Idiopathic ischaemic enteritis is an irreversible lesion of the mucosa induced by intestinal ischaemia, without evidence of mesenteric artery occlusion.1,2 It is considered to be caused by hypoperfusion of the mesenteric vessels, without an explanatory structural, obstructive or inflammatory cause. The most common form of presentation is an inflammatory stricture.
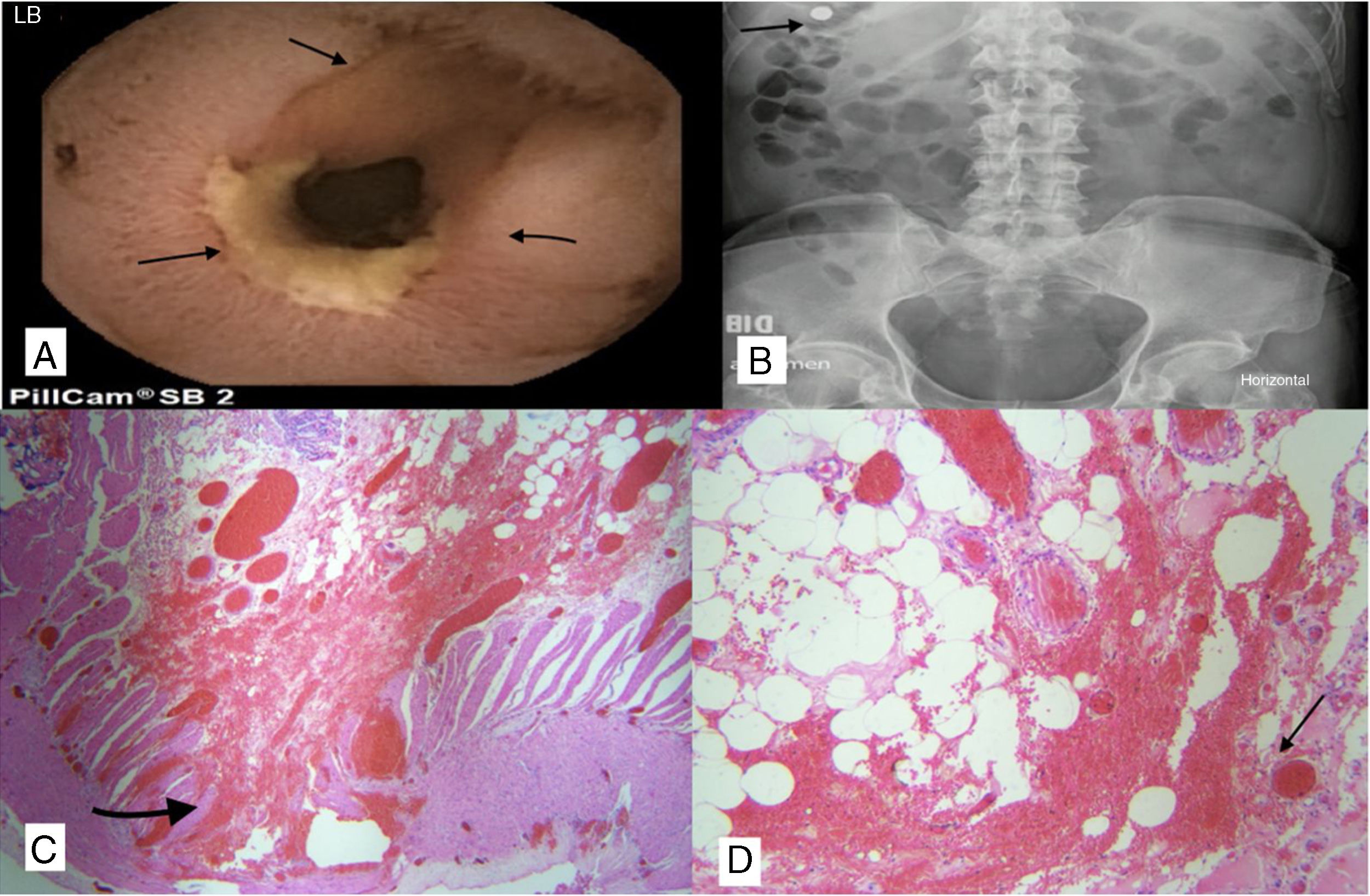
We present the case of a 59-year-old male with a history of hypertension, who denied alcohol or NSAID use or being a smoker. He had been assessed several times in Accident and Emergency for gastrointestinal bleeding manifested by melaena. Tests showed him to have iron deficiency anaemia (haemoglobin: 5.1g/dl, total iron: 15μg/dl and ferritin: 27ng/ml). Endoscopic studies (two oesophagogastroduodenoscopies and one colonoscopy) were reported as normal. Video capsule endoscopy (VCE) showed an ulcerated inflammatory lesion in the proximal ileum which was generating a concentric stricture, with estimated residual lumen of 30% in that area (Fig. 1A); the VCE was retained at the level of the stricture (Fig. 1B) for 72h. The patient had colicky pain and distension, but no vomiting. We performed a retrograde double-balloon enteroscopy but, as we were unable to reach the site of the stricture, laparoscopic surgery was scheduled. Local resection of the diseased segment was performed with end-to-end anastomosis, without intraoperative complications. Intraoperatively, the surgeons found a hard area of about 5cm of fibrotic strictures with marked local inflammation, so Crohn's disease (CD) was suspected. Histopathology showed chronic inflammation of the ileum with submucosal and serous fibrosis, muscle hypertrophy and marked vascular congestion, compatible with active chronic ileitis of ischaemic aetiology (Fig. 1C and D), but no findings suggestive of CD or malignancy. Special staining methods were used on the tissue, such as Ziehl-Neelsen, methenamine silver, PAS and Gram, all of which were negative, as was immunohistochemistry for cytomegalovirus, ruling out infectious causes. Further tests were carried out, including nuclear antibodies (anti-cytoplasmic antibodies, which were negative), enabling systemic vasculitis to be ruled out. CT-angiogram of the abdomen showed no thrombi or other vascular lesions, ruling out mesenteric ischaemic disease, and faecal calprotectin was normal, making CD unlikely, as it has a high negative predictive value. The patient made a satisfactory recovery, with no new episodes of bleeding or anaemia after surgery. At the 12-month follow-up, the patient was asymptomatic and not on any medication.
(A) Capsule endoscopy showing severe stenosis, with fibrotic appearance, ulcerated and covered with fibrin. (B) Simple X-ray of abdomen: retained capsule on day three post-ingestion. (C and D) Fibrotic ulcer with submucosal, serous inflammation, severe vascular congestion and hypertrophy of the muscular layer.
The surgical treatment was definitive in terms of curing the condition, but the patient still requires periodic follow-up.
This is an uncommon, difficult-to-diagnose disorder with few reported cases.2 It is thought to be caused by hypoperfusion of the mesenteric vessels. However, there are multiple factors which make it unusual: first of all, ischaemic changes are rare in the small intestine due to its rich blood supply from collateral arteries; secondly, there are no established clinical or pathological diagnostic criteria for ischaemic enteritis; and thirdly, the small intestine is not easy to assess because of its length. Ischaemic enteritis is classified according to its progression as transient, when it resolves completely within a few days without sequelae, and permanent or stricturing,1,2 when it presents with tubular stenosis after a period of chronic inflammation.1 The most characteristic macroscopic histopathological findings are the formation of strictures, segmental circumferential ulcers and proximal tubular stenosis.1,2 Strictures tend to progressively worsen and ultimately lead to total obstruction.1–3 Microscopically, ulcers of variable depth are identified, with their bases coated with granulation tissue, and severe fibrosis mainly in the submucosa. There is usually severe inflammatory infiltration (mainly lymphocytes and plasma cells) and haemosiderin-laden macrophages scattered throughout the entire breadth of the intestine.
Increasing use and understanding of imaging studies such as VCE and balloon enteroscopy could increase earlier and more accurate detection of the disorder.2,4,5 In this case, the diagnostic approach used was VCE, followed by curative surgical treatment.
Please cite this article as: Mosquera-Klinger G, Rincón RA. Ileítis isquémica idiopática, con sangrado digestivo oscuro manifiesto. Gastroenterol Hepatol. 2019;42:439–440.