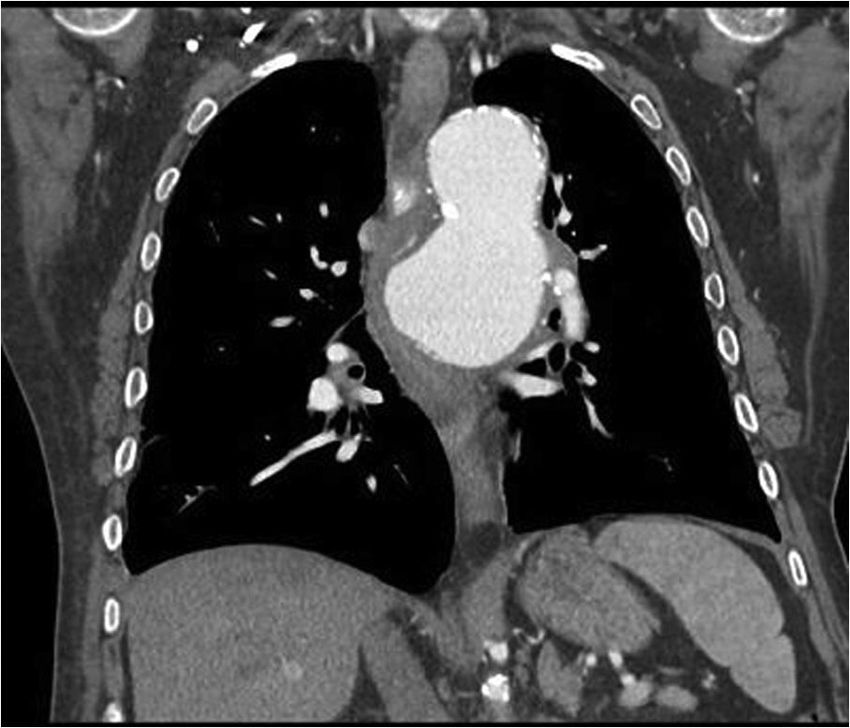
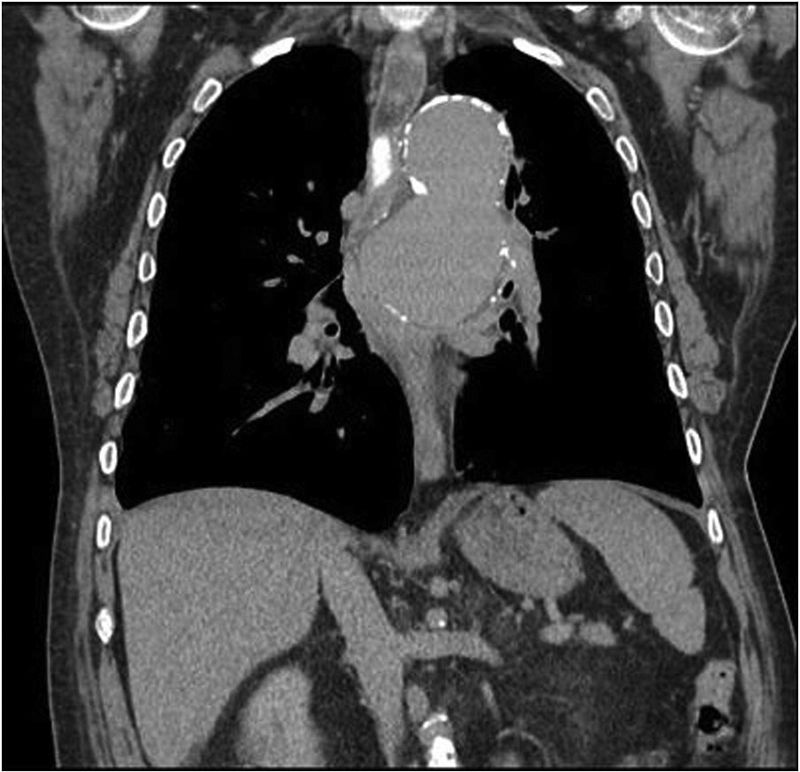
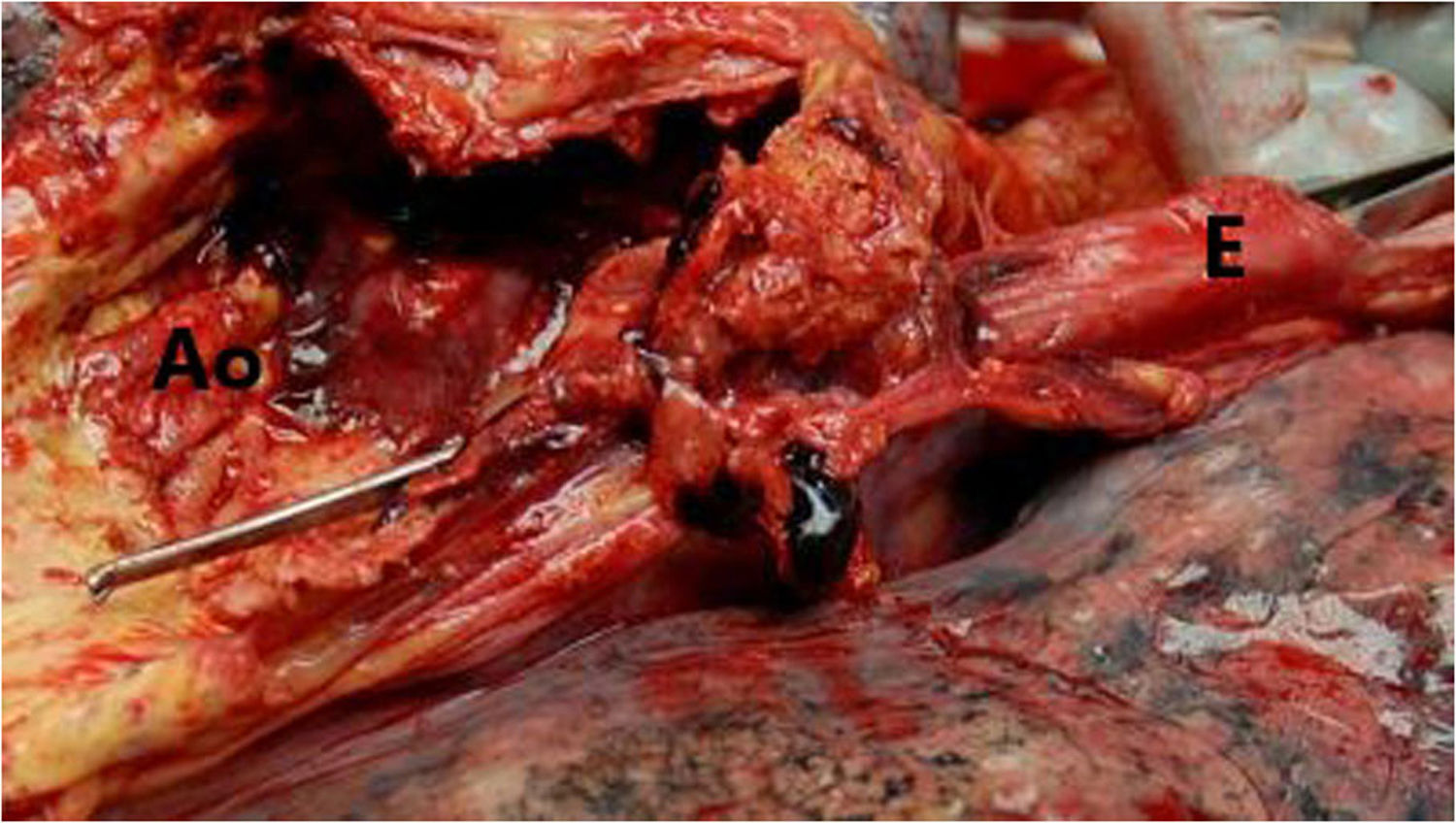
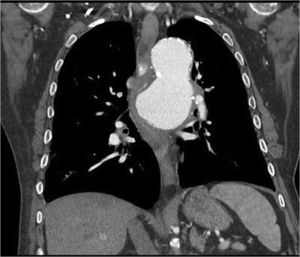
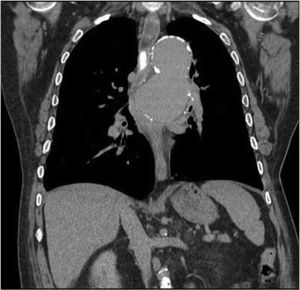
Sixty-four-year-old male with a history of thoracic aortic aneurysm who came to the emergency department due to the feeling of blockage at mid-oesophageal level which led to vomiting after eating. He denied bolus obstruction. He reported the presence of strands of blood in the most recent vomiting, as well as dyspnoea and orthopnoea. A chest X-ray showed an increase in the size of the aortic aneurysm, which led to a CT-angiogram being performed, showing hyperdense content in the oesophageal lumen, as well as signs of instability and penetrating ulcer which was in contact with and compressed the oesophageal lumen and the left bronchus (Figs. 1 and 2). Urgent surgery was performed with the fitting of an aortic stent, with no immediate complications. At 48h, the patients presented with haematemesis, with gastroscopy showing a mid-oesophageal clot and pulsating bleeding. In view of a suspected endoleak a surgical review was performed, with the arteriography showing no periprosthetic leakage. The patient presented with haemodynamic shock which did not respond to multiple transfusions or vasoactive drugs, leading to death. In the autopsy, the presence of an aortoesophageal fistula was confirmed (Fig. 3).
Oesophageal dysphagia secondary to extrinsic vascular compression is a rare cause of dysphagia, with the presence of cardiovascular abnormalities being the most common cause.1 Aortic dysphagia refers to dysphagia brought about by atherosclerosis or aortic aneurysm.2 Clinical manifestations of dysphagia and upper gastrointestinal haemorrhage may appear in complicated aneurysms, as in the case of our patient, with secondary aortoesophageal fistula being a complication with high mortality.3
Please cite this article as: Abanades Tercero M, Arribas Miranda C, Barón Rodiz PA, Romo Navarro Á. Disfagia esofágica secundaria a fístula aortoesofágica. Gastroenterol Hepatol. 2020;43:138–139.