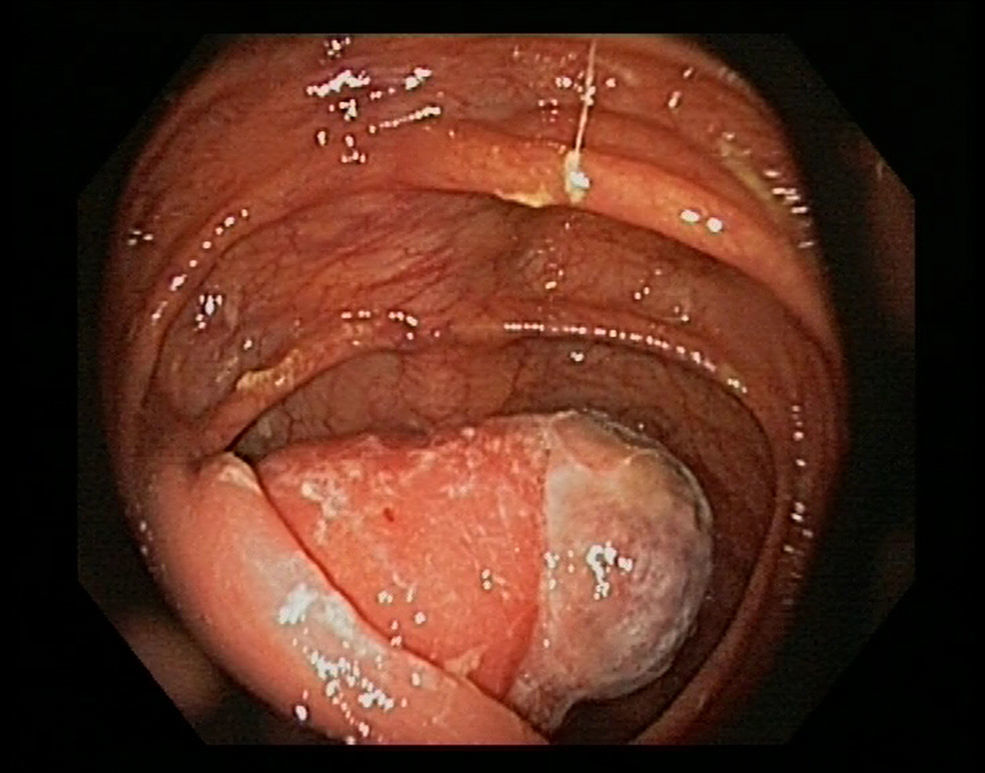
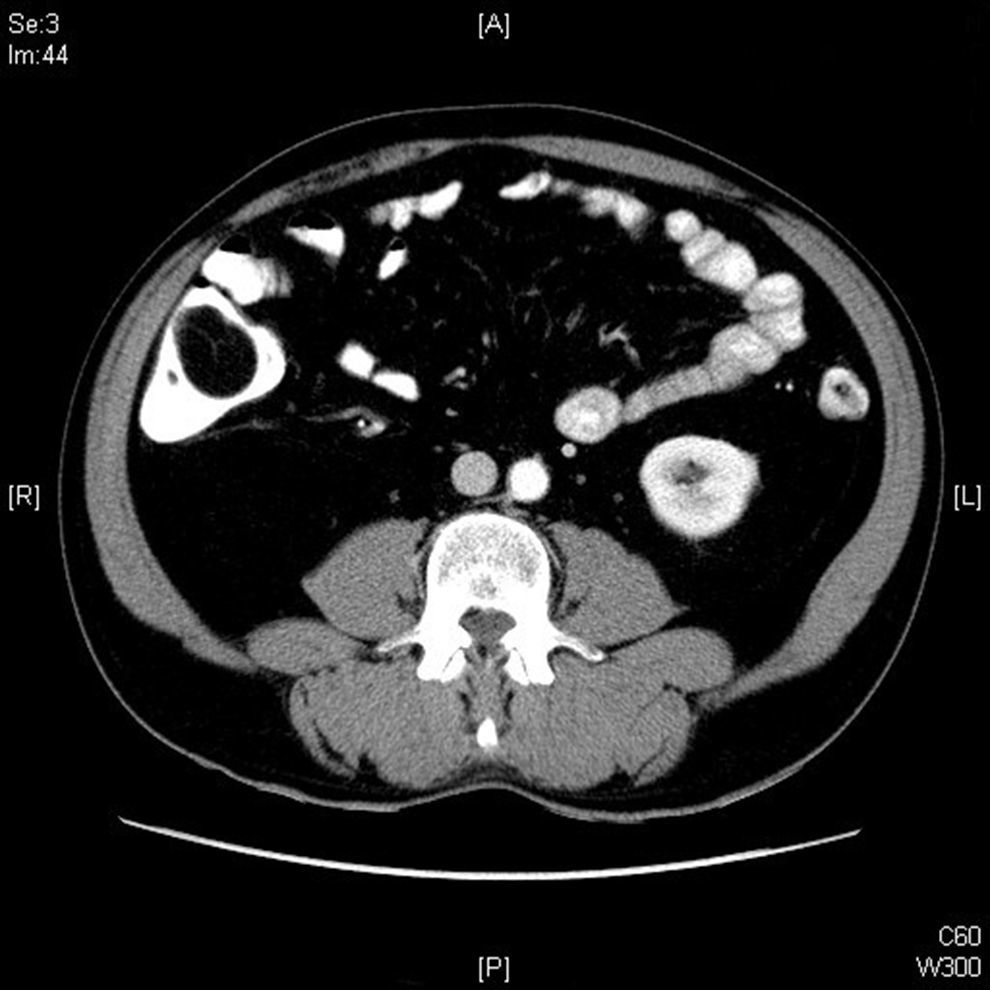
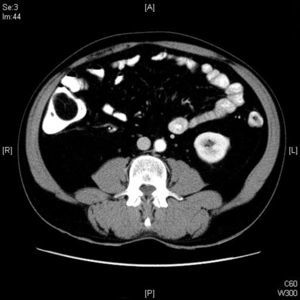
Here we report the case of a 54-year-old man, with no history of interest, who was admitted to hospital for lower gastrointestinal bleeding, manifested as rectal bleeding with dark blood, which did not affect his hemodynamic stability. In the days before admission, he had abdominal pain with cramps, nausea and vomiting. Because of the characteristics of the feces, a gastroscopy was performed, which showed no abnormalities. When performing a colonoscopy, traces of blood were found throughout the colon, as well as a bulging ileocecal valve. An ileoscopy was performed with some difficulty, without being able to see any damage; but when the endoscope was removed again, a whitish lesion was seen in the base of the caecum, which appeared to be ulcerated, but with no active bleeding, and was about 3cm and prolapsed through the ileocecal valve (Fig. 1). Biopsies were taken of the lesion, and it was compatible with a lipoma. The study was completed with a CT scan (Fig. 2), which showed a fat and pedunculated mass, originating on the inner lip of the ileocecal valve, that was prolapsed in the base of the caecum. The patient was assessed in the general surgery department, and it was decided to treat the lesion by using elective laparoscopic right hemicolectomy, which confirmed the origin of the lesion. The surgical specimen measured a total of 18×5cm, with a pedicled lesion originating in the terminal ileum and with a maximum size of 5×2.3cm, and was brown-colored with macroscopic involvement of the mucosa, compatible with lipoma.
Lipomas are benign, and usually submucosal, mesenchymal tumors. Gastrointestinal lipomas are located primarily in the right colon, and to a lesser extent, in the small intestine.1 They are usually asymptomatic, and when they do cause symptoms, they are non-specific ones, such as occlusive problems, bleeding, abdominal pain, nausea or diarrhea.
Types of intussusception were classified in 1956 as enteric, colocolic, ileocecal and ileocolic,2 with the most common being enteric intussusception, because it occurs in 43% of patients.3 Our case involves an ileocolic intussusception, with an ileal lipoma being the main cause. Generally, in submucosal lesions such as lipomas, conventional biopsies are not the best means for an accurate diagnosis. In our case this was not so, because the lipoma affected the mucosa macroscopically, which allowed us to collect adipose tissue with a conventional biopsy, thus facilitating the diagnosis.
Historically the treatment of symptomatic lipomas has been surgical, as in our case, by the use of a laparoscopic right hemicolectomy. In the past few years, cases of single-port laparoscopy have been reported, with fewer complications and a more acceptable esthetic result.4
Recently, endoscopic techniques have been developed to treat lipomas in certain cases, mostly in patients who are not candidates for surgery or who reject it.
Endoscopic submucosal dissection is a technique originally intended for superficial neoplastic lesions, but it has also been used to resect symptomatic lipomas.5 However, this is a complex technique that is not performed at all centers in our setting, and it has a higher rate of complications, mainly perforation and bleeding.
The loop-and-let-go technique consists of placing a disposable loop on the lipoma pedicle, which promotes a slow mechanical resection, thereby reducing the risk of bleeding and perforation.6
The unroofing technique consists of the spontaneous removal of the lipoma from the exposed mucosa after making an incision in the upper half of the mucosal surface of the submucosal mass.7
According to the literature, these techniques are mostly used for lipomas located in the colon, whereas in our case the lipoma was located in the terminal ileum, which made the endoscopic approach even more difficult. This being said, cases of ileal lipoma resections have been reported after bringing it into the colonic lumen by aspiration8 or by placing a cap at the tip of the endoscope.9
Despite advances in endoscopic techniques, surgical treatment is of vital importance for sessile lipomas with a wide base of implantation, for cases where diagnosis is uncertain, for lipomas that cause intussusception or obstruction, and for cases of involvement of the serous layers.10
Please cite this article as: Valdivielso Cortázar E, López Álvarez M, Guerrero Montañes A, Yañez González-Dopeso L, Yañez López JÁ, Alonso Aguirre PA. Intususcepción íleo-cólica de lipoma ileal como causa de hemorragia digestiva baja. Gastroenterol Hepatol. 2017;40:457–458.