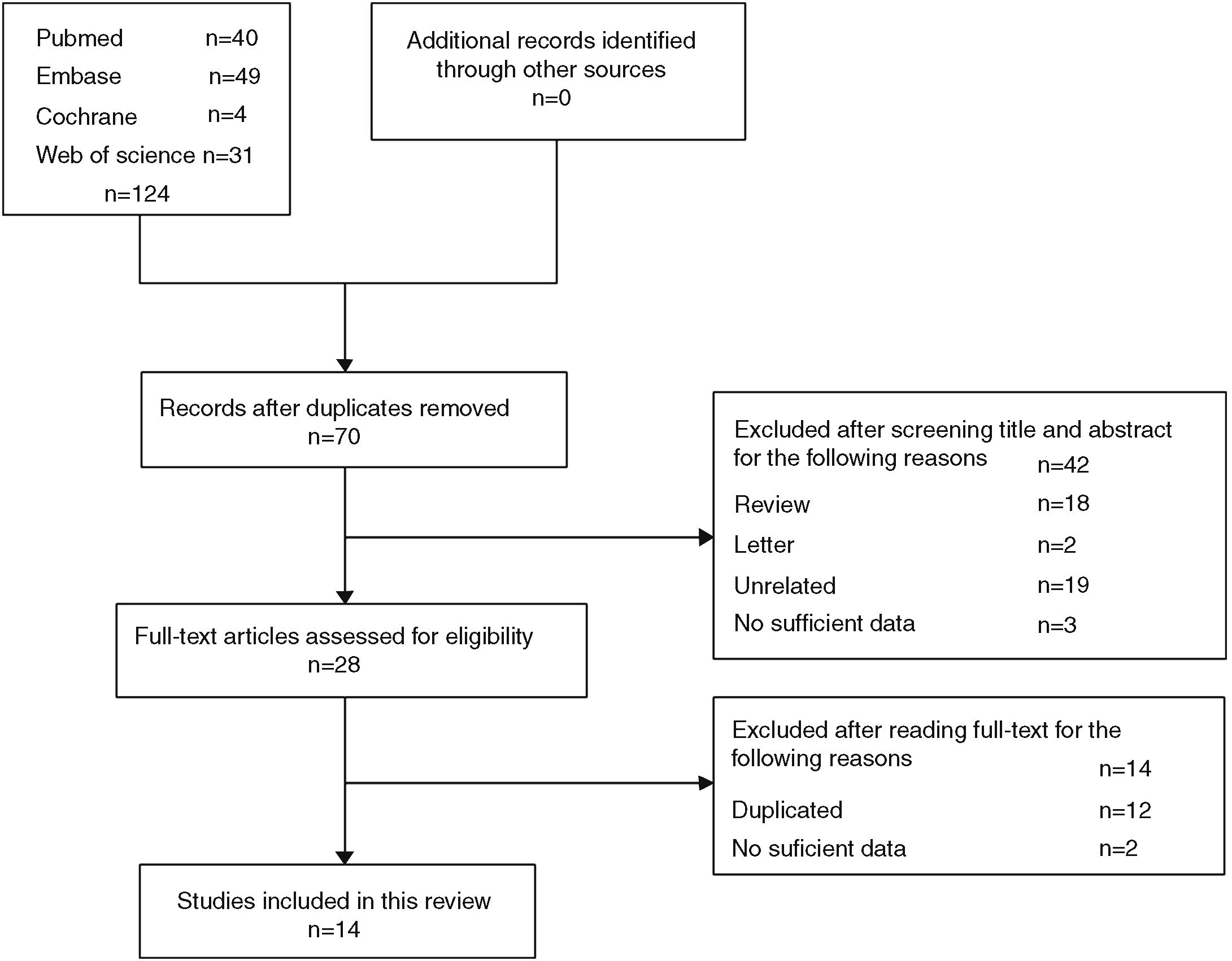
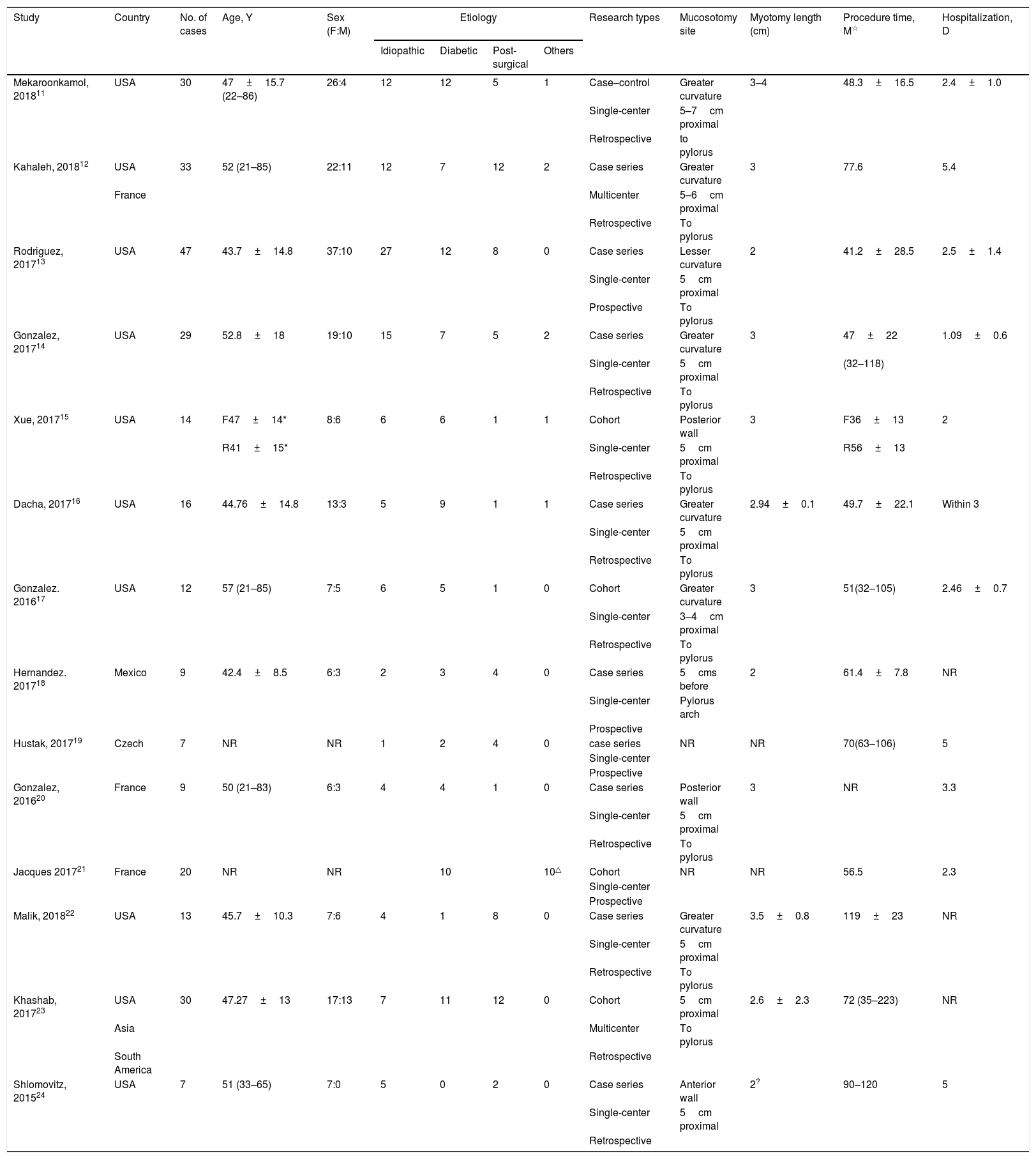
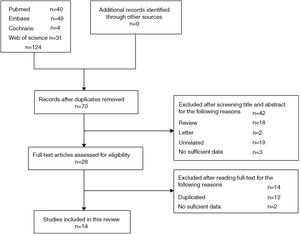
ResultsDescription of studiesA total of 124 studies were initially identified from the literature search and fourteen studies11–24 (276 patients) were eligible for this systematic review. The search process is summarized in Fig. 1. Among the fourteen studies, there were nine case series,12–14,16,18–20,22,24 four cohort studies with no controlled group15,17,21,23 and one case–control study.11 Characteristics of the studies are summarized in Table 1. As mentioned in twelve studies,11–18,20,22–24 the mean age of the patients in each study ranged from 42.4 to 57 years old and 175 (70.3%) of 249 patients were female. The etiology of gastroparesis varied, there were 106 (38.4%) idiopathic gastroparesis, 89 (32.2%) diabetic, 64 (23.2%) post-surgical and 10 (3.6%) classed as “others”, for example, post-infection and scleroderma. Ten patients21 were classified as non-diabetic gastroparesis but the specific etiology was unknown.
Characteristics of the included studies.
| Study | Country | No. of cases | Age, Y | Sex (F:M) | Etiology | Research types | Mucosotomy site | Myotomy length (cm) | Procedure time, M☆ | Hospitalization, D | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Idiopathic | Diabetic | Post-surgical | Others | ||||||||||
| Mekaroonkamol, 201811 | USA | 30 | 47±15.7 (22–86) | 26:4 | 12 | 12 | 5 | 1 | Case–control | Greater curvature | 3–4 | 48.3±16.5 | 2.4±1.0 |
| Single-center | 5–7cm proximal | ||||||||||||
| Retrospective | to pylorus | ||||||||||||
| Kahaleh, 201812 | USA | 33 | 52 (21–85) | 22:11 | 12 | 7 | 12 | 2 | Case series | Greater curvature | 3 | 77.6 | 5.4 |
| France | Multicenter | 5–6cm proximal | |||||||||||
| Retrospective | To pylorus | ||||||||||||
| Rodriguez, 201713 | USA | 47 | 43.7±14.8 | 37:10 | 27 | 12 | 8 | 0 | Case series | Lesser curvature | 2 | 41.2±28.5 | 2.5±1.4 |
| Single-center | 5cm proximal | ||||||||||||
| Prospective | To pylorus | ||||||||||||
| Gonzalez, 201714 | USA | 29 | 52.8±18 | 19:10 | 15 | 7 | 5 | 2 | Case series | Greater curvature | 3 | 47±22 | 1.09±0.6 |
| Single-center | 5cm proximal | (32–118) | |||||||||||
| Retrospective | To pylorus | ||||||||||||
| Xue, 201715 | USA | 14 | F47±14* | 8:6 | 6 | 6 | 1 | 1 | Cohort | Posterior wall | 3 | F36±13 | 2 |
| R41±15* | Single-center | 5cm proximal | R56±13 | ||||||||||
| Retrospective | To pylorus | ||||||||||||
| Dacha, 201716 | USA | 16 | 44.76±14.8 | 13:3 | 5 | 9 | 1 | 1 | Case series | Greater curvature | 2.94±0.1 | 49.7±22.1 | Within 3 |
| Single-center | 5cm proximal | ||||||||||||
| Retrospective | To pylorus | ||||||||||||
| Gonzalez. 201617 | USA | 12 | 57 (21–85) | 7:5 | 6 | 5 | 1 | 0 | Cohort | Greater curvature | 3 | 51(32–105) | 2.46±0.7 |
| Single-center | 3–4cm proximal | ||||||||||||
| Retrospective | To pylorus | ||||||||||||
| Hernandez. 201718 | Mexico | 9 | 42.4±8.5 | 6:3 | 2 | 3 | 4 | 0 | Case series | 5cms before | 2 | 61.4±7.8 | NR |
| Single-center | Pylorus arch | ||||||||||||
| Prospective | |||||||||||||
| Hustak, 201719 | Czech | 7 | NR | NR | 1 | 2 | 4 | 0 | case series | NR | NR | 70(63–106) | 5 |
| Single-center | |||||||||||||
| Prospective | |||||||||||||
| Gonzalez, 201620 | France | 9 | 50 (21–83) | 6:3 | 4 | 4 | 1 | 0 | Case series | Posterior wall | 3 | NR | 3.3 |
| Single-center | 5cm proximal | ||||||||||||
| Retrospective | To pylorus | ||||||||||||
| Jacques 201721 | France | 20 | NR | NR | 10 | 10△ | Cohort | NR | NR | 56.5 | 2.3 | ||
| Single-center | |||||||||||||
| Prospective | |||||||||||||
| Malik, 201822 | USA | 13 | 45.7±10.3 | 7:6 | 4 | 1 | 8 | 0 | Case series | Greater curvature | 3.5±0.8 | 119±23 | NR |
| Single-center | 5cm proximal | ||||||||||||
| Retrospective | To pylorus | ||||||||||||
| Khashab, 201723 | USA | 30 | 47.27±13 | 17:13 | 7 | 11 | 12 | 0 | Cohort | 5cm proximal | 2.6±2.3 | 72 (35–223) | NR |
| Asia | Multicenter | To pylorus | |||||||||||
| South America | Retrospective | ||||||||||||
| Shlomovitz, 201524 | USA | 7 | 51 (33–65) | 7:0 | 5 | 0 | 2 | 0 | Case series | Anterior wall | 2? | 90–120 | 5 |
| Single-center | 5cm proximal | ||||||||||||
| Retrospective | |||||||||||||
NR: not reported; ☆: minute.
*F: Fluoroscopy-guided G-POEM Group (N=7);*R: Routine G-POEM Group (N=7).
△:10 patients were described as non-diabetic gastroparesis but the specific etiology was unknown.
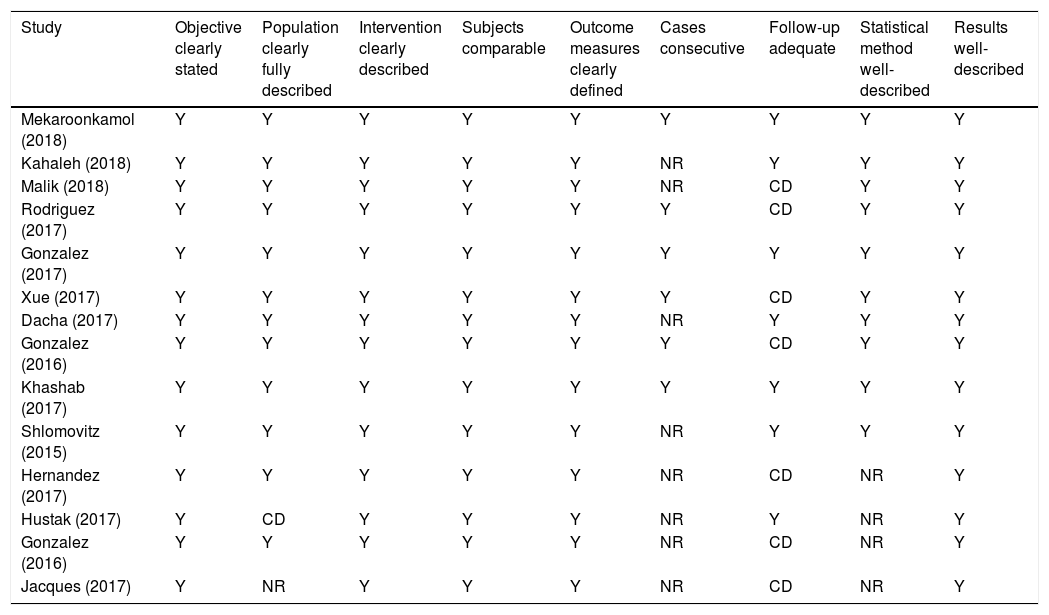
Quality assessment was summarized in Table 2. All of the included studies clearly described the objective, intervention, outcome measures and results. Among them, twelve studies11–18,20,22–24 had a full and clear description of the studied population. Ten studies11–17,22–24 mentioned statistical methods. Six studies11,13–15,17,23 enrolled patients consecutively and seven studies11,12,14,16,19,23,24 had more than three months follow-up period.
Quality assessment.
| Study | Objective clearly stated | Population clearly fully described | Intervention clearly described | Subjects comparable | Outcome measures clearly defined | Cases consecutive | Follow-up adequate | Statistical method well-described | Results well-described |
|---|---|---|---|---|---|---|---|---|---|
| Mekaroonkamol (2018) | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Kahaleh (2018) | Y | Y | Y | Y | Y | NR | Y | Y | Y |
| Malik (2018) | Y | Y | Y | Y | Y | NR | CD | Y | Y |
| Rodriguez (2017) | Y | Y | Y | Y | Y | Y | CD | Y | Y |
| Gonzalez (2017) | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Xue (2017) | Y | Y | Y | Y | Y | Y | CD | Y | Y |
| Dacha (2017) | Y | Y | Y | Y | Y | NR | Y | Y | Y |
| Gonzalez (2016) | Y | Y | Y | Y | Y | Y | CD | Y | Y |
| Khashab (2017) | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Shlomovitz (2015) | Y | Y | Y | Y | Y | NR | Y | Y | Y |
| Hernandez (2017) | Y | Y | Y | Y | Y | NR | CD | NR | Y |
| Hustak (2017) | Y | CD | Y | Y | Y | NR | Y | NR | Y |
| Gonzalez (2016) | Y | Y | Y | Y | Y | NR | CD | NR | Y |
| Jacques (2017) | Y | NR | Y | Y | Y | NR | CD | NR | Y |
Y: yes; NR: not reported; CD: cannot decide.
All studies included in the systematic review had an 100% technical success rate. Technical details of G-POEM are described in Table 1. The length of average procedure time ranged from 41.2 to 119min in different studies and hospitalization days were from 1.09 to 5 days. The mucosotomy site and myotomy incision length varied across the studies. The most common incision site was the greater curvature (50%), followed by the anterior wall, posterior wall and lesser curvature. The distance between the mucosal incision site and the pylorus ranged from 3 to 7cm. The myotomy incision length ranged from 2 to 3.5cm in different studies.
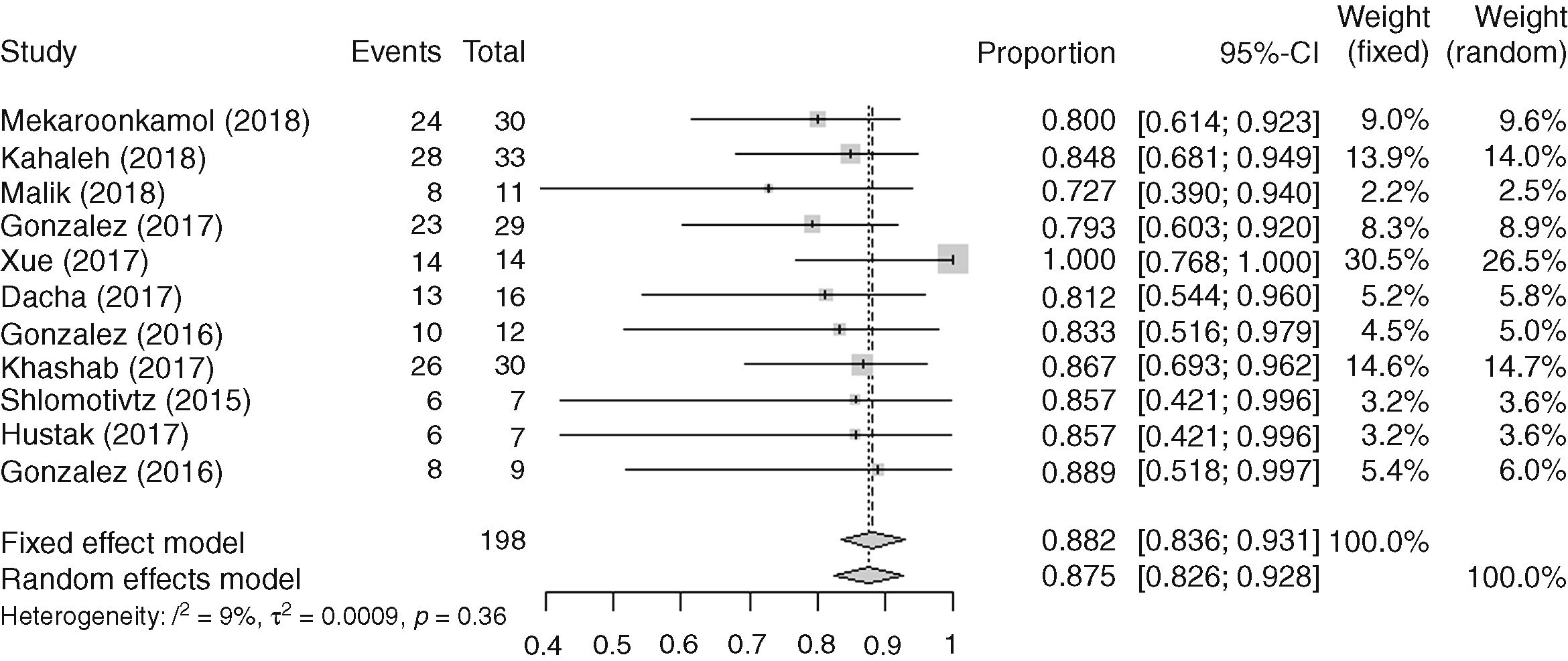
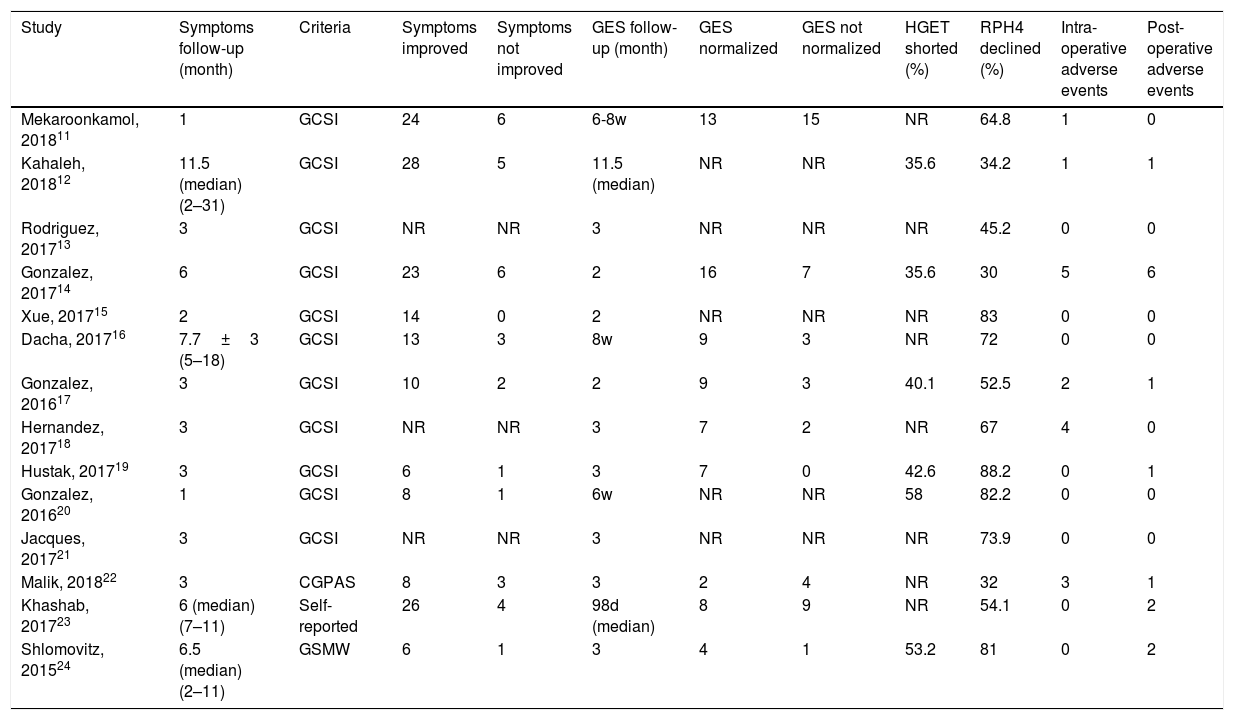
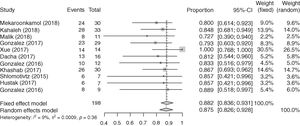
Clinical efficacyGES normalization and clinical symptom improvement were considered as the two main indicators for clinical efficacy (Table 3). In nine studies11,14,16–19,22–24 involving 119 patients, GES normalization occurred in 75 (63%) patients at two or three months post G-POEM. The GES normalization rate ranged from 33.3% to 100% in various studies. The pooled estimate of GES normalization rate determined by meta-analyses was 67.2% (95% CI, 53.0–80.1%). The heterogeneity between the studies was statistically significant (I2>50%). We therefore did a sensitivity analysis and omitted the study by Hustak et al.19 since it contributed to the heterogeneity significantly. After that, the pooled GES normalization rate was 61.3% (95% CI, 51.5–70.8%). Eleven studies11,12,14–17,19,20,22–24 including 198 patients had improved clinical symptoms in 166 (83.8%) patients during the one to eighteen months follow-up period after G-POEM. The symptom improvement rate ranged from 72.7% to 100% and the pooled improvement rate was 88.2% (95% CI, 83.6–93.1%). There was no heterogeneity between the studies (I2<50%) (Fig. 2).
The values of clinical efficacy and safety.
| Study | Symptoms follow-up (month) | Criteria | Symptoms improved | Symptoms not improved | GES follow-up (month) | GES normalized | GES not normalized | HGET shorted (%) | RPH4 declined (%) | Intra-operative adverse events | Post-operative adverse events |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mekaroonkamol, 201811 | 1 | GCSI | 24 | 6 | 6-8w | 13 | 15 | NR | 64.8 | 1 | 0 |
| Kahaleh, 201812 | 11.5 (median) (2–31) | GCSI | 28 | 5 | 11.5 (median) | NR | NR | 35.6 | 34.2 | 1 | 1 |
| Rodriguez, 201713 | 3 | GCSI | NR | NR | 3 | NR | NR | NR | 45.2 | 0 | 0 |
| Gonzalez, 201714 | 6 | GCSI | 23 | 6 | 2 | 16 | 7 | 35.6 | 30 | 5 | 6 |
| Xue, 201715 | 2 | GCSI | 14 | 0 | 2 | NR | NR | NR | 83 | 0 | 0 |
| Dacha, 201716 | 7.7±3 (5–18) | GCSI | 13 | 3 | 8w | 9 | 3 | NR | 72 | 0 | 0 |
| Gonzalez, 201617 | 3 | GCSI | 10 | 2 | 2 | 9 | 3 | 40.1 | 52.5 | 2 | 1 |
| Hernandez, 201718 | 3 | GCSI | NR | NR | 3 | 7 | 2 | NR | 67 | 4 | 0 |
| Hustak, 201719 | 3 | GCSI | 6 | 1 | 3 | 7 | 0 | 42.6 | 88.2 | 0 | 1 |
| Gonzalez, 201620 | 1 | GCSI | 8 | 1 | 6w | NR | NR | 58 | 82.2 | 0 | 0 |
| Jacques, 201721 | 3 | GCSI | NR | NR | 3 | NR | NR | NR | 73.9 | 0 | 0 |
| Malik, 201822 | 3 | CGPAS | 8 | 3 | 3 | 2 | 4 | NR | 32 | 3 | 1 |
| Khashab, 201723 | 6 (median) (7–11) | Self-reported | 26 | 4 | 98d (median) | 8 | 9 | NR | 54.1 | 0 | 2 |
| Shlomovitz, 201524 | 6.5 (median) (2–11) | GSMW | 6 | 1 | 3 | 4 | 1 | 53.2 | 81 | 0 | 2 |
NR: not reported; GES: gastric emptying scintigraphy; HGET: half emptying time on gastric emptying scintigraphy; RPH4: gastric retention at 4h.
As the follow-up period varied among the studies, the GCSI improvement rate and the decreasing percentage of mean GCSI score were analyzed according to the length of the follow-up period. Four studies11,15,17,20 had an improved GCSI score in less than three months follow-up period and the improvement rate ranged from 80% to 100% with a mean of 90.2%. Three studies 14,17,19 with a three months follow-up reported the GCSI score improvement rate ranged from 79.3% to 85.7% with a mean of 82.8%. Two studies11,14 with a six months follow-up reported the improvement rate being 69.2% and 71.4%, respectively. In the study by Mekaroonkamol et al.,11 the improvement rate was reported as 52.4% and 57.1% at twelve months and eighteen months, respectively. This was the longest follow-up reported in all the published studies to date. Several studies11–22 described the mean GCSI score before and after G-POEM. The mean percentage decrease in GCSI score was of 60.4% with a range of 48.6–74.3% at one month after G-POEM, 60.8% at three months (range of 28.3–73.3%), 60.0% at six months (range of 45.7–70%). Only two studies11,16 had a follow up at twelve months and the decrease in GCSI score was 25.7% and 57%, respectively. In addition, the study by Mekaroonkamol and colleagues showed a 40% decrease in GCSI score at eighteen months. When the follow-up was more than three months, the median decrease of nausea, vomiting, early satiety, post-prandial fullness and bloating score was 59.4%, 69.1%, 65.2%, 53.5% and 36.3%, respectively.
Other indicators could also reflect the effectiveness of clinical treatment (Table 3). The half gastric emptying time before and after G-POEM was mentioned in six studies.12,14,17,19,20,24 The shortened percentage of half emptying time ranged from 35.6% to 58% in different studies. All fourteen studies described a decrease on gastric retention time post procedure, ranging from 30% to 88.2% (median). Changes in body mass index (BMI) were reported in three studies,11,14,16 two11,16 being increased in the mean BMI by 2.68% and 5.96% respectively and one14 displaying a 9.19% decrease in BMI.
Adverse eventsFourteen patients in six studies11,12,14,17,18,22 developed sixteen intra-operative complications (Table 3), including five capnoperitoneum, two pneumoperitoneum, two accidental mucosotomy, one tension capnoperitoneum, one intraoperative incision site bleeding and rest with self-limited unspecified complications. The remaining eight studies13,15,16,19–21,23,24 did not develop any intra-operative complications. In general, the rate of the intra-operative complications in the original studies ranged from 0% to 44.4% and the pooled rate measured by meta-analysis was 3.2% (95% CI, 0.1–8.6%). The heterogeneity between studies was statistically significant (I2>50%). Following sensitivity analysis, we removed the result obtained from Hernandez et al.18 as it contributed the most to the heterogeneity. Therefore, the pooled rate was revised as 1.6% (95% CI, 0.1–4.2%). Fourteen post-operative adverse events were observed in seven studies (Table 3),12,14,17,19,22–24 occurring in less than two weeks after G-POEM in most cases. Of the adverse events, there were four abdominal pain, three ulcer, three bleeding, and others such as difficulty swallowing, capnoperitoneum, stricture (occurred at three months after the procedure) and pulmonary embolism. The rest of the seven studies11,13,15,16,18,20,21 did not have any post-operative adverse events, among them two followed up for more than one month. The rate of adverse post-operative events ranged from 0% to 28.6% in different studies and the pooled rate was 2.1% (95% CI, 0.3–4.8%). The heterogeneity between studies was not statistically significant (I2<50%).
RecurrenceAmong all studies, four patients in three studies13,14,20 developed recurrent gastroparesis, presenting as gastrointestinal symptoms re-occurred in one to nine months post procedure. The follow-up time ranged from one to nine months. One study12 clearly indicated that no patients needed a repeat endoscopic therapy post G-POEM during the median of 11.5 months follow-up period. Two studies16,23 also declared that none of the patients required re-hospitalization during the median of 6.5 and 7.7 months of follow-up, respectively.
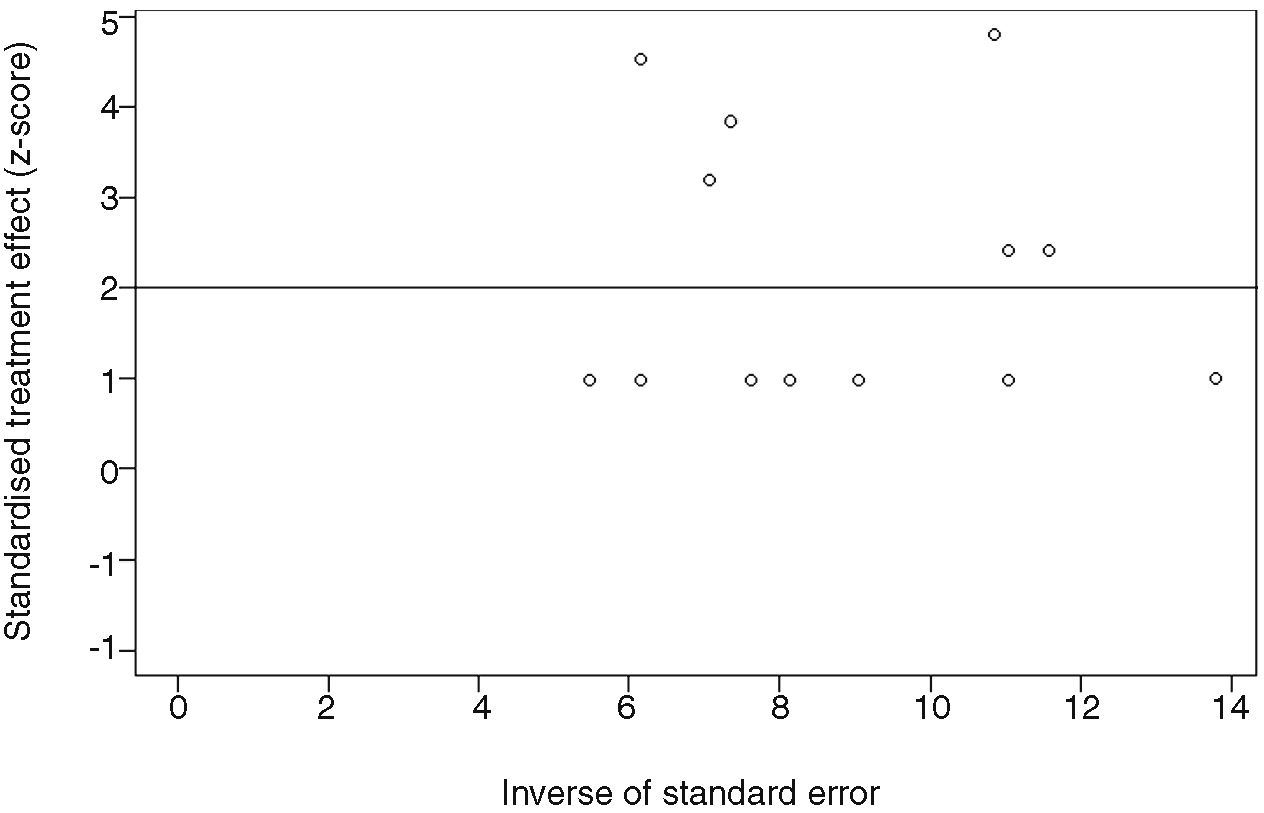
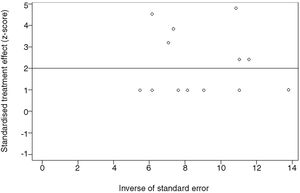
Publication biasThe Egger's test was conducted to investigate publication bias in fourteen studies on intra-operative complications (Fig. 3). The data were symmetrical, indicating a lack of substantial publication bias (P=0.18).
DiscussionGastroparesis remains a clinically challenging disease for which current therapeutic strategies are far from satisfactory. G-POEM, as a novel endoscopic procedure, was technically feasible and yielded promising clinical results in managing gastroparesis patients in multiple studies.11–24
Our meta-analysis demonstrated that G-POEM is an effective treatment in controlling gastroparesis, which is consistent with the previous literature. It was reported in a recent published systematic review that GES normalized in about 55.5% patients and GCSI improved in about 81.5% of gastroparesis patients after G-POEM.26 Our result is similar to that report despite we used meta-analysis statistically while averaging the values of all the eligible studies was used in that review. Furthermore, G-POEM was more effective when compared to other therapies. For example, comparing with placebo (saline inject) in recent randomized controlled studies, the intra-pyloric injection of botulinum toxin had failed to confirm its efficacy.27,28 Transpyloric stenting of the pylorus was clinically effective in 75% patients, but the stent migration occurred in up to 50% patients during follow-up, limiting its long-term efficacy.29 Whereas, as a promising outcome in our study, the rate of improvement at six months was about 70%. Since the number of follow-up cases longer than six months was relatively low in our meta-analysis, further larger scale and longer follow-up studies are essential to validate the results.
Patients with gastroparesis should be substratified according to the etiology, gender and clinical presentation since patients in some groups may benefit more from G-POEM. As mentioned, patients who suffered from nausea, vomiting, early satiety or post-prandial fullness may display better improvement than those with bloating alone after G-POEM, however the exact mechanisms remain unclear. A number of studies suggested that diabetes and female gender were associated with poor responses to G-POEM, which could be the result of diabetic involvement in both stomach and small intestine.14,16 Other studies showed that patients with pylorospasm may have a high possibility of responding to G-POEM.11,16,22 Measurements including Endoscopic Functional Luminal Imaging Probe (EndoFLIP) of the pylorus or pyloric distensibility and transpyloric pressure can serve as markers to identify patients with pylorospasm.16,22 Considering the multifactorial nature of the gastroparesis, it is beneficial to perform a subgroup analysis of treatment efficacy based on gender, etiology and the major symptoms in future studies.
The G-POEM procedure was feasible as no technical failure was reported in all included studies. The mean procedure time was less than two hours. G-POEM was also a safe technique when compared to other interventional therapies. For instance, similar to our result, Hibbard et al.30 reported that laparoscopic pyloroplasty, an invasive and more complicated procedure in managing gastroparesis yielded an 86% improvement in symptomatic control. However, the laparoscopic pyloroplasty was often accompanied with more severe postoperative complications than G-POEM, such as gastric leak. Most intra and post G-POEM adverse events were mild to moderate, and manageable. For example, capnoperitoneum could be easily treated by abdominal paracentesis, while minor bleeding and pain could be relieved spontaneously. Since the data published on G-POEM was limited, the adverse events of Per Oral Endoscopic Myotomy (POEM), a technology similar to G-POEM would be discussed. Haito Chavez et al.31 analyzed 1826 cases of POEM and reported an overall 7.5% prevalence of adverse events and 0.5% severe adverse events. Most of POEM-related adverse events were mild to moderate and self-limited. Severe adverse events included perforation, major bleeding, cardiac arrhythmia, capnomediastinum, empyema, esophageal leak and pneumonia. In that study, only four patients required surgery to control the complications and there was no lethal adverse event. The adverse event predictive factors were considered as endoscopists’ experience, patients’ clinical characteristics, the use of a Triangular tip knife, a sigmoid-type esophagus and the use of an electrosurgical current.31
Though this systematic review showed promising results for gastroparesis treatment, there were several limitations. Firstly, only one study had a control group. Thus, the clinical efficacy and safety rates obtained may be influenced by some other potential factors, such as etiology, duration of gastroparesis and previous treatments. Secondly, among the fourteen included studies, twelve were single-center studies and some were conducted by the same group in one country. In addition, most were retrospective studies, which may result in selection bias. Thirdly, the sample size of each study was relatively small and the evaluation of the improvement in gastrointestinal symptoms were not standardized. Furthermore, the duration of follow-up periods varied in each study. All these factors may led to heterogeneity in the meta-analysis. Therefore, definitive conclusions regarding the safety and efficacy of G-POEM remain to be drawn.
In conclusion, G-POEM represents a safe and effective treatment option for gastroparesis. Though the short term outcomes are promising, prospectively randomized controlled studies with larger sample size and longer follow-up are required to validate these findings in the near future.
Conflict of interestThe authors declare no conflicts of interest.