Starting with Paul Langerhans, who first described pancreatic islets in 1869, this article reviews the various protagonists who, in the last century and a half, have contributed to the discovery of the main hormones originating in the pancreas, the analytical methods for their measurement, the imaging techniques for identifying tumoural location, and the various pancreatic neoplasms.
Tomando como punto de partida la descripción de los islotes pancreáticos realizada por Paul Langerhans en 1869 se efectúa una revisión histórica de los diferentes protagonistas que, aproximadamente, a lo largo de este último siglo y medio han contribuido a la identificación de las principales hormonas que tienen su origen en el páncreas, de los métodos analíticos que permiten cuantificarlas, de las técnicas de imagen que informan sobre la localización de los tumores y de los diferentes tipos de neoplasias que se originan en esta glándula.
Pancreatic neuroendocrine tumours (PNET) account for fewer than 3% of all pancreatic tumours, 1–2% of which are familial syndromes (multiple endocrine neoplasia-type 1 [MEN-I], Von-Hippel Lindau disease, neurofibromatosis type I or tuberous sclerosis). No sex or age predilection has been observed, although they are most common between 20 and 60 years of age. Clinically, they may be functioning or non-functioning. The former are diagnosed as a result of the symptoms produced by the various hormones that they secrete, while the latter are usually diagnosed incidentally following an imaging study performed on the patient for symptoms unrelated with the tumour, or due to the onset of pain.
The hormonesThe importance of understanding of the microscopic structure of the pancreatic gland cannot be overlooked in the context of PNET. It was a Parisian student called D. Moyse who apparently first described the structure of the pancreatic acini in his thesis published in 1852.1 Some years later, in 1869, Paul Langerhans (Berlin [Germany], 1847–1888), a student of Rudolph Virchow at the famous Berlin Pathological Institute, published his thesis Beiträge zur mikroskopischen Anatomie der Bauchspeicheldrüse2 (Contribution to the microscopic anatomy of the pancreas) in which he described (by means of staining studies with glycerine and Berlin blue), 9 different types of pancreatic cells, defining the structure, but not the function, of what years later became known as the islets of Langerhans. It was not until 1893 that French histologist Gustave Édouard Láguesse (Dijon [France], 1861–1927), professor of histology at Lille, finally insisted that the pancreatic islet cells should receive the name of their discoverer, Langerhans, and postulated that they generated hormones, specifically a substance that affected carbohydrate metabolism.3 This substance was first called insulin in 1909 by Belgian Jean de Meyer (1878–1934), although some attribute it to Scottish physiologist Edward Albert Sharpey-Shafer (Middlesex [United Kingdom], 1850–1935). Based on his findings, Láguesse coined the term “endocrine”, and paved the way for what is known as endocrinology; the term was later reiterated by Nicola Pende (Noicattaro [Italy], 1880–1970) in his treatise Endocrinologia. Patologia e clinica degli organi a secrezione interna, published in 1916.4
When talking about endocrinology, it is important to remember the concept of hormone. These are biochemical messengers secreted into the blood by the endocrine glands, and which act selectively on a target organ whose cells have specific surface receptors that enable the hormone to bind to them and produce its effect.
It is therefore helpful to bear in mind that in 1894, J.L. Dolinsky, a co-worker of Russian physiologist Ivan Petrovich Pavlov, observed that the introduction of acid into the duodenum caused pancreatic secretion, leading him to suspect that gastric acid stimulated this secretion, possibly by producing a substance that reached the pancreas through the circulation.5,6 Ernest Henry Starling (London [United Kingdom], 1866–1927) and his brother-in-law William Maddock Bayliss (Wolverhampton [United Kingdom], 1860–1924) named this substance secretin in 1902.5,7 In June 1905, Ernest Henry Starling gave a lecture to the Royal Society of Physicians entitled The chemical correlation of the functions of the body, in which he demonstrated how the cells of an organism communicated via chemical messengers that used the circulation to carry out their specific biological action at a distance. During a dinner at Gonville and Caius College, Cambridge, Starling is believed to have spoken with William Hardy, director of the college and renowned biologist, and suggested the convenience of finding a suitable word to designate that chemical messenger. Accordingly, they asked William Vesey, a colleague who was an expert in Greek, who suggested using the verb “opμαo” (hormaṓ, which means to excite or stimulate), and so the term “hormone” was born.8 This account appeared in an essay by Joseph Needman (a biochemist at Cambridge who was present during the conversation) entitled Order and life, published in 1936. William Maddock Bayliss was also attributed with the discovery that trypsin originated in the form of a proferment, which he called trypsinogen.9
In 1905, John Sidney Edkins (London [United Kingdom], 1863–1940) discovered a substance obtained from extracts of pyloric mucosa in anaesthetised cats, which induced the secretion of gastric acid and pepsin, and which he called gastrin.7 This finding was eclipsed, however, with the discovery of histamine in 1910, which had similar effects. Serious doubts were therefore raised with respect to Edkins's hypothesis regarding the existence of gastrin.
Roderick Alfred Gregory (London [United Kingdom], 1913–1990), a professor of physiology at the University of Liverpool, worked on biochemical processes of carbohydrate metabolism and the circulation, especially the heart. In 1939, he obtained a grant from the Rockefeller Foundation and worked in Andrew Conway Ivy's laboratory at Northwestern University (Illinois, USA), where he became interested in problems related to the gastrointestinal tract.10 He later returned to the Chemistry Department at Liverpool University, where he made important contributions to the study of intestinal hormones. In 1964, together with his co-worker, Hilda J. Tracy, he defined the chemical structure of gastrin, and discovered that this hormone was produced in excess in the tumours of patients with Zollinger-Ellison syndrome (described in 1955).11,12 These findings led to the acceptance of Edkins's original hypothesis.13
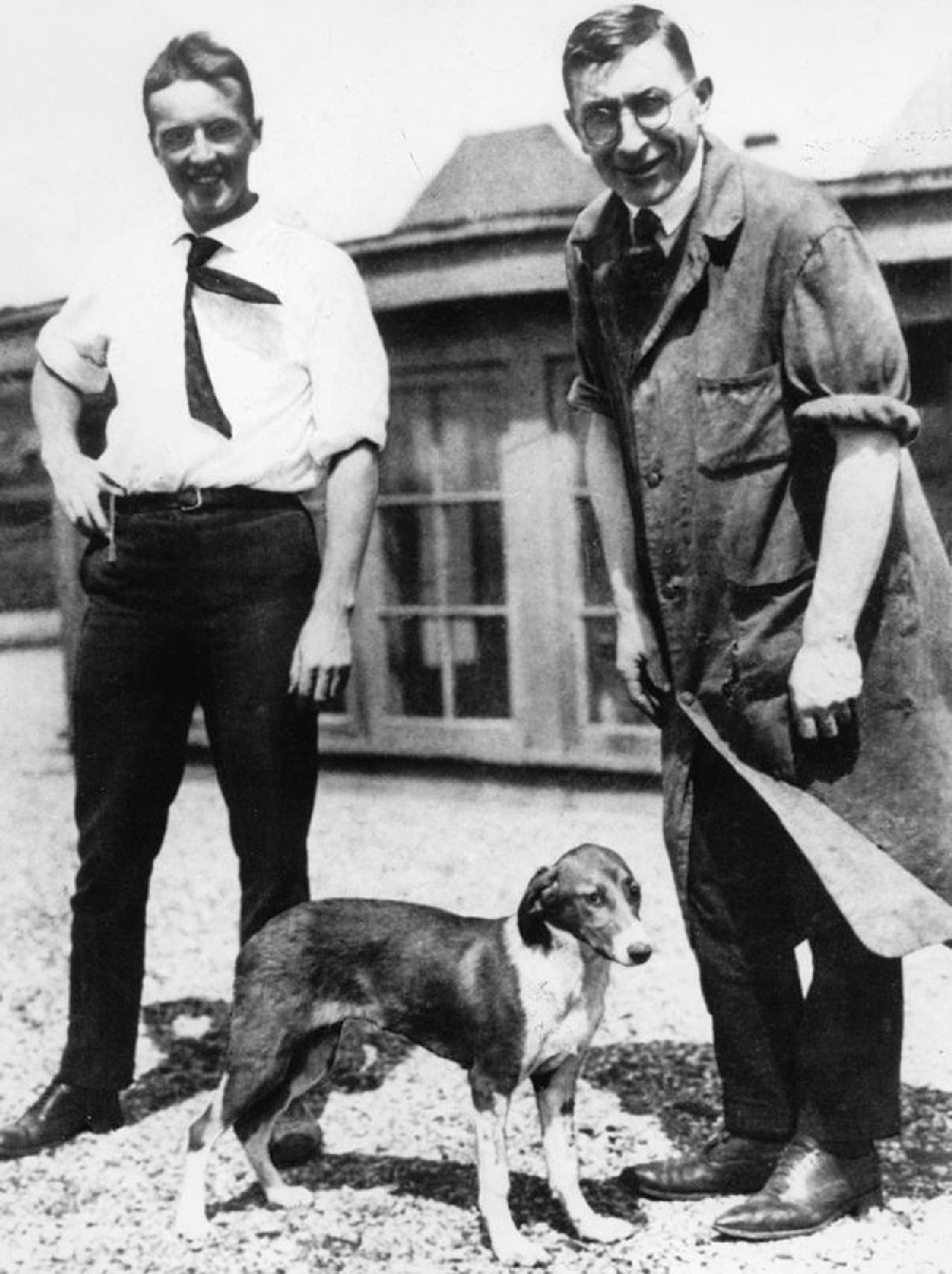
In 1921, Frederick Grant Banting (Alliston, Ontario [Canada], 1891–1941) and Charles Herbert Best (Washington County [Maine, USA], 1899–1978), then a student, ligated the pancreatic ducts in a series of dogs, isolating a hormone that they initially called isletin, but later came to be called insulin (Fig. 1).
In 1923, Banting and John James Rickard MacLeod (Clunie [Scotland], 1876–1935), a professor of physiology in Toronto, received the Nobel Prize in Physiology or Medicine for this discovery. Best, the student who had helped Banting, was ignored. Upset by this, Banting shared the prize money with his young colleague.7,14 Frederick Sanger (Gloucestershire [United Kingdom], 1918–2013), a biochemist who worked at Cambridge University, was one of only 4 people to have been awarded a Nobel prize twice, the others being Marie Curie, Linus Pauling and John Bardeen. He received the first award in 1958 after having identified the amino acid sequence of insulin in 1955. However, human insulin was not synthesised until 1974 by the Swiss P. Sieber.15
John Raymond Murlin (1874–1960), a professor of physiology at the University of Rochester between 1919 and 1945 and co-founder of the American Institute of Nutrition in 1928, researched diabetes, insulin and protein metabolism. In 1923, he discovered, together with Charles P. Kimball, glucagon in an extract of dog duodenal mucosa and pancreas,16 although this discovery has also been attributed to Christian de Duve (Thames-Ditton [United Kingdom), 1917–2013); de Duve was a cytologist and biochemist who won the Nobel prize in Physiology or Medicine in 1974 (which he shared with Albert Claude and George Emil Parade) for having described the structure and functions of the different organelles inside the cells. Nevertheless, it was not until 1956 that William W. Bromer described the sequence of amino acids that form glucagon.17
In 1970, Sani I. Said (Cairo [Egypt], 1928–2013) and Viktor Mutt (Tartu [Estonia], 1923–1998), working at the Karolinska Institute in Stockholm, isolated a polypeptide with vasodilatory properties at splanchnic level from the small intestine of a pig, which they called vasoactive intestinal peptide.18 Two years later, the same authors managed to sequence this hormone,19 which is widely distributed in the body, with high concentrations having been detected in pancreatic tissue. In 1973, it was implicated as the agent that produced the syndrome that Verner and Morrison had described in 1958, and which will be discussed later.
Roger Guillemin (Dijon [France], 1924) was a medical graduate from the University of Lyon, who in 1970 joined the Salk Institute in La Jolla (California, USA). In 1972, he isolated somatostatin, for which he won the 1977 Nobel prize in Physiology or Medicine, shared with Andrew Viktor Schally (Vilna [Poland], 1926), an endocrinologist who had emigrated to Great Britain and then later to the USA, and with Rosalyn Yalow (New York [USA] 1921–2011), a professor in the Department of Medicine at Mount Sinai School. The 3 of them worked on hypothalamic and pituitary hormones, and their quantitation using radioimmunoassay techniques.20 Receptors for this hormone are expressed in 80% of PNET, except in insulinoma, which expresses it in only 50% of cases, thereby aiding its localisation.
In 1975, J.R. Kimmel, working in the Department of Biochemistry and Medicine at the University of Kansas, published an article in which he described the isolation and characterisation of a new pancreatic hormone that he called pancreatic polypeptide. It had previously been identified in the pancreas of other mammals, birds and reptiles.21 The function of pancreatic peptide is to self-regulate the secretory function (endocrine and exocrine), and it has an effect on hepatic glycogen levels and gastrointestinal secretions. Its secretion in humans is increased after the ingestion of protein-rich foods, fasting, exercise and hypoglycaemia, and decreases with the release of somatostatin and intravenous glucose administration.
Other diagnostic developmentsThe different techniques used to diagnose PNET can be divided into: analytical methods, imaging techniques and histopathological studies.
Analytical methodsVarious techniques have been used to detect elevated levels of the different hormones responsible for symptoms caused by functioning tumours, or to help determine type in non-functioning tumours.
Prior to 1960, it was very difficult to determine the plasma concentration of different substances, especially peptide hormones, since they circulate through the organism in very small quantities and are very difficult to distinguish chemically from other plasma proteins that are present in much higher concentrations.
A fundamental step was taken in 1960, when the aforementioned Rosalyn Yalow, together with Salomon Aaron Berson (New York [USA], 1918–1972) (son of a Russian immigrant and consummate violinist and chess player), using their experience in protein labelling, devised a technique to quantitate plasma insulin, which they called radioimmunoassay.22,23 This technique is based on the principle of competitive inhibition according to the law of mass action proposed by Cato Maximillian Gulberg (Oslo [Norway], 1836–1902] and his brother-in-law Peter Petersen Waage (Hydra [Norway], 1833–1900), which states that the rate of a chemical reaction is directly proportional to the concentrations of the reacting substances.
With the development of this method, the plasma concentration of different hormones was gradually determined. Thus, in 1961, Roger H. Unger, working in Dallas Veterans Hospital, quantitated glucagon,24 in 1967 James McGuigan quantitated gastrin,25 and in 1977 J. Fahrenkrug quantitated vasoactive intestinal polypeptide.26
Other techniques used for this purpose include enzyme immunoassay, an immunochemical method based on antigen-antibody reactions that is similar to radioimmunoassay but uses an enzyme instead of a radioactive isotope as a label. It does not use radioactive compounds, which makes it easy to handle (it does not require specific facilities or licenses), is highly sensitive and can be automated (enzyme-linked immunosorbent assay [ELISA] techniques). Fluoroimmunoassay differs from enzyme immunoassay in that it uses a fluorescent molecule as a label. Finally, chemiluminescent immunoassay uses an enzyme to catalyse the oxidation of a substrate to produce an electrical stimulation that emits light energy that can be measured using a luminometer.
Imaging techniquesThe aim of these techniques is to identify and locate the tumour to help the surgeon plan the intervention, the only treatment considered potentially curative, and to determine whether the growth has spread, which can occur in 30–50% of cases.
Mesenteric arteriography and later selective arteriography was one of the first radiological techniques used for the identification and localisation of PNETs, especially in the case of insulinomas. The procedure consists of intra-arterial stimulation with subsequent venous sampling to determine insulin levels.27 The high vascularity of these tumours enabled their diagnosis using this technique. This hypervascularity had already been demonstrated in 1901 by Baltimore pathologist Eugene Lindsay Opie (Staunton [Virginia, USA], 1873–1971) on observing that, when he injected Berlin blue through the arteries, the islets showed a greater number of blood vessels than the surrounding exocrine tissue due to the larger diameter of the capillaries.28 Owing to its aggressiveness, arteriography was gradually replaced by other, less invasive radiological methods.
Grey-scale ultrasound, introduced in 1971, was very useful in identifying some of these tumours, but has low sensitivity given the retroperitoneal location of the pancreas.
In 1974, the first computed tomography scan of the body was obtained, which was a huge breakthrough in the diagnosis and localisation of the different pancreatic diseases, especially PNETs. The administration of intravenous contrast enabled these tumours to be easily diagnosed, due to their characteristic high vascularity.
Magnetic resonance was a technique developed by Isidor Isaac Rabi (Rymanov [Poland], 1898–1988) to measure the magnetic properties of atoms, and for which he was awarded the Nobel prize in Physics in 1944.29 It was later applied to medical imaging, with a sensitivity, in the case of PNETs, similar to computed tomography. However, it is less effective in detecting metastases.
Octreoscan is a technique introduced in 1990 by Dutchman S.W. Lamberts from Dijkzigt hospital in Rotterdam. The technique uses somatostatin analogues conjugated with radioisotopes to obtain a scintographic image, which is useful in diagnosis of both the primary tumour and its metastases.30 The effectiveness of this technique derives from the fact that 80% of PNETs present somatostatin receptors, except for insulinoma, which only presents 50%.
Positron emission tomography (PET) is a 3-dimensional imaging technique based on the detection and analysis of an intravenously administered radiotracer with a very short half-life. It was developed following the theoretical and experimental discovery of the positron, the existence of which was predicted in 1927 by physicist Paul A.M. Dirac (Bristol [Great Britain], 1902–1984), for which he was awarded the Nobel prize in Physics in 1933.31 Subsequent to this discovery, Carl David Anderson (New York [USA], 1905–1991) detected, in 1932, the positron, for which he also received the Nobel prize in Physics in 1936.32 The PET scanner was pioneered in 1975 by biophysicist Michael Phelps (Cleveland [USA], 1939).33 Finally, in 1998, David W. Townsend34 and Ronald Nutt proposed the first PET-CT prototype for clinical evaluation, which was installed in the University of Pittsburg before being widely commercialised in 2002. Better localisation of the lesions can be obtained with this combined technique.
In the field of endoscopy, the first endoscopic ultrasounds were performed in 1976 by H. Lutz and W. Rösch from Ludwig Demling's team in Erlangen.35 However, it was not until 1980 when Eugene DiMagno in the Mayo Clinic and Meinhard Classen in Germany started real-time endoscopic ultrasound, which has improved the diagnosis of different pancreatic diseases, determined tumour extension, and enabled clinicians to perform therapeutic procedures and fine needle aspiration for histopathological study of the samples.36,37Endoscopic ultrasound elastography, developed in the early 2000s, estimates tissue stiffness using specific computer software. It has been shown to be useful for differentiating pancreatic inflammatory processes from carcinoma and PNETs.38
Histopathological evaluationIn 2000, the World Health Organisation proposed a classification system for neuroendocrine tumours, that was later modified in 2010. This latter classification considers 3 tumour grades: G1, benign and of uncertain behaviour; G2, well-differentiated carcinomas; and G3, poorly-differentiated carcinomas. The latter are the most aggressive.39 Most PNET belong to the first 2 groups. They have a low mitotic and proliferative index which is measured by quantitating Ki-67, a nuclear protein that is associated with and necessary for cell proliferation. This marker is present in all active phases of the cell cycle. Various studies have shown that a Ki-67 index of over 5% indicates a more aggressive tumour.40 These tumours also express general neuroendocrine markers such as chromogranin A, synaptophysin, neuron-specific enolase and cytokeratin 19.41 They also generate, as mentioned, certain hormones that define the tumour type.
The tumoursInsulinomaIn 1888, Jean Louis Marius Bard (Mens [France], 1857–1930) and Ferdinand Adrien Pic (1863–1943) published a clinical and histological study in which they hypothesised that pancreatic islet cells could develop cancer.42 Some years later, in 1902, Albert G. Nicholls, a Canadian pathologist, published the first case of an adenoma that had developed from the islet cells, based on an incidental finding during an autopsy.43 The following year, Salvatore Fabozzi published 5 cases of islet cell carcinoma, 4 of which presented metastases.44 In 1914, Kristian Axel Heiberg (Vemmelev [Denmark], 1880–1961), in his book on pancreatic diseases, stated that pancreatic adenomas had no clinical significance,45 and 1 year later, Innsbruck pathologist Franz Josef Lang (Elbigenalp [Austria], 1894–1975) described the case of an asymptomatic patient with nodular hyperplasia of the islets that almost completely replaced the pancreatic exocrine tissue.
In 1922, the aforementioned Banting and Best isolated insulin,14 and in 1924, Seale Harris (Cedartown [Georgia, USA], 1870–1957) was the first to suggest that hypersecretion of this hormone could be responsible for certain cases of spontaneous hypoglycaemia.46 Based on his description, this clinical picture was called Harris syndrome. His hypothesis was confirmed by Russell M. Wilder (Cincinnati [Ohio, USA], 1885–1959) in 1927, when he described the first case of hyperinsulinism associated with insular cell carcinoma with hepatic, lymph node and mesenteric metastases in a 40-year-old surgeon who presented frequent episodes of unconsciousness that were alleviated by the intake of sugar.47 The patient died 1 month after surgery performed by William James Mayo (Le Sueur [Minnesota, USA], 1861–1939), founder of the Mayo Clinic in Rochester together with his brother Charles Horace and 5 other physicians. This intervention was considered the first published case of resection of a PNET. William Mayo died in 1939 from gastric cancer (Fig. 2).
However, the first successful excision of an insulinoma was carried out in Toronto (Canada) on 15th March 1929 by Roscoe Reid Graham (Lobo [Ontario, Canada], 1890–1948). The patient was a 52-year-old woman who had presented repeated episodes of hypoglycaemia with convulsions and coma for 6 years. The intervention consisted of enucleation of a tumour the size of a hazelnut from the pancreatic body. The patient recovered and did not present any further attacks. Histological examination of the tumour demonstrated that it was composed of α and β cells, which are the cells that generate insulin.48
In 1935, Allen Oldfather Whipple (Urmia [Persia], 1885–1963), considered the father of pancreatic surgery, and pathologist Virginia Kneeland Frantz (New York [USA], 1896–1967) published a compilation of 61 insular tumours, only 1 of which presented metastasis.49
The difficulty of locating insulinomas during surgery is known to have plagued surgeons for many years. This problem led James T. Priestley (1903–1979) in 1942 to perform (in the Mayo Clinic) the first total pancreatectomy for hyperinsulinism, when he was unable to locate the tumour during the laparotomy in a 49-year-old woman. The patient survived for 5 years.50
Although surgery is considered to be the curative treatment for PNET, in 1943 Scotsman J. Shaw Dunn raised the possibility of medical treatment of insulinomas using alloxan, after having tested it in an experimental model of diabetes in rabbits. This agent acts selectively on the β cells of the pancreatic islets.51 Years later, in 1964, Sheldon Joseph Bleicher (Dedham [Massachusetts, USA], 1931–2012) applied diazoxide for the treatment of metastatic insulinoma.
GastrinomaIn 1955, Robert Milton Zollinger (Millersport [Ohio, USA], 1903–1992), a surgeon and editor of the American Journal of Surgery from 1958 to 1986, and Edwin Homer Ellison (Dayton [Ohio, USA], 1918–1970)52 described 2 cases of young women with jejunal ulcers associated with a non-β cell tumour of the pancreatic islets.53 One year after publication of the article, Ben Eiseman (St. Louis [Missouri, USA], 1917–2012) proposed calling this clinical picture Zollinger-Ellison syndrome.54 However, some authors prefer the stricter denomination of Strøm-Zollinger-Ellison syndrome, since it was Roar Strøm (Oslo [Norway], 1903–1958) who, in 1952, published the first description.7,55
In 1964, Roderick Alfred Gregory, a professor of physiology at the University of Liverpool, and his co-worker Hilda J. Tracy defined the chemical structure of gastrin, and discovered that it was produced in excess in the tumours of patients with this syndrome.11,12 The subsequent development of the radioimmunoassay technique, devised by Yallow and Berson in 1960 and applied to the quantitation of gastrin in 1967 by James E. McGuigan,25 facilitated the rapid diagnosis of a significant number of cases of this disease.
For many years, treatment of this PNET was total gastrectomy, until the introduction of H2 receptor antagonists in 1978. This molecule, called cimetidine, was developed by pharmacologist James Whyte Black (Uddington [Scotland, Great Britain], 1924–2010), who also discovered propranolol, which was first marketed in 1964. These achievements earned him the 1988 Nobel Prize in Physiology or Medicine.56
GlucagonomaThis is one of the least common PNETs, since it affects only 1 in every 206 individuals. The tumour was first reported in 1942 by S.W. Becker, a dermatologist at the University of Chicago, who described a patient with a malignant pancreatic tumour with a migratory skin rash, glossitis, stomatitis, diabetes, anaemia, weight loss, depression and venous thrombosis.57 The next publication of a similar case did not appear until 1960, reported by pathologist Wolfgang Gössner (Leipzig [Germany], 1919–2004) and dermatologist Günter Waldemar Korting (Mainz [Germany], 1919–1994)58,59 of the University of Tübingen (Baden-Wurtemberg), one of the oldest universities in Germany, founded in 1477. However, some years previously, in 1956, Russian physician V.C. Zhadanov60 had published a case report that was not recognised as glucagonoma until the 1970s. Neverthess, it was M.H. McGravan, a pathologist at Washington University School of Medicine (St. Louis [USA]) who related the process with excess secretion of glucagon by the pancreatic α cells in 1966.61 Seven years later, in 1973, Darrell S. Wilkinson, who was president of the British Association of Dermatologists (BAD) between 1979 and 1980, coined the term “necrolytic migratory erythema” to define the skin rash associated with this process.62
The number of cases worldwide was revealed by the aforementioned Association, which in 1974 had identified 9 similar cases and defined the characteristics of glucagonoma syndrome in an article authored by C.N. Mallinson et al.63
VipomaVipoma is another very rare PNET that only affects 1 in every 106 individuals.64 In 1958, American internist John Victor Verner (Greenville [North Carolina, USA], 1927) and an American pathologist of Irish origin, Ashton Byrom Morrison (1922), described a syndrome that carries their name, characterised by watery diarrhoea, hypokalaemia and achlorhydria,65 even though 1 year earlier, British physicians W.M. Priest and M.K. Alexander had described a similar syndrome.66 This clinical picture received several names since its first description, such as pancreatic cholera,67 WDHA syndrome (from Watery Diarrhoea, Hypokalemia, Achlorhydria) or watery diarrhoea syndrome,68 until in 1973, Stephen Robert Bloom (Maidstone [Great Britain], 1942) and Julia Margaret Polak (Buenos Aires [Argentina], 1939–2014) named it vipoma,69 after identifying vasoactive intestinal peptide as the causal agent of the syndrome, the hormone originally discovered by Sani I. Said and Viktor Mutt in 1970. Bloom and Polak worked in Hammersmith Hospital, London. In 1995, Dr. Polak had to undergo a heart and lung transplant after she developed idiopathic pulmonary arterial hypertension; from then on, she changed her field of interest from pathology to tissue engineering.
Treatment of this syndrome initially consisted only of correcting the dehydration caused by the copious diarrhoea, but streptozotocin was later used due to its cytotoxic action,70 followed subsequently by the administration of octreotide, a somatostatin analogue synthesised in 1979 by Swiss chemist Wilfried Bauer,71 due to its blocking effect on vasoactive intestinal peptide. However, surgery is the only curative treatment if the tumour is localised.
SomatostatinomaThis is an even rarer PNET than those mentioned above, as it affects only 1 in every 406 individuals.72 The first description of this type of tumour was published in 1977 by an American endocrinologist of Indian origin, Om P. Ganda73 of the Joslin Diabetes Centre in Boston. It originates in the δ cells of the pancreas and inhibits the pancreatic and gastrointestinal hormones, therefore manifesting with diabetes (inhibition of insulin), achlorhydria (gastrin), gallstones (cholecystokinin) and steatorrhoea (secretin and cholecystokinin). The treatment of choice is surgery when possible. When there is metastatic disease, streptozotocin, alone or in combination with 5-fluoracyl,74 doxorubicin and adriamycin75 is used. Support treatment must be given with insulin and oral pancreatic enzyme supplements that improve the steatorrhoea and the nutritional status.
PpomaThis is also a very rare PNET, with only 21 cases having been described until 1990.76 It is characterised by watery diarrhoea, hypokalaemia and achlorhydria, as in Verner-Morrison syndrome, but with normal vasoactive intestinal peptide values. However, pancreatic polypeptide levels are abnormally high. The first case of this type of tumour was described in 1976 by biochemist Lars-Inge Larsson of the University of Aarhus in Denmark.77
Multiple endocrine neoplasmsIn 1954, Paul Wermer (1898–1975), who worked in the Presbyterian Hospital in New York, observed that a certain percentage of pancreatic islet cell tumours formed part of multiple endocrine adenomatoses.78 Thus, pancreatic tumours could co-exist with pituitary and parathyroid gland tumours, and also presented autosomal dominant inheritance with complete penetrance. In 1968, A.L. Steiner79 introduced the term “multiple endocrine neoplasia” to describe these tumours, and differentiated type I or Wermer syndrome from type II or Sipple syndrome (neoplasms that affect various endocrine glands, except the pancreas) described by this author in 1961.80 One year after acceptance of the term multiple endocrine neoplasia, A.G. Everson Pearse (Birchintong [Kent, Great Britain], 1916–2003) proposed grouping all these lesions that presented common biochemical characteristics under the acronym “Apudoma”.81 Finally, in 1998, Sirandanahalli C. Guru cloned the gene for multiple endocrine neoplasia I in the National Institutes of Health in Bethesda (USA).82
Conflict of interestsThe authors declare that they have no conflict of interests.