Helicobacter pylori approximately infect 50% of Spanish population and causes chronic gastritis, peptic ulcer and gastric cancer. Until now, three consensus meetings on H. pylori infection had been performed in Spain (the last in 2012). The changes in the treatment schemes, and the increasing available evidence, have justified organising the IV Spanish Consensus Conference (March 2016), focused on the treatment of this infection. Nineteen experts participated, who performed a systematic review of the scientific evidence and developed a series of recommendation that were subjected to an anonymous Delphi process of iterative voting. Scientific evidence and the strength of the recommendation were classified using GRADE guidelines. As starting point, this consensus increased the minimum acceptable efficacy of recommended treatments that should reach, or preferably surpass, the 90% cure rate when prescribed empirically. Therefore, only quadruple therapies (with or without bismuth), and generally lasting 14 days, are recommended both for first and second line treatments. Non-bismuth quadruple concomitant regimen, including a proton pump inhibitor, clarithromycin, amoxicillin and metronidazole, is recommended as first line. In the present consensus, other first line alternatives and rescue treatments are also reviewed and recommended.
La infección por Helicobacter pylori afecta aproximadamente al 50% de la población española y es causante de la gastritis crónica, la úlcera péptica y el cáncer gástrico. Se han llevado a cabo hasta el momento, en nuestro país, 3 reuniones de Consenso sobre el manejo de la infección por H.pylori (la última de ellas en 2012). Los cambios en los esquemas de tratamiento y la creciente evidencia disponible al respecto han justificado la organización de esta IV Conferencia Española de Consenso en marzo de 2016, centrada en el tratamiento de esta infección. Participaron 19 expertos sobre el tema, que realizaron una búsqueda sistemática de la evidencia científica y elaboraron una serie de recomendaciones que fueron sometidas a un proceso de interacción de votaciones anónimas seriadas mediante metodología Delphi. Para clasificar la evidencia científica y la fuerza de las recomendaciones se utilizó el sistema GRADE. Este consenso establece, como punto de partida, un aumento de la exigencia en la eficacia de los tratamientos recomendados, que deben alcanzar, o preferiblemente superar, el 90% de curación al ser administrados de forma empírica. De este modo, tanto en primera como en segunda línea se recomiendan tratamientos cuádruples con o sin bismuto, generalmente prescritos durante 14días. El tratamiento cuádruple sin bismuto concomitante, que incluye un inhibidor de la bomba de protones, claritromicina, amoxicilina y metronidazol, se recomienda como primera línea. En el presente consenso se revisan también con detalle otras alternativas de tratamiento tanto de primera línea como de rescate.
Helicobacter pylori infection affects around 50% of the world population, and plays a key role in the development of various gastrointestinal diseases such as chronic gastritis, peptic ulcer and gastric cancer, so proper diagnosis and effective treatment are essential in clinical practice. Several Consensus Conferences have hitherto been organised on the diagnosis and treatment of infection by this microorganism in the United States, Europe and Asia. Three Consensus meetings on the diagnosis and treatment of H. pylori infection have been held thus far in Spain: in 1999,1,2 in 20043,4 and in 2012.5 The notable changes made in treatment regimens and growing evidence in support of these prompted the organisation of a fourth Spanish Consensus Conference, held in March 2016. Since there have been no relevant breakthroughs in aspects related with treatment indications or diagnostic techniques, this Consensus Conference focused exclusively on updating the recommendations for the treatment of H. pylori infection.
MethodologyConference participants. All the experts who participated in the last Consensus Conference held in 2012 were invited.3 Researchers named as first author on any article on treatment of H. pylori infection published in the last 4 years (identified using the search strategy “helicobacter pylori AND Spain” in PubMed) were also asked to attend. A total of 19 experts were invited, with 18 (95%) eventually participating, including gastroenterologists, microbiologists, primary care physicians and experts in scientific methodology and evidence-based medicine. Two gastroenterologists (JPG and JMI) acted as coordinators.
Literature searches. Systematic reviews and other critical synthesis documents in the scientific literature were first identified. The following electronic databases were consulted: TRIP Database, NHS National Library of Guidelines, National Guideline Clearinghouse, Cochrane Database of Systematic Reviews (The Cochrane Library), Database of Abstracts of Reviews of Effects (DARE) and MEDLINE (accessed by PubMed). The second phase consisted of a search for individual studies, randomised clinical trials and observational studies, as well as a review of the bibliographical references cited in the documents included.
Grading the quality of scientific evidence and the strength of recommendations. The Grading of Recommendations Assessment, Development and Evaluation (GRADE) system (http://www.gradeworkinggroup.org/) was used to grade the quality of the scientific evidence and the strength of the recommendations. GRADE, a clear structured classification system that is being widely adopted in the international setting, has the advantage of overcoming the limitations of previous systems and standardising the formulation of guidelines by all institutions.6,7
Evaluation of the recommendations by the consensus group. The recommendations were initially drawn up by the coordinators and then submitted to an interactive, anonymous serial voting system using the Delphi methodology.8 Three rounds of voting took place, 2 online and 1 in person. The online procedure was carried out using the REDCap (research electronic data capture) system, a software application hosted on the Spanish Association of Gastroenterology (AEG) server (https://redcap.aegastro.es/).9 AEG is a non-profit medical-scientific society dedicated to research and training in the field of gastroenterology, and offers this service free of charge with the sole aim of promoting research led by independent investigators. REDCap is a secure web-based application designed to support data capture for research studies, offering: (1) an intuitive interface for compiling validated data; (2) traceability of data manipulation, access and export; (3) automated procedures for seamless data downloads to common statistical programmes, and (4) procedures for importing data from external sources.
The participants rated their agreement with each recommendation on a 6-point Likert scale (1: completely disagree; 2: mostly disagree; 3: somewhat disagree; 4: somewhat agree; 5: mostly agree; 6: completely agree). Any score under 6 required the coordinators to review each section of that recommendation (wording, grade of evidence, strength of the recommendation and rationale), and to make suggestions for improvement. After each vote, the 2 coordinators gathered together the comments and votes received for each recommendation, integrating the suggestions to maximise the agreement.
The recommendations that emerged from the 2 rounds of online voting were discussed and approved during an in-person meeting held in Madrid on 1 March 2016, chaired by the 2 coordinators (JPG and JMI). During the meeting, the recommendations were reviewed, amended (when necessary) and submitted to a new vote. A recommendation was approved if more than 75% of the participants were in agreement (score of 4–6 on the Likert scale). AGM acted as scientific secretary of the consensus, taking the minutes of the meeting, counting the votes in the various rounds of voting, recording the comments, and systematizing the incorporation of suggestions.
Ethical aspects. The consensus complied with established ethical guidelines.10 The participants declared any conflicts of interest before and after the Delphi voting process.
Sponsorship, endorsements and funding. The conference was sponsored by the Spanish Biomedical Research Networking Centre for Liver and Digestive Diseases (CIBEREHD). This Consensus document has been endorsed by the Spanish Association of Gastroenterology and by the Spanish Society of Digestive Pathology, who have adhered to and supported the consensus recommendations. No funding was received from any pharmaceutical company.
RecommendationsEach recommendation is accompanied by the final vote (percentage of agreement), grade of recommendation (GR; strong or weak), certainty in the evidence (CE; high, moderate, low or very low) and discussion of the corresponding evidence.
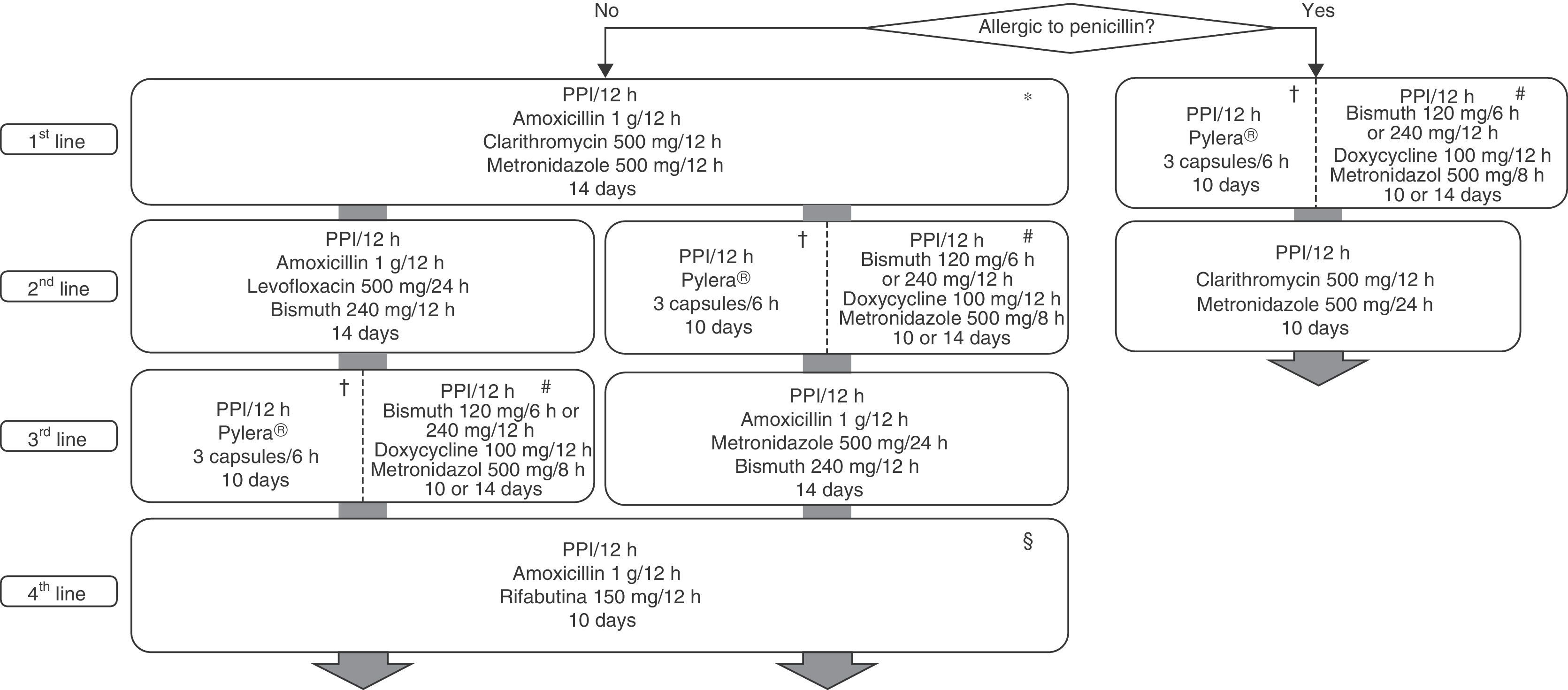
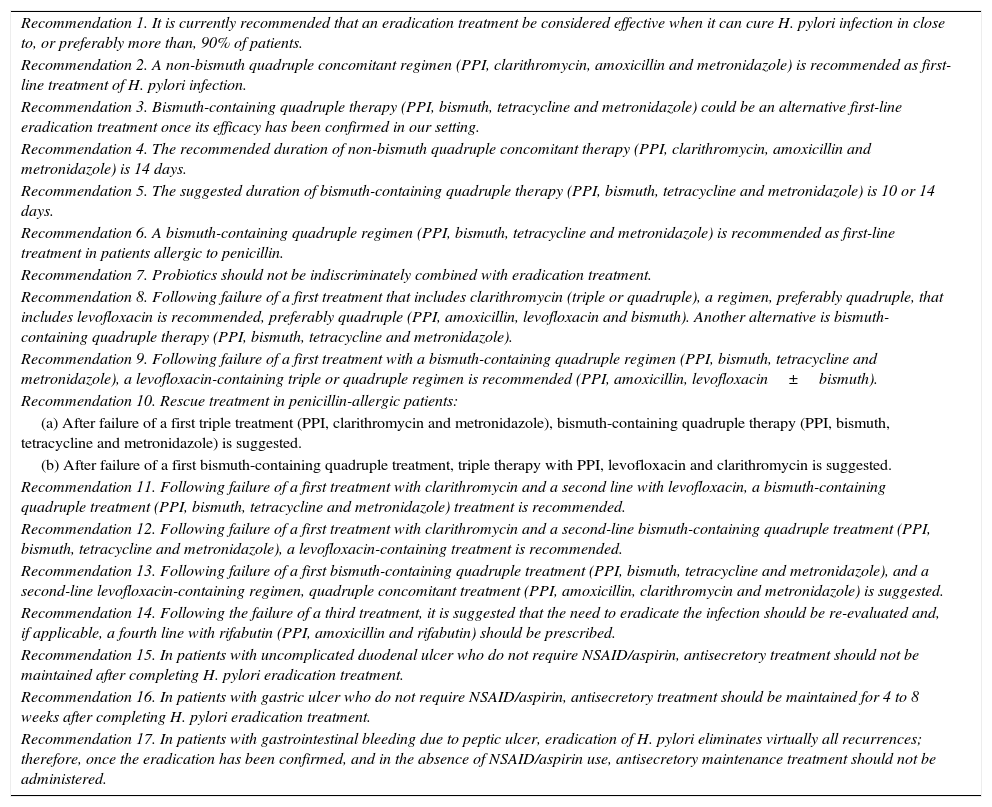
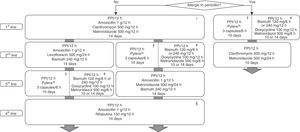
All the recommendations approved in the present Spanish Consensus on the treatment of H. pylori infection are included in Table 1. The drugs, duration and dose of each component included in the recommended regimens are broken down in Table 2. Finally, the algorithm for initial and rescue treatment of the infection is shown in Fig. 1.
Recommendations for the treatment of Helicobacter pylori infection.
| Recommendation 1. It is currently recommended that an eradication treatment be considered effective when it can cure H. pylori infection in close to, or preferably more than, 90% of patients. |
| Recommendation 2. A non-bismuth quadruple concomitant regimen (PPI, clarithromycin, amoxicillin and metronidazole) is recommended as first-line treatment of H. pylori infection. |
| Recommendation 3. Bismuth-containing quadruple therapy (PPI, bismuth, tetracycline and metronidazole) could be an alternative first-line eradication treatment once its efficacy has been confirmed in our setting. |
| Recommendation 4. The recommended duration of non-bismuth quadruple concomitant therapy (PPI, clarithromycin, amoxicillin and metronidazole) is 14 days. |
| Recommendation 5. The suggested duration of bismuth-containing quadruple therapy (PPI, bismuth, tetracycline and metronidazole) is 10 or 14 days. |
| Recommendation 6. A bismuth-containing quadruple regimen (PPI, bismuth, tetracycline and metronidazole) is recommended as first-line treatment in patients allergic to penicillin. |
| Recommendation 7. Probiotics should not be indiscriminately combined with eradication treatment. |
| Recommendation 8. Following failure of a first treatment that includes clarithromycin (triple or quadruple), a regimen, preferably quadruple, that includes levofloxacin is recommended, preferably quadruple (PPI, amoxicillin, levofloxacin and bismuth). Another alternative is bismuth-containing quadruple therapy (PPI, bismuth, tetracycline and metronidazole). |
| Recommendation 9. Following failure of a first treatment with a bismuth-containing quadruple regimen (PPI, bismuth, tetracycline and metronidazole), a levofloxacin-containing triple or quadruple regimen is recommended (PPI, amoxicillin, levofloxacin±bismuth). |
| Recommendation 10. Rescue treatment in penicillin-allergic patients: |
| (a) After failure of a first triple treatment (PPI, clarithromycin and metronidazole), bismuth-containing quadruple therapy (PPI, bismuth, tetracycline and metronidazole) is suggested. |
| (b) After failure of a first bismuth-containing quadruple treatment, triple therapy with PPI, levofloxacin and clarithromycin is suggested. |
| Recommendation 11. Following failure of a first treatment with clarithromycin and a second line with levofloxacin, a bismuth-containing quadruple treatment (PPI, bismuth, tetracycline and metronidazole) treatment is recommended. |
| Recommendation 12. Following failure of a first treatment with clarithromycin and a second-line bismuth-containing quadruple treatment (PPI, bismuth, tetracycline and metronidazole), a levofloxacin-containing treatment is recommended. |
| Recommendation 13. Following failure of a first bismuth-containing quadruple treatment (PPI, bismuth, tetracycline and metronidazole), and a second-line levofloxacin-containing regimen, quadruple concomitant treatment (PPI, amoxicillin, clarithromycin and metronidazole) is suggested. |
| Recommendation 14. Following the failure of a third treatment, it is suggested that the need to eradicate the infection should be re-evaluated and, if applicable, a fourth line with rifabutin (PPI, amoxicillin and rifabutin) should be prescribed. |
| Recommendation 15. In patients with uncomplicated duodenal ulcer who do not require NSAID/aspirin, antisecretory treatment should not be maintained after completing H. pylori eradication treatment. |
| Recommendation 16. In patients with gastric ulcer who do not require NSAID/aspirin, antisecretory treatment should be maintained for 4 to 8 weeks after completing H. pylori eradication treatment. |
| Recommendation 17. In patients with gastrointestinal bleeding due to peptic ulcer, eradication of H. pylori eliminates virtually all recurrences; therefore, once the eradication has been confirmed, and in the absence of NSAID/aspirin use, antisecretory maintenance treatment should not be administered. |
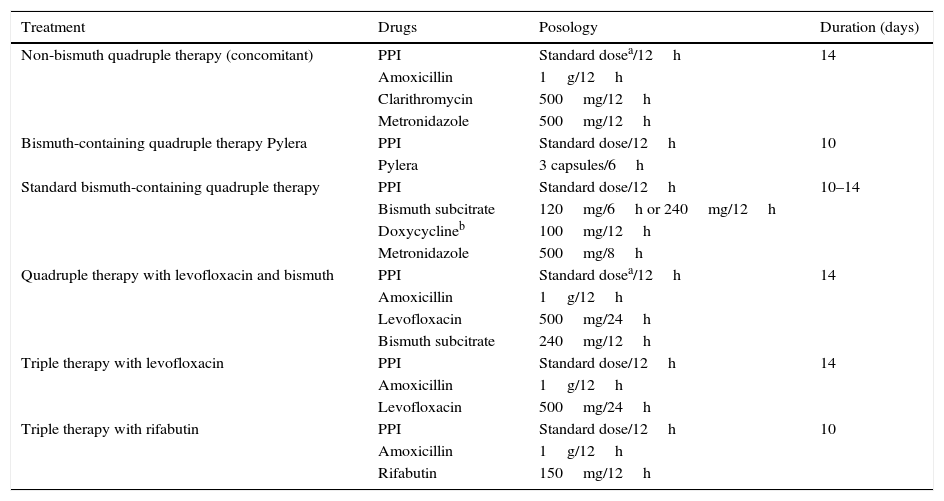
Drugs, doses and duration of eradication treatments for Helicobacter pylori infection.
| Treatment | Drugs | Posology | Duration (days) |
|---|---|---|---|
| Non-bismuth quadruple therapy (concomitant) | PPI | Standard dosea/12h | 14 |
| Amoxicillin | 1g/12h | ||
| Clarithromycin | 500mg/12h | ||
| Metronidazole | 500mg/12h | ||
| Bismuth-containing quadruple therapy Pylera | PPI | Standard dose/12h | 10 |
| Pylera | 3 capsules/6h | ||
| Standard bismuth-containing quadruple therapy | PPI | Standard dose/12h | 10–14 |
| Bismuth subcitrate | 120mg/6h or 240mg/12h | ||
| Doxycyclineb | 100mg/12h | ||
| Metronidazole | 500mg/8h | ||
| Quadruple therapy with levofloxacin and bismuth | PPI | Standard dosea/12h | 14 |
| Amoxicillin | 1g/12h | ||
| Levofloxacin | 500mg/24h | ||
| Bismuth subcitrate | 240mg/12h | ||
| Triple therapy with levofloxacin | PPI | Standard dose/12h | 14 |
| Amoxicillin | 1g/12h | ||
| Levofloxacin | 500mg/24h | ||
| Triple therapy with rifabutin | PPI | Standard dose/12h | 10 |
| Amoxicillin | 1g/12h | ||
| Rifabutin | 150mg/12h |
PPI: proton pump inhibitor.
Algorithm for initial and rescue treatment of Helicobacter pylori infection. H: hours; PPI: proton pump inhibitor. *Bismuth-containing quadruple therapy (PPI, bismuth, tetracycline and metronidazole) could be an alternative as first-line eradication treatment, once its efficacy has been confirmed in our setting. †There is a new formulation with all the antibiotics included in a single capsule. #Tetracycline hydrochloride on its own is not marketed in Spain; doxycycline can be used instead (100mg/12h), although experience is much more limited and there are doubts about its therapeutic equivalence. §It is suggested to carefully re-evaluate the need to eradicate the infection.
Since the advantage of guiding eradication therapy by studying the antimicrobial susceptibility of the H. pylori strain versus empirical administration of treatment has not been sufficiently confirmed,11,12 and since this test is not generally accessible,13 the comments included in this consensus document will be based on the assumption that this susceptibility is unknown.
• Recommendation 1. It is currently recommended that an eradication treatment be considered effective when it can cure H. pylori infection in close to, or preferably more than, 90% of patients.
Agreement: 92.3%; votes: completely agree (84.6%); mostly agree (7.7%); completely disagree (7.7%). GR: strong. CE: very low.
The goal of therapy aimed at eliminating any microorganism should be to reach a 100% success rate, and H. pylori infection should be no exception.14 However, all previous European15–18 and Spanish2,4,5 consensus documents have established that a cure rate greater than or equal to 80% could be considered sufficient. Given that quadruple therapies with cure rates close to or even higher than 90% are currently available,19,20 it was considered that this efficacy threshold should henceforth be required to consider treatment for H. pylori infection effective. To achieve this goal, all treatments should be optimised in terms of duration, dose and frequency of proton pump inhibitor (PPI) and antibiotic administration.21
• Recommendation 2. A non-bismuth quadruple concomitant regimen (PPI, clarithromycin, amoxicillin and metronidazole) is recommended as first-line treatment of H. pylori infection.
Agreement: 100%; votes: completely agree: (100%). GR: strong. CE: moderate.
The choice of first-line treatment for H. pylori infection will depend primarily on the rate of resistance of this bacterium to the antibiotics prescribed. Standard triple therapy (PPI, clarithromycin and amoxicillin) is not recommended when the rate of resistance to clarithromycin is >15%,18 since the eradication rates are unacceptably low above this threshold.21 Other factors that affect the efficacy of eradication treatment are patient compliance and their previous history of antibiotic use, which could determine the choice of first treatment option.21 The evidence available with respect to the different first-line treatment regimens is reviewed below.
Triple therapy (PPI, clarithromycin and amoxicillin)The mean efficacy of triple therapy in Spain was 80% and 70% in 2 systematic reviews published in 2011 and 2013, respectively.22,23 The efficacy of triple therapy in subsequent Spanish studies has always been less than 75%.24,25 A recent multicentre study using triple therapy for 14 days with high-dose PPIs managed to increase efficacy to 81%.26 In Spain, the mean rate of resistance to clarithromycin was 14% in 200927 and 18% in an updated review in 2013.23 A recent study has shown the rate of resistance to clarithromycin in children to be 34%,28 while in a multicentre study conducted in the Andalusia region of Spain, published in 2015, the mean rate of resistance was 18%.29 Together, all this evidence points to the need to abandon triple therapy as first-line treatment in Spain, especially when therapeutic alternatives with significantly better cure rates are now available; these include non-bismuth quadruple therapies (in sequential, concomitant or hybrid regimens), which will be reviewed below.
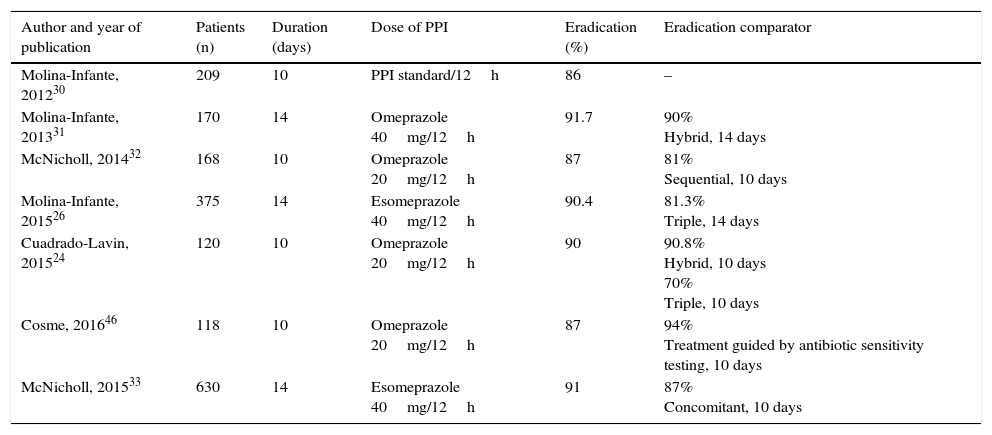
Non-bismuth quadruple therapies (PPI, amoxicillin, clarithromycin and metronidazole)The efficacy of non-bismuth quadruple therapies will depend on the prevalence of H. pylori strains that are simultaneously resistant to clarithromycin and to metronidazole (dual or double resistance).21 Concomitant treatment is the most effective quadruple therapy in situations of high resistance. Sequential, hybrid and concomitant treatments are estimated to achieve cure rates >90% when this double resistance rate is below 5%, 9% and 15%, respectively. In Spain, the dual resistance rate is still below 15%. Several studies conducted in Europe (Spain,24,26,30–33 Greece34–36 and Italy37,38) and Asia (Taiwan39,40 and Japan41) have shown an efficacy close to or greater than 90% in intention-to-treat analysis. Nevertheless, in certain regions of Europe and Asia, with much higher rates of resistance to clarithromycin and metronidazole, the efficacy of concomitant treatment has been suboptimal (Turkey,42 South Korea43,44 and China45). The outcomes obtained with this quadruple treatment in various studies conducted in Spain since 2012 are summarised in Table 3, showing a mean eradication efficacy of approximately 90%.24,26,30–33,46 Quadruple concomitant treatment is therefore considered a valid first-choice alternative.
Spanish studies that have evaluated the efficacy (intention-to-treat) of first-line non-bismuth quadruple concomitant therapy in the last 5 years.
| Author and year of publication | Patients (n) | Duration (days) | Dose of PPI | Eradication (%) | Eradication comparator |
|---|---|---|---|---|---|
| Molina-Infante, 201230 | 209 | 10 | PPI standard/12h | 86 | – |
| Molina-Infante, 201331 | 170 | 14 | Omeprazole 40mg/12h | 91.7 | 90% Hybrid, 14 days |
| McNicholl, 201432 | 168 | 10 | Omeprazole 20mg/12h | 87 | 81% Sequential, 10 days |
| Molina-Infante, 201526 | 375 | 14 | Esomeprazole 40mg/12h | 90.4 | 81.3% Triple, 14 days |
| Cuadrado-Lavin, 201524 | 120 | 10 | Omeprazole 20mg/12h | 90 | 90.8% Hybrid, 10 days 70% Triple, 10 days |
| Cosme, 201646 | 118 | 10 | Omeprazole 20mg/12h | 87 | 94% Treatment guided by antibiotic sensitivity testing, 10 days |
| McNicholl, 201533 | 630 | 14 | Esomeprazole 40mg/12h | 91 | 87% Concomitant, 10 days |
PPI: proton pump inhibitor.
Several recent studies and meta-analyses have shown that sequential therapy (PPI together with amoxicillin for the first 5 days, followed by PPI together with clarithromycin and metronidazole for the last 5 days) is not superior to 14-day triple therapy.47–50 Furthermore, concomitant treatment is significantly superior to sequential treatment when both are prescribed for a similar length of time.51 In addition, suboptimal results with this regimen have recently been published in our setting.32,52,53 Therefore, the use of sequential therapy is not currently recommended.
Hybrid treatment (PPI together with amoxicillin for the first 5–7 days, followed by PPI together with amoxicillin, clarithromycin and metronidazole for the last 5–7 days) is a therapeutic alternative that reduces the antibiotic load during the first half of treatment, and could theoretically improve tolerance and treatment compliance. This treatment showed an initial efficacy of 97% in a multicentre study conducted in Taiwan,54 later confirmed in 2 subsequent Taiwanese studies, even with a duration less than 14 days.55,56 Nevertheless, it is important to highlight that the clarithromycin resistance rate in Taiwan is low (8%).57 The efficacy of hybrid treatment was corroborated in later studies in Iran58,59 and Spain.24,31 The eradication rate in both Spanish studies was 90%, with durations of 1024 and 14 days.31 In contrast, recent studies published in Italy37,38 and Korea44,60 have shown hybrid treatment to be less effective (77–85%). Either way, a more robust comparative validation of this hybrid therapy is required before it can be incorporated into our therapeutic armamentarium.
In summary, a non-bismuth quadruple concomitant regimen is recommended as first-line treatment of H. pylori infection in Spain. The duration of therapy and dose of each component (i.e. PPI, clarithromycin, amoxicillin and metronidazole) are summarised in Table 2. For further details on the duration of treatment, see recommendation 4.
• Recommendation 3. Bismuth-containing quadruple therapy (PPI, bismuth, tetracycline and metronidazole) could be an alternative first-line eradication treatment once its efficacy has been confirmed in our setting.
Agreement: 100%; votes: completely agree (92.3%); mostly agree (7.7%). GR: weak. CE: low.
Bismuth-containing quadruple therapy (PPI, bismuth, tetracycline and metronidazole) could be a valid alternative to non-bismuth quadruple treatment, since it consists of drugs such as bismuth and tetracycline, to which H. pylori is never or only exceptionally resistant.61 In addition, resistance to metronidazole may be partially overcome by increasing the dose, frequency and duration of treatment with this antibiotic.61 In countries such as China, with rates of resistance to clarithromycin of between 20% and 40%, and resistance to metronidazole greater than 60%, where no triple or non-bismuth quadruple treatment will reach acceptable efficacy rates, bismuth-containing quadruple therapies are currently the preferred first-line treatment.62 However, experience in Spain has been limited by the frequent lack of availability of tetracycline.
Three meta-analyses carried out in last decade have been unanimous in stressing that bismuth-containing quadruple therapy (mean efficacy of 81%, 78% and 77%) has no advantage over triple treatment.63–65 However, bismuth-containing quadruple therapy was prescribed for only 7 days in the studies on which these meta-analyses were based, and moreover, they were published over a decade ago or more, when clarithromycin resistance rates (which penalise the efficacy of triple therapy) were considerably lower. A recent European multicentre study showed good outcomes with Pylera (a capsule containing bismuth, tetracycline and metronidazole) administered for 10 days, reaching a modified intention-to-treat efficacy (confirmed by a single breath test) of 90% (significantly higher than that of triple therapy).66 Nevertheless, there are some limitations and uncertainties surrounding this new pharmaceutical formulation (Pylera), such as: (1) it is available in a single 10-day format, when a 14-day course might increase its efficacy against metronidazole-resistant H. pylori67; (2) it includes relatively low doses of tetracycline (2g/day in the standard regimen versus 1.5g/day in Pylera); (3) so far, there is very little experience–and therefore scientific evidence–for this new therapeutic formulation in the treatment of infection in Spain, and (4) although Pylera will very likely improve treatment compliance, it is not known whether it will affect the onset of adverse effects.68 Furthermore, there are no comparative studies between bismuth-containing and non-bismuth (concomitant) quadruple therapies. The recent release of Pylera on the Spanish market (2016) should enable all these questions to be answered.
Finally, a new therapeutic approach is bismuth-containing quadruple treatment together with amoxicillin and metronidazole. These combinations have the advantage of using cheap and easily accessible antibiotics, dispensing with tetracycline. The high efficacy of this new first-line treatment regimen (close to or greater than 90%) has been demonstrated in 2 recent studies conducted in China and Thailand,68,69 both of which have a high rate of resistance to clarithromycin (45% and 50%, respectively). It should be noted that the efficacy of this bismuth-containing quadruple therapy against metronidazole-resistant strains was significantly reduced when used for less than 7 days (72%)69 compared to 14 days (>90%).68 Nevertheless, this promising therapeutic regimen must be validated in Spain before it can be recommended.
In summary, bismuth-containing quadruple therapy (PPI, bismuth, tetracycline and metronidazole) could be an alternative first-line eradication treatment in Spain, once its efficacy has been confirmed in our setting. The duration and dose of its components are summarised in Table 2. For further details on the duration of treatment, see recommendation 5.
• Recommendation 4. The recommended duration of non-bismuth quadruple concomitant therapy (PPI, clarithromycin, amoxicillin and metronidazole) is 14 days.
Agreement: 100%; votes: completely agree (85.7%); mostly agree (14.3%). GR: strong. CE: low.
Non-bismuth quadruple concomitant therapy, developed at the end of the 1990s, was initially designed to reduce the duration of eradication treatment.70 In fact, initial studies from Germany and Japan suggested that a duration of 3–5 days could be sufficient to reach acceptable cure rates.71,72 More recently, however, various clinical trials comparing different durations of this therapy have shown superior cure rates with longer treatments: 3 days (81%) vs 5 days (89%)73; 5 days (87%) vs 7 days (90%)74; 5 days (89%) vs 10 days (96%)75; or 5 days (78%) vs 14 days (86%).38 In a recent non-randomised Spanish study, concomitant treatment administered for 14 days (with high-dose PPI) was superior to another administered for 10 days (with standard-dose PPI; 87% vs 91%, p<0.01).33 In line with this, the first meta-analysis of this therapy revealed that the efficacy of concomitant treatment was dependent on the duration, so that the longer the course of treatment, the better the efficacy.76 Finally, this same tendency can be observed in the overall experience in Spain in the last 4 years, where only 14-day treatments consistently exceeded the efficacy threshold of 90% (Table 3).
In summary, and as a general rule, it is currently recommended that the duration of quadruple concomitant treatment should be 14 days. Concomitant treatment will obtain cure rates greater than 90% in regions with dual resistance (clarithromycin and amoxicillin) rates <15%, as is the case of Spain at present, provided that it is optimised in terms of extended duration (14 days) (and possibly high-dose PPI).77
• Recommendation 5. The suggested duration of bismuth-containing quadruple therapy (PPI, bismuth, tetracycline and metronidazole) is 10 or 14 days.
Agreement: 100%; votes: completely agree (100%). GR: weak. CE: low.
In a meta-analysis published in 2004 on different eradication treatments, the efficacy of bismuth-containing quadruple therapy administered for 1–3, 4 and 7 days was observed to be lower compared with a duration of 10–14 days.78 Similarly, a duration of 10 days or more was found to achieve cure rates greater than 85%, even in regions with a high prevalence of metronidazole resistance.78 However, a recent systematic review by the Cochrane Collaboration, which included 6 studies (1157 patients) with different bismuth quadruple combinations, was unable to show a significant advantage for any treatment duration (7, 10 and 14 days).79
To date, only one study (417 patients) has directly compared 10- and 14-day bismuth-containing quadruple therapy, finding no differences between regimens (91.6% vs 92.6%).80 In 2 large randomised clinical trials that included a 10-day course of Pylera (the capsule containing bismuth, tetracycline and metronidazole), the intention-to-treat efficacy was 87.7%81 and 80%,66 being effective against metronidazole-resistant strains in 80% and 91% of cases, respectively. In a small pilot study that evaluated the efficacy of this same pharmaceutical formulation for 14 days, the intention-to-treat efficacy was 85.1%, although 100% of the metronidazole-resistant strains were eradicated.67 In all these studies, the per-protocol efficacy was higher (91%,81 93%66 and 97%67) than the intention-to-treat efficacy, which suggests that poor compliance as a result of the relatively high rate of adverse effects associated with this therapy (58%,81 47%66 and 74%67) is key to explaining these results, independent of the treatment duration.
A 10-day bismuth-containing quadruple treatment will be highly effective against strains sensitive to metronidazole, but it is likely that a 14-day treatment will be more effective than a 10-day course against strains resistant to this antibiotic.68 In this respect, 2 recent studies that evaluated new quadruple treatments with bismuth combined with PPI, amoxicillin and metronidazole have shown cure rates >90% in China and Thailand, where resistance to metronidazole is 45% and 50%, respectively69,82; however, the efficacy of this new treatment against metronidazole-resistant strains was significantly reduced in shorter treatments: 7 days (72%)82 vs 14 days (>90%).69 This should be taken into account in Spain, where the mean rate of resistance to metronidazole is currently 41% (30–47%).23 Experience in our setting with first-line bismuth-containing quadruple therapy has been limited by the frequent shortage of tetracyclines. The recent release of Pylera in Spain will allow us to determine whether this treatment is sufficiently effective when used for 10 days (the only format currently available), or if it will need to be prolonged. Comparative studies evaluating the efficacy, safety and cost of different regimens are needed to clarify the ideal duration of bismuth-containing quadruple therapy. Meanwhile, it seems prudent to suggest that the duration of this therapy should be at least 10 days.
• Recommendation 6. A bismuth-containing quadruple regimen (PPI, bismuth, tetracycline and metronidazole) is recommended as first-line treatment in patients allergic to penicillin.
Agreement: 100%; votes: completely agree (100%). GR: strong. CE: low.
Amoxicillin is one of the most effective antimicrobial agents against H. pylori and, therefore, most eradication treatments include this antibiotic. Experience with eradication treatment in patients allergic to penicillin has been very scant to date, although this allergy is relatively common in clinical practice.
Triple therapy with PPI, clarithromycin and metronidazole is generally recommended in patients allergic to beta-lactamics.18 In a meta-analysis performed 15 years ago, treatment with PPI, clarithromycin and nitroimidazole was considered relatively effective for the treatment of H. pylori infection, with mean eradication rates above 80%.83 In an initial Spanish prospective study, this regimen was administered for 7 days to 12 patients who were allergic to penicillin, but obtained an eradication rate (intention-to-treat analysis) of only 58%.54 In another subsequent Spanish study–in this case multicentre–eradication rates as low as 55% were obtained when the same treatment was used in 50 patients.85 The disappointing cure rates (<60%) in the aforementioned recent Spanish studies84,85 could be due, at least in part, to the increase in rates of resistance to both clarithromycin and to metronidazole.23,27,86
In contrast, 2 groups of investigators evaluated the efficacy of a 10-day regimen with PPI, tetracycline and metronidazole in 5 and 17 patients allergic to penicillin, obtaining intention-to-treat eradication rates of 80–85%.87,88 These encouraging results suggest that this triple combination (or better still, with the addition of bismuth, which would result in a quadruple regimen) could be a better alternative first-line treatment in patients allergic to penicillin (mainly in areas with high resistance to metronidazole or clarithromycin). This is probably because the negative effect of the metronidazole resistance is overcome by the co-administration of bismuth,89 and because the efficacy of this regimen is not affected by resistance to clarithromycin.66
In this respect, the findings of a Spanish prospective multicentre study were recently updated. In this case, 267 patients allergic to penicillin were given first-line treatment with omeprazole, clarithromycin and metronidazole for 7 days, or omeprazole, bismuth, tetracycline and metronidazole for 10 days.90 The intention-to-treat eradication rate with the triple therapy was only 57%, while that of the quadruple regimen was clearly higher (74%). Treatment compliance was 94% and 98%, respectively. Fourteen percent of patients reported adverse effects with both regimens (all mild). The authors therefore concluded that, although a triple combination with PPI, clarithromycin and metronidazole can be prescribed to patients allergic to penicillin in areas with low clarithromycin resistance, standard bismuth-containing quadruple therapy should be preferred in countries such as Spain, where resistance to clarithromycin is common.
Finally, Liang et al.91 randomised 109 penicillin-allergic patients to receive standard bismuth-containing quadruple therapy (PPI, bismuth, tetracycline and metronidazole) for 2 weeks, or a modified bismuth-containing quadruple regimen (PPI, bismuth, tetracycline and furazolidone). The intention-to-treat eradication rates were, respectively, 88% and 92%, supporting the effectiveness of the bismuth-containing regimens in patients allergic to penicillin.
In summary, bismuth-containing quadruple therapy (PPI, bismuth, tetracycline and metronidazole) is recommended in Spain as first-line treatment in patients allergic to penicillin.
• Recommendation 7. Probiotics should not be indiscriminately combined with eradication treatment.
Agreement: 100%; votes: completely agree (85.7%); mostly agree (7.1%); somewhat agree (7.1%). GR: strong. CE: low.
Probiotics are live microorganisms that, when administered in adequate amounts, may be beneficial to health; they are currently indicated in the treatment of acute gastroenteritis and antibiotic-induced diarrhoea.92 The microorganisms most commonly used in probiotic formulations in clinical practice are Lactobacillus spp., Bifidobacterium and Saccharomyces, as well as Bacillus, Streptococcus and Escherichia coli. Their potential beneficial effects include regulation of the intestinal microbiota, stimulation of the immune system response and potential inhibitory activity against H. pylori demonstrated in vivo and in vitro.93
There is strong scientific evidence synthesised in numerous meta-analyses on the use of numerous different probiotic formulations (Lactobacillus combined with Bifidobacterium, bovine lactoferrin, lactic ferment, Saccharomyces boulardii and other probiotic formulations) that overall suggest a reduction in adverse effects and, to a lesser degree, an improvement the cure rate of eradication treatments.94–104 However, negative findings associated with probiotics combined with triple therapy have been reported.105–107 These discordant results are likely related with the use of different strains and combinations of strains, as well as different concentrations, doses and duration of treatment.77,108 Moreover, the immense majority of studies on probiotics have evaluated their impact on standard triple therapy, a well-tolerated treatment that is not recommended as first-line treatment due to insufficient efficacy. A recent meta-analysis that included 33 clinical trials and 4459 patients showed that the therapeutic gain obtained with probiotics was greater the less effective the eradication treatment.102 In fact, probiotic supplementation provided no therapeutic benefit when the effectiveness of eradication treatment was greater than 80%. No studies have yet been published evaluating the usefulness of probiotics combined with quadruple concomitant therapy, which is currently the recommended first-line treatment in Spain.
It should also be noted that probiotics are not subsidised in Spain, which increases the costs of eradication treatment; furthermore, the addition of a fifth drug adds to the complexity of quadruple treatment. Finally, no studies have as yet identified predictive risk factors for side effects with antibiotic therapy, and therefore administration of probiotics cannot be individualised. Probiotics can be considered in very specific cases, such as in patients with poor tolerance to or side effects with previous antibiotic treatments.
In conclusion, more evidence on the impact of probiotics on the effectiveness and safety of the new quadruple H. pylori eradication treatments is needed before they can be implemented in routine clinical practice. For now, therefore, probiotics should not be indiscriminately combined with eradication treatment.
• Recommendation 8. Following failure of a first treatment that includes clarithromycin (triple or quadruple) a regimen, preferably quadruple, that includes levofloxacin is recommended (PPI, amoxicillin, levofloxacin and bismuth). Another alternative is bismuth-containing quadruple therapy (PPI, bismuth, tetracycline and metronidazole).
Agreement: 100%; votes: completely agree (76.9%); mostly agree (15.4%); somewhat agree (7.7%). GR: strong. CE: moderate (after failure of triple therapy); low (after failure of quadruple therapy).
After failure of triple therapyAfter failure of triple therapy with PPI, clarithromycin and amoxicillin, it is reasonable to assume that H. pylori was already resistant to clarithromycin (primary resistance) or that it has developed resistance (secondary) to this antibiotic after failed eradication treatment; therefore, re-use of this antibiotic should be avoided. In this respect, a combined analysis of 8 studies found a very low eradication rate (46%) when clarithromycin-containing therapy was repeated.109
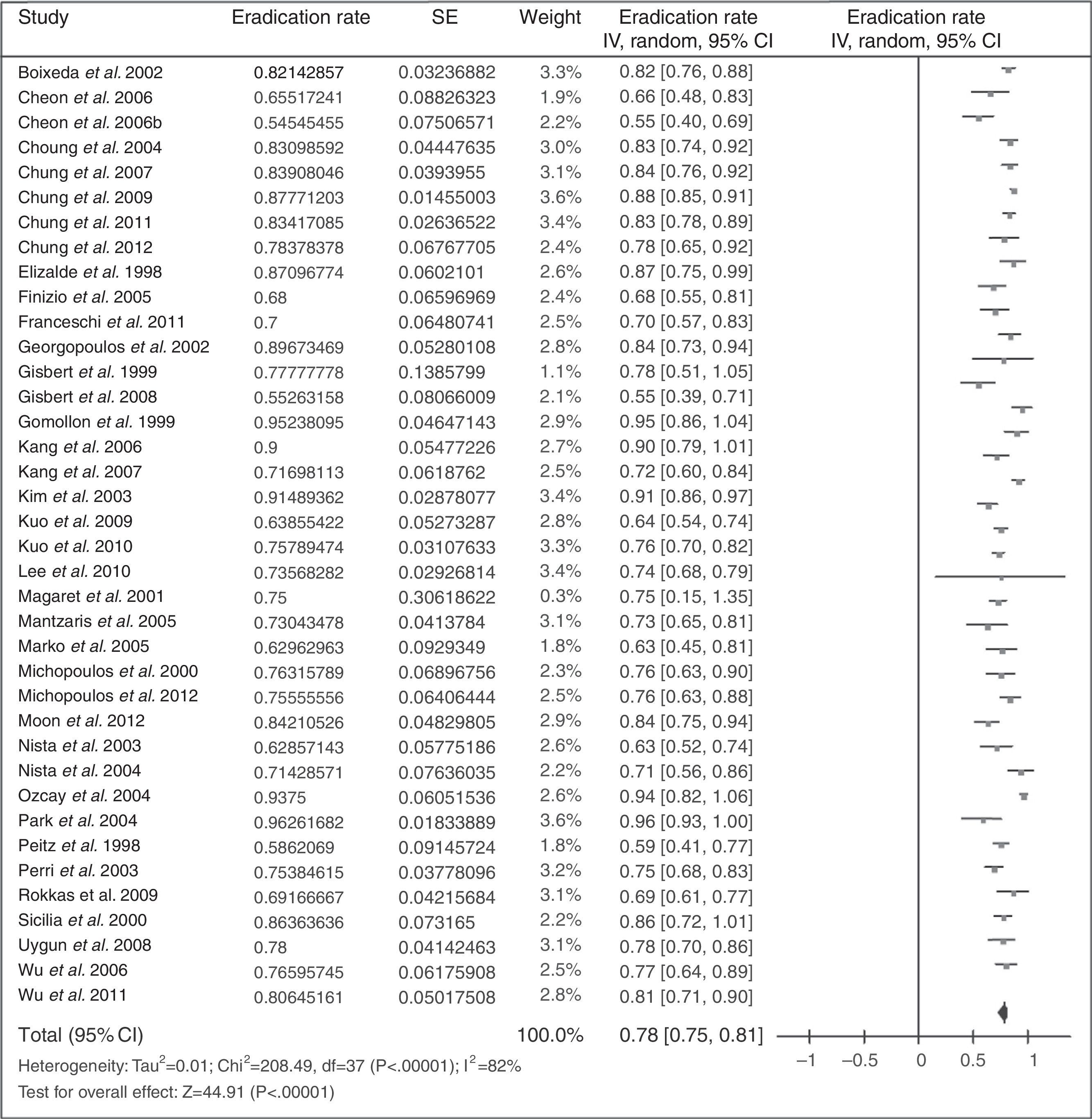
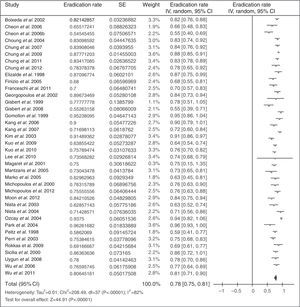
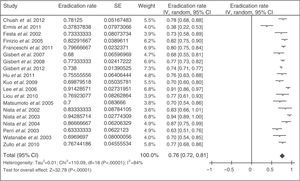
When standard triple treatment (PPI, clarithromycin and amoxicillin; combination currently not recommended) has failed, standard quadruple therapy (PPI, bismuth, tetracycline and metronidazole) has traditionally been recommended. The results obtained with this strategy are summarised in Fig. 2 (mean eradication rate of 78%).109
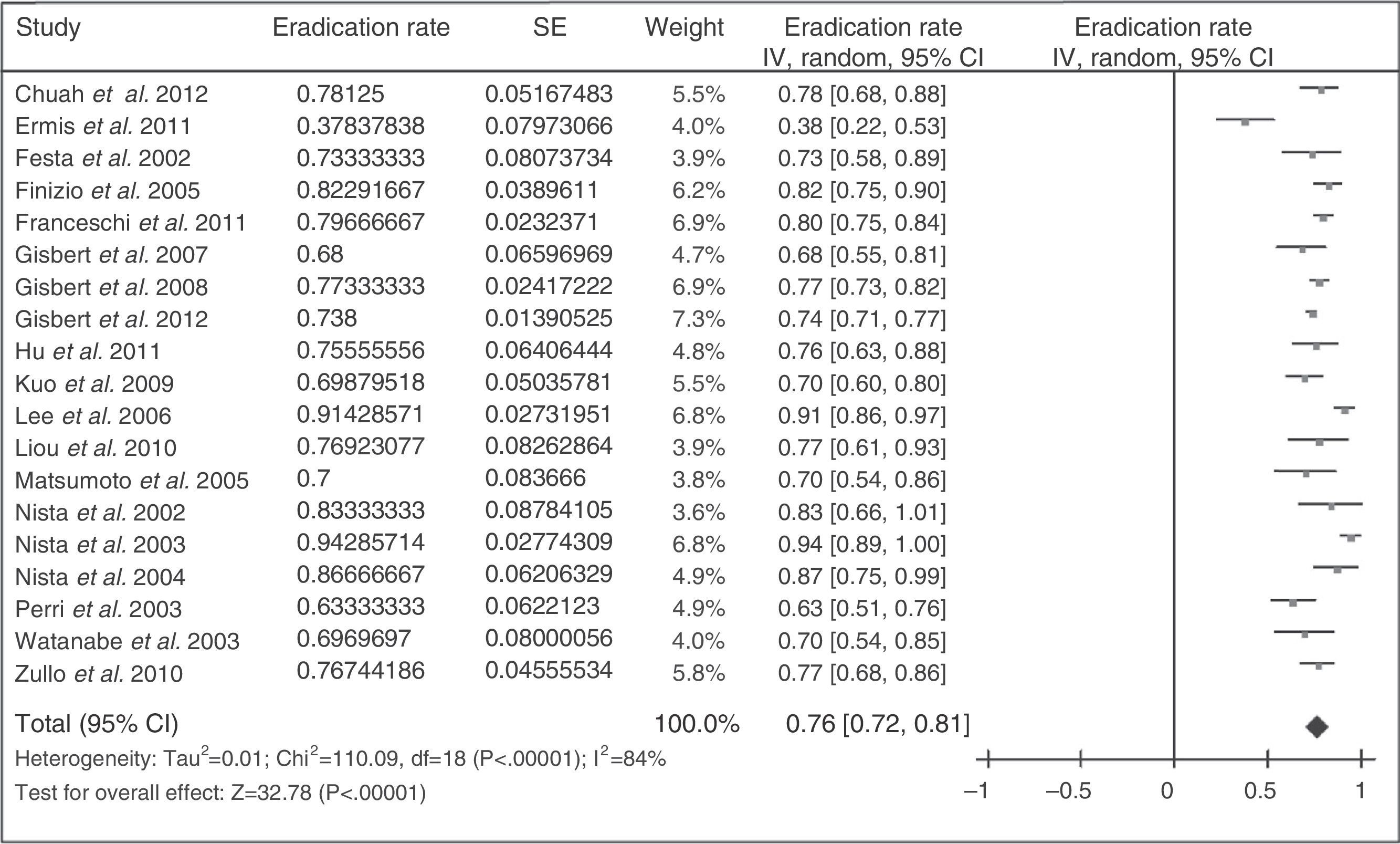
Given the complexity of bismuth-containing quadruple therapy and the shortage of tetracycline and bismuth salts in many countries, several studies have recently been conducted using levofloxacin as rescue treatment. The results have been encouraging, as summarised in Fig. 3 (mean eradication rate of 76%). Three meta-analyses have compared a levofloxacin-containing triple regimen against a bismuth-containing quadruple therapy as second-line treatment, and have shown better efficacy and a lower rate of adverse effects with the levofloxacin-containing triple therapy.110,111 These meta-analyses have recently been updated to include 13 studies with a total of 1709 patients (1011 with levofloxacin-containing triple treatment and 698 with bismuth quadruple therapy).109 This meta-analysis showed a non-statistically significant tendency towards higher eradication efficacy of the levofloxacin-containing triple treatment compared to the bismuth-containing quadruple therapy (79% vs 70%; odds ratio [OR]=1.43; 95% confidence interval [95% CI]=0.88–2.31), with a significantly lower rate of adverse effects (14% vs 32%; OR=0.30; 95% CI=0.19–0.50) and serious adverse effects (0.7% vs 7.8%; OR=0.15; 95% CI=0.04–0.59). Ten-day levofloxacin-containing triple therapy was more effective than the 7-day course (89% vs 70%). Finally, a sub-analysis that included only studies that administrated a triple regimen with PPI, levofloxacin and amoxicillin for 10 days showed that this is more effective than a bismuth-containing quadruple therapy (89% vs 66%; OR=4.22; 95% CI=2.84–6.26).
These promising results with levofloxacin have recently been confirmed in a large Spanish multicentre study, in which 1000 patients in whom first-line eradication treatment with PPI, amoxicillin and clarithromycin had failed received PPI, amoxicillin and levofloxacin for 10 days.112 Eradication was achieved in 74% of patients, and although adverse effects were described in one fifth of cases, none of these was serious. This study also assessed whether efficacy diminished over time, since resistance to quinolones in Spain appears to be rising rapidly. However, the eradication rates remained stable over the 6 years of the study.112
Nevertheless, the efficacy of levofloxacin-containing triple therapy can evidently be improved (remember that our current therapeutic objective is to reach an eradication efficacy greater than or equal to 90% and we will not settle for lower rates in either initial or rescue treatment). Moreover, as mentioned, the rate of resistance to quinolones is increasing relatively fast, which could negatively impact the efficacy of triple therapy. It has been suggested that this negative effect could be reduced with the addition of bismuth. In this respect, a recent study has shown that the addition of bismuth (PPI, amoxicillin, levofloxacin and bismuth for 14 days) obtains a per-protocol eradication efficacy of 95%.113 The intention-to-treat efficacy was also high: 88%. These figures were higher than those obtained with (standard) triple treatment with PPI, amoxicillin and levofloxacin (without bismuth). These favourable results were obtained despite a high rate of resistance to quinolones (30%), higher than that described in our setting. This quadruple treatment (PPI, amoxicillin, levofloxacin and bismuth) achieved eradication in 98% of patients with quinolone-sensitive H. pylori strains and, more importantly, achieved eradication in a relatively high percentage (71%) of levofloxacin-resistant strains. However, when the standard levofloxacin-containing triple treatment was used, the infection was only eradicated in 38% of patients with quinolone-resistant strains.
Several studies have evaluated this levofloxacin-containing quadruple therapy (PPI, amoxicillin, levofloxacin and bismuth) as second-line treatment, as shown in Table 4, and have reported satisfactory eradication rates in general.113–118 Among these, a recent Spanish multicentre study administered a quadruple combination with esomeprazole (40mg/12h), amoxicillin (1g/12h), levofloxacin (500mg/24h) and bismuth (240mg/12h) for 14 days to 200 patients in whom triple (PPI, clarithromycin and amoxicillin) or non-bismuth quadruple therapy had previously failed.118 Ninety-six percent of the patients took the medication correctly. Overall, the per-protocol and intention-to-treat eradication rates were 91.1% and 90%, respectively. The figures were similar, regardless of the previous treatment. Almost half the patients (46%) presented adverse effects, but only 3% were classified as intense, and none was serious. The authors therefore concluded that a 14-day bismuth- and levofloxacin-containing quadruple therapy was a simple, safe and effective (≥90% cure) second-line therapy in patients with failure of triple eradication treatment. Nevertheless, it should be noted that estimates suggest that this treatment will fail to reach acceptable eradication rates (≥90%) if the proportion of levofloxacin-resistant H. pylori strains is >25%.119 In Spain, the most recently published studies report levofloxacin resistance rates of 15% in Cantabria,120 27% in Caceres31 and 13% in an Andalusian multicentre study,29 so the increase in quinolone resistance rates should be monitored locally.
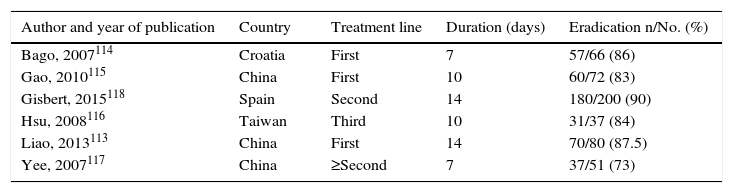
Studies that evaluated the efficacy (intention-to-treat) of the combination of PPI, amoxicillin, levofloxacin and bismuth for the eradication of Helicobacter pylori infection.
| Author and year of publication | Country | Treatment line | Duration (days) | Eradication n/No. (%) |
|---|---|---|---|---|
| Bago, 2007114 | Croatia | First | 7 | 57/66 (86) |
| Gao, 2010115 | China | First | 10 | 60/72 (83) |
| Gisbert, 2015118 | Spain | Second | 14 | 180/200 (90) |
| Hsu, 2008116 | Taiwan | Third | 10 | 31/37 (84) |
| Liao, 2013113 | China | First | 14 | 70/80 (87.5) |
| Yee, 2007117 | China | ≥Second | 7 | 37/51 (73) |
PPI: proton pump inhibitor.
Finally, it should be noted that a small study recently evaluated, for the first time, the efficacy of Pylera (which simplifies the administration of bismuth-containing quadruple therapy) in 49 patients with failure of one or more eradication treatments.121 The vast majority of patients had received one or several treatments with omeprazole, clarithromycin and amoxicillin; H. pylori was resistant to clarithromycin in 31 of the 49 (63%) patients. The 10-day Pylera treatment managed to eradicate H. pylori in 93% and 95% of patients in the intention-to-treat and per-protocol analysis, respectively.
After failure of non-bismuth quadruple therapyNon-bismuth quadruple therapies that include PPI, amoxicillin, clarithromycin and a nitroimidazole (especially in a concomitant regimen) are increasingly used as first-line treatment. It is a challenge to find rescue treatments following the failure of these therapies that use key antibiotics such as clarithromycin and nitroimidazoles.
For the present consensus, a systematic review with meta-analysis was performed to evaluate which second-line treatments have been investigated after a failed attempt to eradicate H. pylori infection with these therapies. Studies were selected if they evaluated the efficacy of second-line regimens after the failure of first-line therapies such as sequential, concomitant or hybrid regimens. Studies in which the second-line treatment was chosen according to antibiotic sensitivity, or which lacked a detailed description of the composition of the therapies (administered as first-line or rescue) were excluded. The data were synthesised by intention-to-treat eradication rate and, when possible, meta-analyses were performed using the inverse variance method.
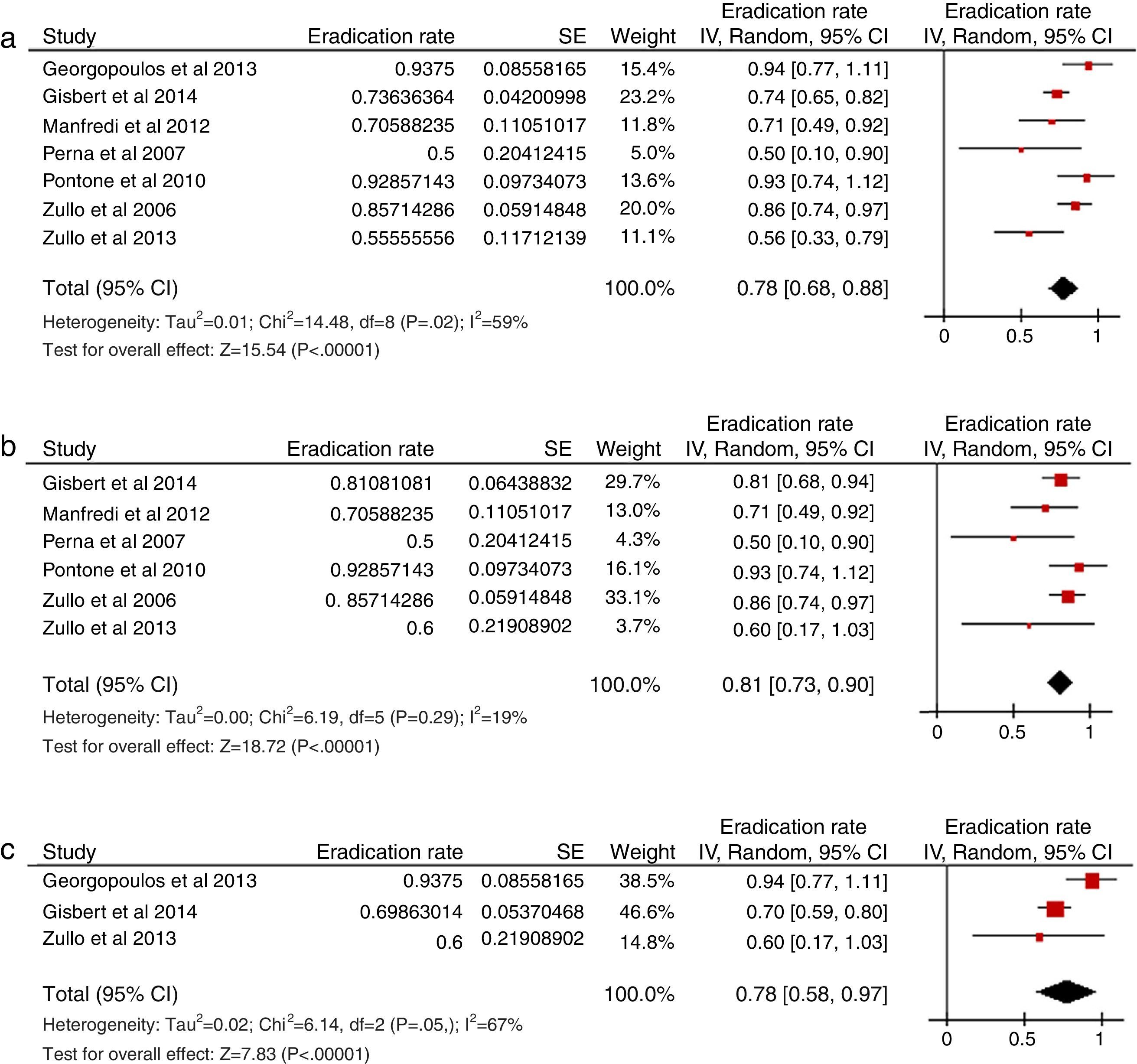
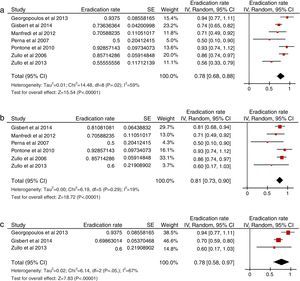
Sixteen studies were selected using this strategy: 7 included patients in whom concomitant treatment had failed, 15 in whom sequential treatment had failed, and 1 in whom hybrid treatment had failed. Most of the studies evaluated a rescue therapy with PPI, amoxicillin and levofloxacin, a combination that obtained an overall eradication rate of 78% following failure of non-bismuth quadruple therapy (Fig. 4a).36,37,122–126 The rescue regimen was administered for 10 days in all the studies, and in all except one,122 250mg of levofloxacin was prescribed twice daily. This triple therapy (PPI, amoxicillin and levofloxacin) was effective after failure of both sequential (81%) (Fig. 4b)37,122–126 and concomitant treatment (78%) (Fig. 4c).36,37,122 Only 1 study37 evaluated the results of levofloxacin-containing triple therapy after the failure of hybrid therapy, with a 50% cure rate. Tolerance to this rescue regimen was generally good.
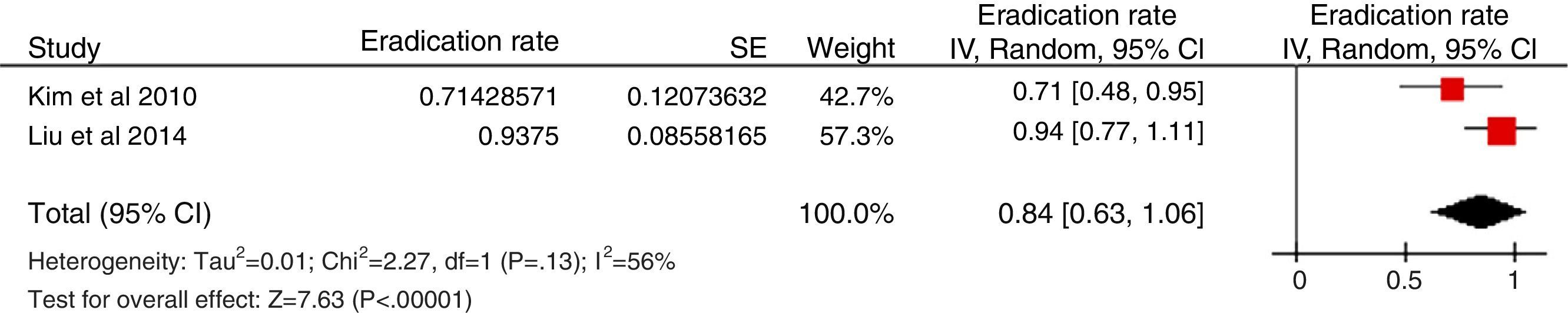
(a) Efficacy (intention to treat) of a second-line treatment with PPI, amoxicillin and levofloxacin after failure of a non-bismuth quadruple therapy (sequential or concomitant). (b) Efficacy (intention-to-treat) of a second-line treatment with PPI, amoxicillin and levofloxacin after failure of a sequential therapy. (c) Efficacy (intention-to-treat) of a second-line treatment with PPI, amoxicillin and levofloxacin after failure of a concomitant therapy.
Some authors have used moxifloxacin instead of levofloxacin in this triple rescue regimen (i.e. PPI, amoxicillin and moxifloxacin); the mean eradication rate was 71% (238 patients) after the failure of non-bismuth quadruple therapies.127–129 These results should be interpreted with caution, due to the high heterogeneity of the studies and the differences in the study characteristics (e.g. the duration and dose of moxifloxacin were different in each study).
As previously mentioned, an important aspect of levofloxacin-containing therapy is that it is less effective in the presence of resistance to fluoroquinolones.130 Thus, recent studies suggest that the efficacy of levofloxacin-containing triple therapy is decreasing, probably due to the increase in these resistances.131 Similarly, bismuth seems to have a synergic effect with certain antibiotics and to overcome resistance to clarithromycin and levofloxacin to a large extent.113,132 Accordingly, some authors have evaluated a quadruple regimen adding bismuth to levofloxacin (i.e. PPI, amoxicillin, levofloxacin and bismuth), obtaining encouraging results.113–118 A recent Spanish multicentre study evaluated the efficacy of a quadruple combination with PPI, amoxicillin, levofloxacin and bismuth for 14 days in 200 patients in whom triple or non-bismuth quadruple therapy (either sequential or concomitant) had previously failed, obtaining per-protocol and intention-to-treat eradication rates of 91.1% and 90%, respectively.118 These figures were similar, regardless of the previous treatment: triple therapy 88.5% vs sequential 93.8% vs concomitant 91.9%. Therefore, 14-day bismuth- and levofloxacin-containing quadruple therapy is an effective second-line therapy (≥90% cure) not only in patients following failure of standard triple therapy, but also in those with failure of quadruple sequential or concomitant therapy; the results are even better than those described with levofloxacin-containing triple therapy.
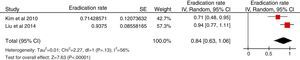
Only 2 studies to date (both with small sample sizes) have evaluated the efficacy of standard quadruple therapy (PPI, bismuth, tetracycline and metronidazole) following the failure of a non-bismuth quadruple therapy (sequential in both cases) (Fig. 5). In the first, the infection was eradicated in 8 patients (100%) treated with a bismuth-containing quadruple therapy for 10 days133; in the second, the infection was eradicated in 10 of 14 patients (71%) treated for 14 days.134
There is very little evidence on other treatment options. Hsu et al.135 evaluated a modified bismuth-containing quadruple therapy (administering levofloxacin instead of metronidazole) after failure of the sequential regimen, obtaining an eradication rate of 96%. Fakheri et al.136 evaluated a hybrid therapy with pantoprazole, amoxicillin and bismuth subcitrate for 14 days following failure of a sequential regimen, adding furazolidone for the first week only; the infection was eradicated in 81% of patients. Finally, Liou et al.137 analysed the efficacy of a modified sequential therapy administered for 14 days (lansoprazole and amoxicillin administered for the first 7 days, followed by lansoprazole, metronidazole and levofloxacin for a further 7 days) following failure of the sequential treatment, achieving an eradication rate of 80%.
In summary, triple therapy with PPI, amoxicillin and levofloxacin was the most widely evaluated rescue regimen after failure of non-bismuth quadruple therapies, reaching eradication rates close to 80%. More recently, bismuth has been considered as a valuable adjuvant in levofloxacin-containing triple therapy; therefore, quadruple therapy (PPI, amoxicillin, levofloxacin and bismuth) may be considered preferable to triple therapy as rescue therapy, although experience with this regimen is still limited. Finally, bismuth-containing quadruple therapy (PPI, bismuth, tetracycline and metronidazole) has obtained encouraging results as rescue treatment, but as previously mentioned, has only been evaluated in 2 small studies.
• Recommendation 9. Following failure of a first treatment with a bismuth-containing quadruple regimen (PPI, bismuth, tetracycline and metronidazole), a levofloxacin-containing triple or quadruple regimen is recommended (PPI, amoxicillin, levofloxacin±bismuth).
Agreement: 100%; votes: completely agree (100%). GR: strong. CE: low.
Following failure of a bismuth-containing quadruple therapy, any treatment can theoretically be used, including repetition of the same bismuth-containing quadruple therapy, since the rate of acquired resistance following the use of amoxicillin, bismuth or tetracycline is insignificant (<3%) and resistance to metronidazole can be partially overcome with higher doses and longer duration of the antibiotic.21 Nevertheless, it does not appear logical to repeat treatment that has already failed. It also seems reasonable to assume that bismuth-containing quadruple treatment was used as a first option due to the high rate of clarithromycin resistance (which reduces the efficacy of triple therapy) and dual clarithromycin and metronidazole resistance (which is associated with lower efficacy of non-bismuth quadruple therapies).21
Experience after failure of bismuth-containing quadruple therapy is very scant. In this context, the Maastricht IV consensus recommended the use of a levofloxacin-containing triple regimen.18 Studies that have evaluated the efficacy of a third-line treatment combining PPI, amoxicillin and levofloxacin for H. pylori eradication following the failure of 2 treatments, the second-line treatment being the bismuth-containing quadruple regimen, are summarised in Table 5 (efficacy between 60% and 85%).138–142
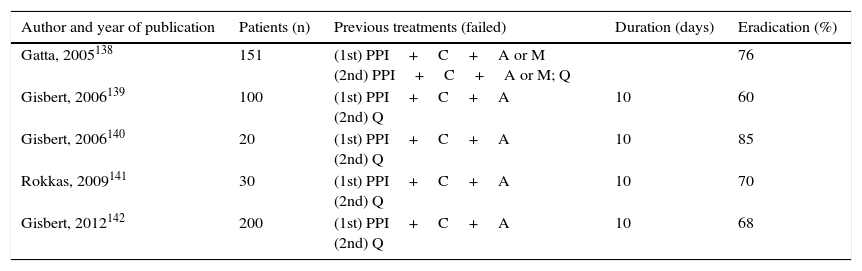
Studies that evaluated the efficacy (intention-to-treat) of a third-line combination with PPI, amoxicillin and levofloxacin for the eradication of Helicobacter pylori infection after 2 eradication failures.
| Author and year of publication | Patients (n) | Previous treatments (failed) | Duration (days) | Eradication (%) |
|---|---|---|---|---|
| Gatta, 2005138 | 151 | (1st) PPI+C+A or M (2nd) PPI+C+A or M; Q | 76 | |
| Gisbert, 2006139 | 100 | (1st) PPI+C+A (2nd) Q | 10 | 60 |
| Gisbert, 2006140 | 20 | (1st) PPI+C+A (2nd) Q | 10 | 85 |
| Rokkas, 2009141 | 30 | (1st) PPI+C+A (2nd) Q | 10 | 70 |
| Gisbert, 2012142 | 200 | (1st) PPI+C+A (2nd) Q | 10 | 68 |
A: amoxicillin; C: clarithromycin; PPI: proton pump inhibitor; M: metronidazole; Q: bismuth-containing quadruple therapy (PPI, bismuth, tetracycline and metronidazole).
Very recently, a Korean study carried out in 28 patients showed that moxifloxacin-containing triple therapy achieved an eradication rate of 67% as second-line treatment following the failure of a bismuth-containing quadruple treatment.128
In a study conducted in China, bismuth-containing therapy was effective as first-line treatment in 99% of patients, and in the 2 patients in whom it failed, sequential therapy (PPI and amoxicillin, followed by PPI, clarithromycin and metronidazole) was effective.133 However, the use of a second-line clarithromycin-containing treatment following failure of a bismuth-containing quadruple therapy does not generally seem to be useful in clinical practice, as this bismuth-containing quadruple therapy is usually recommended as first-line treatment precisely because of high resistance to clarithromycin in some areas. In contrast, it is well known that levofloxacin-containing triple therapy is effective as second-line treatment after failure of a therapy containing clarithromycin110,111,143; therefore, this would seem more advisable after failure of a bismuth-containing quadruple regimen.
Finally, as previously mentioned (see section on rescue treatment following failure of triple or non-bismuth quadruple therapy), the addition of bismuth to levofloxacin-containing triple therapy has achieved promising results; the efficacy of this combination (PPI, amoxicillin, levofloxacin and bismuth) as rescue treatment following the failure of bismuth-containing quadruple therapy should be evaluated in the future.
• Recommendation 10. Rescue treatment in penicillin-allergic patients:
- (a)
After failure of a first triple treatment (PPI, clarithromycin and metronidazole), bismuth-containing quadruple therapy (PPI, bismuth, tetracycline and metronidazole) is suggested.
- (b)
After failure of a first bismuth-containing quadruple treatment, triple therapy with PPI, levofloxacin and clarithromycin is suggested.
Agreement: 100%; votes: completely agree (100%). GR: weak. CE: very low.
The eradication of H. pylori in penicillin-allergic patients is a challenge, especially in those in whom a previous eradication attempt has failed. In a Spanish pilot study, 15 patients allergic to penicillin in whom a first treatment with PPI, clarithromycin and metronidazole had failed received a second treatment with PPI, clarithromycin and levofloxacin for 10 days.85 Compliance was total in all cases. Adverse effects were described in 20% of patients, all mild. The eradication rate (intention-to-treat) was 73%.
More recently, in a Spanish multicentre study, 267 penicillin-allergic patients received a first-line treatment with PPI, clarithromycin and metronidazole or bismuth-containing quadruple therapy (PPI, bismuth, tetracycline and metronidazole), and as rescue treatments, a bismuth-containing quadruple therapy or regimen with PPI, clarithromycin and levofloxacin for 10 days.90 The intention-to-treat eradication rate with PPI, clarithromycin and levofloxacin was 64%, after failure of both first-line PPI, clarithromycin and metronidazole and bismuth-containing quadruple therapy, and compliance was 88–100%, with 23–29% adverse effects (all mild). The authors therefore concluded that triple treatment with PPI, clarithromycin and levofloxacin is an alternative second-line treatment in patients allergic to penicillin. The possibility of increasing the efficacy of the latter combination by optimising the PPI dose and duration of treatment, or by adding bismuth, should be explored in the future.
Liang et al.91 randomised 109 penicillin-allergic patients (in most of whom PPI, clarithromycin and metronidazole had failed) to receive standard bismuth-containing quadruple therapy (PPI, bismuth, tetracycline and metronidazole) for 2 weeks, or a modified bismuth-containing quadruple regimen (PPI, bismuth, tetracycline and furazolidone; the latter antibiotic is not available in Spain). The intention-to-treat and per-protocol eradication rates were 88% and 92%, respectively.
In a retrospective study, Furuta et al.144 treated 28 patients allergic to penicillin with PPI, metronidazole and sitafloxacin for 1 or 2 weeks, achieving H. pylori eradication in all patients. These encouraging results were obtained despite a high rate of resistance to levofloxacin (60%), and could be explained by the fact that the minimum inhibitory concentration (MIC) of sitafloxacin is lower than that of levofloxacin, and could be effective in patients infected by strains with mutations in the gyrA genes (a genetic marker of levofloxacin resistance).145 However, in this study, the sitafloxacin MICs were not determined and, therefore, the prevalence of strains resistant to this antibiotic is not known; it is also unclear whether the regimen used in this study is effective in patients with sitafloxacin-resistant H. pylori strains. Obviously, the efficacy of this sitafloxacin-based regimen must be confirmed in future studies.
Finally, Tay et al.146 prescribed a quadruple regimen containing PPI, bismuth, ciprofloxacin and rifabutin to a group of 69 patients allergic to penicillin in whom at least one standard triple treatment (usually PPI, clarithromycin and metronidazole) had failed, achieving an eradication rate of 94%. It should be noted, however, that the authors systematically carried out cultures and only used this regimen in patients with strains sensitive to quinolones, which could explain the excellent results obtained in this study.
In summary, in patients allergic to penicillin, bismuth-containing quadruple therapy (PPI, amoxicillin, tetracycline and metronidazole) is suggested after failure of triple treatment (PPI, clarithromycin and metronidazole), while triple therapy with PPI, levofloxacin and clarithromycin is suggested after failure of a first bismuth-containing quadruple treatment.
• Recommendation 11. Following failure of a first treatment with clarithromycin and a second line with levofloxacin, a bismuth-containing quadruple treatment (PPI, bismuth, tetracycline and metronidazole) is recommended.
Agreement: 100%; votes: completely agree (100%). GR: strong. CE: very low.
Following the failure of a clarithromycin-containing triple or quadruple combination, triple therapy with PPI, amoxicillin and levofloxacin is often recommended.5 This second treatment also fails sometimes, and in these cases, a bismuth-containing quadruple therapy (PPI, bismuth, tetracycline and metronidazole) is usually prescribed.13 The choice of rescue treatment depends on the drugs that have been used in previous eradication attempts. Since repetition of the same antibiotic is not recommended (with the well-known exceptions of bismuth, amoxicillin and, to a lesser degree, metronidazole), bismuth-containing quadruple therapy currently seems to be the best option, since it basically avoids re-administration of clarithromycin and levofloxacin and, therefore, is usually used in clinical practice in our setting.13
Nevertheless, experience with this quadruple regimen following failure of 2 eradication treatments is very scant. A Spanish multicentre study was recently conducted to evaluate the efficacy of bismuth-containing quadruple therapy as third-line treatment.147 One advantage of this regimen is that it is not affected by resistance to either clarithromycin or the fluoroquinolones (antibiotics used in the first and second eradication attempt, respectively). Thus, the study included consecutive patients in whom a first treatment with PPI, clarithromycin and amoxicillin, and a second treatment with PPI, amoxicillin and levofloxacin had failed. A third eradication treatment was administered with PPI (at standard dose every 12h), bismuth subcitrate (120mg/6h or 240mg/12h), tetracycline (between 250mg/8h and 500mg/6h) and metronidazole (between 250mg/8h and 500mg/6h) for 7–14 days. Two hundred patients were included, 2 of whom were lost to follow-up. The intention-to-treat eradication rate was 65%. Adverse effects were described in 22% of cases, none of them serious.
Following failure of 2 eradication treatments, one option is to perform culture and antibiotic sensitivity testing in order to select the most appropriate antibiotic combination based on the bacterial susceptibility.
Although this “susceptibility-guided” treatment option is usually recommended in other consensuses, its superiority over empirical treatment has not been sufficiently confirmed. A sub-analysis of studies that included second-line treatments in a recent meta-analysis11 and literature review12 comparing the efficacy of empirical treatment against therapy based on antibiotic susceptibility was unable to demonstrate statistically significant differences between both strategies. No randomised clinical trials were identified that compared empirical treatment against susceptibility-guided treatment using antibiotic sensitivity testing as third-line therapy, but the mean eradication rate in the studies that used the culture-based strategy was only 72%.11
As previously stated, the comments included in this consensus document were based on the assumption that the antibiotic susceptibility is unknown. Furthermore, most of the authors of this document believe there to be arguments for not systematically performing culture before indicating a third eradication treatment, and that administration of an empirical treatment should be recommended after failure of a second attempt. This recommendation is based on the fact that H. pylori culture is available in very few centres, it requires an invasive test (upper gastrointestinal endoscopy), has a sensitivity of less than 90%, and an apparent conflict between in vitro results and the in vivo eradication rate.148 Furthermore, culture only provides useful information on some antibiotics already used in previous first- (clarithromycin and metronidazole) and second-line eradication treatments (levofloxacin), which, by definition, should not be used again.
In summary, it can be concluded that bismuth-containing quadruple empirical rescue treatment is a valid alternative after failure of one treatment with clarithromycin and another with levofloxacin.
• Recommendation 12. Following failure of a first treatment with clarithromycin and a second-line bismuth-containing quadruple treatment (PPI, bismuth, tetracycline and metronidazole), a levofloxacin-containing treatment is recommended.
Agreement: 100%; votes: completely agree (100%). GR: strong. CE: low.
After failure of a clarithromycin-containing triple or quadruple treatment, quadruple therapy with PPI, bismuth, tetracycline and metronidazole is often recommended.5,13 When this second treatment also fails, and in order to avoid reusing either clarithromycin or metronidazole, it has been suggested that a triple regimen with PPI, amoxicillin and levofloxacin be prescribed.5,13
Nevertheless, experience with this combination following failure of 2 eradication treatments is scant. A few years ago, a Spanish multicentre study was published that evaluated the efficacy of levofloxacin-containing triple therapy as third-line treatment, achieving eradication in approximately 70% of cases.139 These results were recently confirmed in a larger national multicentre study that included a total of 200 patients.142 It included consecutive patients in whom a first treatment with PPI, amoxicillin and clarithromycin, and a second treatment with a bismuth-containing quadruple regimen (PPI, bismuth, tetracycline and metronidazole) had failed. A third eradication treatment with PPI, amoxicillin and levofloxacin was administered for 10 days. The intention-to-treat eradication rate was 68%. Adverse effects were described in 19% of cases, none of them serious.
Other authors have also obtained acceptable results with this third-line levofloxacin-containing triple treatment, with eradication rates that have varied between 60% and 86%, as summarised in Table 5.138–142
Therefore, it can be concluded that empirical triple rescue treatment with PPI, amoxicillin and levofloxacin is a third-line alternative after the failure of 2 previous eradication therapies containing key antibiotics such as amoxicillin, clarithromycin, metronidazole and tetracycline. There are still no published studies with levofloxacin-containing quadruple therapy (adding bismuth to treatment with PPI, amoxicillin and levofloxacin) which, as we have previously seen, increases the efficacy of second-line levofloxacin-containing triple therapy by 15%118; however, by analogy it seems reasonable that it is also a good alternative in this case.
• Recommendation 13. Following failure of a first bismuth-containing quadruple treatment (PPI, bismuth, tetracycline and metronidazole), and a second-line levofloxacin-containing regimen, quadruple concomitant treatment (PPI, amoxicillin, clarithromycin and metronidazole) is suggested.
Agreement: 100%; votes: completely agree (100%). GR: weak. CE: very low.
In this case (failure of a first bismuth-containing quadruple treatment and a second-line levofloxacin-containing treatment), since clarithromycin was not previously used, it is suggested to use a non-bismuth quadruple treatment (concomitant), which is precisely the first-line treatment of choice in our setting. It should be mentioned that this recommendation is not based on any direct evidence, but is established instead on indirect data, theoretical assumptions and the absence of other effective therapeutic alternatives.
Another option is to re-use the bismuth with amoxicillin and tetracycline (drugs with an acquired resistance rate of <3%), but combined with other antibiotics not previously employed, such as furazolidone (although this drug is not currently available in our setting).149 The efficacy of this strategy has been recently demonstrated,91 and it has been included in the latest consensus therapeutic recommendations in China,62 where the rates of primary resistance to clarithromycin and levofloxacin are so high that they preclude the use of treatments with these antibiotics for H. pylori infection.
• Recommendation 14. Following the failure of a third treatment, it is suggested that the need to eradicate the infection should be re-evaluated and, if applicable, a fourth line with rifabutin (PPI, amoxicillin and rifabutin) should be prescribed.
Agreement: 100%; votes: completely agree (92.3%); mostly agree (7.7%). GR: weak. CE: very low.
H. pylori infection occasionally persists despite having administered 3 eradication treatments.148 Since it is not known whether the benefit obtained by the potential eradication of H. pylori exceeds the risks associated with more complex treatment lines, the indication for eradication treatment and the possibility of administering maintenance antisecretory therapy should be re-evaluated individually in these patients. Obviously, the decision to prescribe a fourth treatment line will be clearer the greater the benefit of H. pylori eradication, as is the case in patients with peptic ulcer (especially if they have had previous complications) or with gastric MALT lymphoma.
A recent literature review evaluated the role of rifabutin–an antibiotic with high in vitro activity against H. pylori–in the treatment of this infection.150 The mean rate of H. pylori resistance to rifabutin (calculated from 11 studies, including 2982 patients) was 1.3%. When only studies that included patients with no previous eradication treatments were considered, this figure was even lower (0.6%). Overall, the mean H. pylori eradication rate (by intention-to-treat analysis) with combinations that included rifabutin (1008 patients) was 73%. Specifically, the eradication rate for the fourth/fifth-line rifabutin-containing treatments (95 patients) was 79%.139,151–156 Most studies used 300mg/day of rifabutin for the treatment of H. pylori infection, a dose that seems to be more effective than the 150mg/day dose. The optimal duration of treatment has not been established, but 10–12 days is generally recommended. The mean incidence of adverse effects was 22%; of these, myelotoxicity, although rare, was the most important (so follow-up complete blood count should be performed at the end of treatment); to date, leukopenia has resolved without incident in all patients within a few days of completing treatment, and no infections or other complications associated with the myelotoxicity have been described.150
These findings have recently been confirmed in a Spanish multicentre study that evaluated the efficacy of a fourth empirical rifabutin-containing rescue treatment in patients in whom 3 previous eradication attempts had failed (the first with PPI, clarithromycin and amoxicillin; the second with a quadruple therapy with PPI, bismuth, tetracycline and metronidazole, and a third with PPI, amoxicillin and levofloxacin).157 A fourth eradication treatment with PPI, amoxicillin (1g/12h) and rifabutin (150mg/12h) was administered for 10 days. One hundred consecutive patients were included. Eight patients did not take the medication correctly (in 6 cases due to adverse effects). The intention-to-treat eradication rate was 50%. Adverse effects were reported in 30 patients (30%). Mild myelotoxicity, observed in 4% of patients, resolved spontaneously in all cases after completion of treatment. It was therefore concluded that even after failure of 3 previous treatments, a fourth empirical rescue therapy with rifabutin (together with PPI and amoxicillin) may be effective for eradicating H. pylori infection in approximately half of cases. Finally, although the evidence in this respect is very limited,146,158 when multiple eradication attempts have failed, combining bismuth with rifabutin in order to increase eradication efficacy can be considered.
In summary, after the failure of a third treatment, the need to eradicate the infection and the possibility of administering maintenance antisecretory therapy should be carefully evaluated. If eradication is considered necessary, the need for a fourth line of treatment, for example with rifabutin, should be assessed individually, with strict patient monitoring and follow-up.
• Recommendation 15. In patients with uncomplicated duodenal ulcer who do not require non-steroidal anti-inflammatory drugs (NSAID)/aspirin, antisecretory treatment should not be maintained after completing H. pylori eradication treatment.
Agreement: 100%; votes: completely agree (92.9%); mostly agree (7.1%). GR: strong. CE: high.
Initially, most authors who used PPIs in eradication therapies for uncomplicated duodenal ulcer disease (with no gastrointestinal bleeding or perforation) prolonged the use of these drugs for 2–4 weeks after conclusion of antibiotic treatment in order to ensure ulcer healing.159 However, it has been found that limiting administration of PPIs to the duration of antibiotic treatment is sufficient to achieve a high rate of ulcer healing in these patients. A systematic review of the medical literature identified 24 studies with a total of 2378 patients in which ulcer healing was evaluated after 7 days of PPI plus 2 antibiotics.160 The overall (both success and failure of H. pylori eradication) mean healing rate (intention-to-treat) was 86%. This figure rose to 95% when only those patients in whom the infection had been eradicated were included. The meta-analysis of the 6 randomised studies161–166 that compared efficacy in terms of ulcer healing with PPI plus 2 antibiotics for 7 days versus the same treatment with PPI prolonged for a further 2–4 weeks160 found ulcer healing in 91% and 92% of cases, respectively. The OR for this comparison was 1.11 (95% CI=0.71–1.74), with homogeneous results. Finally, a sub-analysis of patients with duodenal ulcer found similar results (OR 1.14, with 95% CI=0.71–184). Two other randomised studies were conducted subsequent to the publication of this meta-analysis, with similar outcomes.167,168
In summary, it can be concluded that a PPI administered for the same duration as antibiotic therapy is sufficient to obtain a high rate of healing in uncomplicated duodenal ulcer in patients who do not take NSAID or aspirin. Nevertheless, in the case of complicated duodenal ulcers (gastrointestinal bleeding, perforation), it is prudent to administer antisecretory agents until H. pylori eradication is confirmed.
• Recommendation 16. In patients with gastric ulcer who do not require NSAID/aspirin, antisecretory treatment should be maintained for 4–8 weeks after completing H. pylori eradication treatment.
Agreement: 100%; votes: completely agree (100%). GR: strong. CE: moderate.
Two medical literature reviews published more than a decade ago provide arguments in favour of not prolonging antisecretory treatment in patients with gastric ulcer, in line with the approach taken with duodenal ulcers. The first of these concludes that “H. pylori eradication was found to induce a better response in peptic ulcer healing, regardless of diagnosis (duodenal or gastric)”.169 The other systematic review reached the conclusion that “the eradication of H. pylori cures both gastric and duodenal ulcer, and the cure rates are similar”.170 From these data, it can be concluded that the healing rate with H. pylori eradication treatment was similar for both gastric and duodenal ulcers.
However, recent studies suggest the need to prolong antisecretory treatment, especially in gastric ulcers larger than 1cm. An initial study documented 100% healing of gastric ulcers smaller than 1cm 8 weeks after the administration of a 2-week eradication treatment.171 The healing rate was considerably reduced when the ulcers were larger than 1cm; it is important to note that all the ulcers that had not healed at 8 weeks disappeared after additional PPI treatment. One of the randomised studies that provides highly relevant information on this subject evaluated gastric ulcer healing in patients infected with H. pylori after 1-week eradication treatment or 8-week PPI therapy.172 It was found that the healing rate 8 weeks after eradication treatment was exponentially reduced according to the size of the ulcer (89% for ulcers <1cm, 54% for ulcers between 1 and 1.4cm and 5% for those ≥1.5cm), while it was significantly higher in the group treated with PPI for 8 weeks (100% for ulcers <1cm, 77% for ulcers between 1 and 1.4cm and 77% for those ≥1.5cm).172
More recently, another randomised study was published comparing the administration of eradication therapy alone versus this therapy followed by a PPI for 3 weeks.173 Gastric ulcer healing at 4 weeks was lower in patients treated with triple therapy alone, without subsequent PPIs (64% vs 82%). Similarly, in patients with unhealed gastric ulcer, 1 additional 4-week cycle of a PPI (esomeprazole) increased this percentage to 89–96%. It should be noted that this study has some methodological defects, such as the exclusion of patients with ulcers >2cm and excessively early endoscopic follow-up of the healing (4 weeks) for a gastric ulcer.
Finally, a recent Japanese study randomised 115 patients with gastric ulcer stratified according to the size of the lesion (<0.5cm, 0.5–1.5cm and >1.5cm) to receive eradication treatment (for 1 week) plus 7 weeks with PPI versus eradication treatment plus 7 weeks of a cytoprotective agent.168 The ulcer healing rates at 8 weeks were significantly higher in the group with eradication treatment plus PPI. Consistent with previous studies, the ulcer healing results with eradication treatment plus PPI were better for gastric ulcers >1.5cm (85% vs 43%).
In summary, the scant evidence available points to a higher ulcer healing rate with eradication treatment followed by PPI for gastric ulcers associated with H. pylori infection. All the aforementioned studies168,172,173 found a lack of healing of up to 20% with eradication treatment alone, or even higher in the case of large ulcers. It is therefore recommended that after completing eradication treatment, antisecretory therapy should be prolonged between 4 and 8 weeks in gastric ulcers, especially in those larger than 1cm. Finally, it should be remembered that after completing eradication treatment and subsequent PPI, endoscopic surveillance should be carried out to confirm ulcer healing.
• Recommendation 17. In patients with gastrointestinal bleeding due to peptic ulcer, eradication of H. pylori eliminates virtually all recurrences; therefore, once the eradication has been confirmed, and in the absence of NSAID/aspirin treatment, antisecretory maintenance treatment should not be administered.
Agreement: 100%; votes: completely agree (100%). GR: strong. CE: high.
Peptic ulcer is the leading cause of upper gastrointestinal bleeding, and H. pylori is the main aetiological factor in gastroduodenal ulcer disease.174 Long-term antisecretory maintenance therapy has been the standard treatment to prevent re-bleeding in patients with a previous episode of gastrointestinal bleeding from peptic ulcer. Although it is amply known that H. pylori eradication is associated with a drastic decrease in ulcer recurrence, the efficacy of eradication treatment in the prevention of re-bleeding from peptic ulcer was unknown until recently.
A meta-analysis that followed the Cochrane Collaboration methodology was published in 2004 comparing the efficacy of H. pylori eradication treatment with antisecretory treatment for the prevention of re-bleeding from peptic ulcer.175,176 An initial sub-analysis included 7 studies with a total of 578 patients: the average percentage of re-bleeding in the eradication treatment group was 2.9% vs 20% (OR=0.17; 95% CI=0.10–0.32) in the group with neither eradication treatment nor maintenance antisecretory treatment. The second sub-analysis included 3 studies with a total of 470 patients: the average percentage of re-bleeding in the eradication treatment group was 1.6% vs 5.6% (OR=0.24; 95% CI=0.09–0.67) in the group given maintenance antisecretory treatment but no eradication treatment. Several studies have evaluated the incidence of re-bleeding in patients with confirmed H. pylori eradication who were followed-up without administering maintenance antisecretory treatment.177–196 Given that the duration of follow-up varies notably among the various studies, the follow-up periods of each study were taken into account and the respective annual re-bleeding rate was calculated (per patient and year of follow-up). Thus, the overall follow-up was 1913 patient-years, and 13 re-bleeding episodes were detected among patients in whom the bacterium had been eradicated; the annual recurrence was 0.88% per patient and year of follow-up.
These favourable results have been confirmed in a recent Spanish multicentre study that prospectively included 1000 patients with gastrointestinal bleeding from a peptic ulcer in whom H. pylori infection had been eradicated and antisecretory treatment was not subsequently prescribed.197 Three re-bleeding episodes were detected at 1 year of follow-up (in 2 cases after NSAID use and in 1 after H. pylori reinfection) and another 2 episodes at 2 years (1 after NSAID use and another after H. pylori reinfection). The cumulative incidence of re-bleeding was 0.5%, and the incidence rate was 0.15% per patient-year. From the aforementioned results, it can be deduced that treatment of H. pylori infection is more effective than antisecretory treatment (either with or without maintenance antisecretory agents) in preventing peptic ulcer re-bleeding. Consequently, the presence of H. pylori infection should be evaluated in all patients with gastrointestinal bleeding due to peptic ulcer, and eradication treatment prescribed in those who are infected. Once the eradication has been confirmed, it is not necessary to administer antisecretory maintenance treatment (if the patient does not require NSAID), as H. pylori eradication eliminates almost all bleeding recurrences. Nevertheless, it seems prudent that in a peptic ulcer that has presented complications (e.g. gastrointestinal bleeding), antisecretory drugs should be administered until H. pylori eradication is confirmed.
Conflict of interests of the participants at the IV Spanish Consensus Conference on the treatment of Helicobacter pylori infectionJavier P. Gisbert: scientific consultancy, support for research and training activities: Almirall, Allergan, AstraZeneca, Casen Recordati, Nycomed.
Javier Molina-Infante: scientific consultancy: Casen Recordati; training activities: Allergan, Zambón.
Javier Amador: none.
Fernando Bermejo: none.
Luis Bujanda: none.
Xavier Calvet: training activities: Allergan.
Manuel Castro-Fernández: training activities: Allergan.
Antonio Cuadrado: none.
J. Ignasi Elizalde: none.
Emili Gene: none.
Fernando Gomollón: none.
Ángel Lanas: none.
Carlos Martín de Argila: training activities: Allergan, Casen Recordati.
Fermín Mearin: none.
Miguel Montoro: scientific consultancy: Almirall.
Ángeles Pérez-Aisa: training activities: Allergan.
Emilio Pérez-Trallero: none.
Adrián G. McNicholl: training activities: Allergan.
Both these authors have contributed equally to the consensus.
Please cite this article as: Gisbert JP, Molina-Infante J, Amador J, Bermejo F, Bujanda L, Calvet X, et al. IV Conferencia Española de Consenso sobre el tratamiento de la infección por Helicobacter pylori. Gastroenterol Hepatol. 2016;39:697–721.