We read with great interest the article by Martín-Lagos Maldonado A et al.1 describing pelvic inflammatory disease as an uncommon cause of bowel obstruction due to adhesions. We would like to report another uncommon case of bowel obstruction due to adhesions, in this case due to adhesions of idiopathic origin.
Intra-abdominal adhesions may be congenital or acquired.2 In cases in which no cause can be identified, they are considered to be of idiopathic origin.3 Given that idiopathic adhesions are uncommon since the adhesion cause is generally diagnosed, we report the case of a patient with intestinal subocclusion due to idiopathic adhesions.
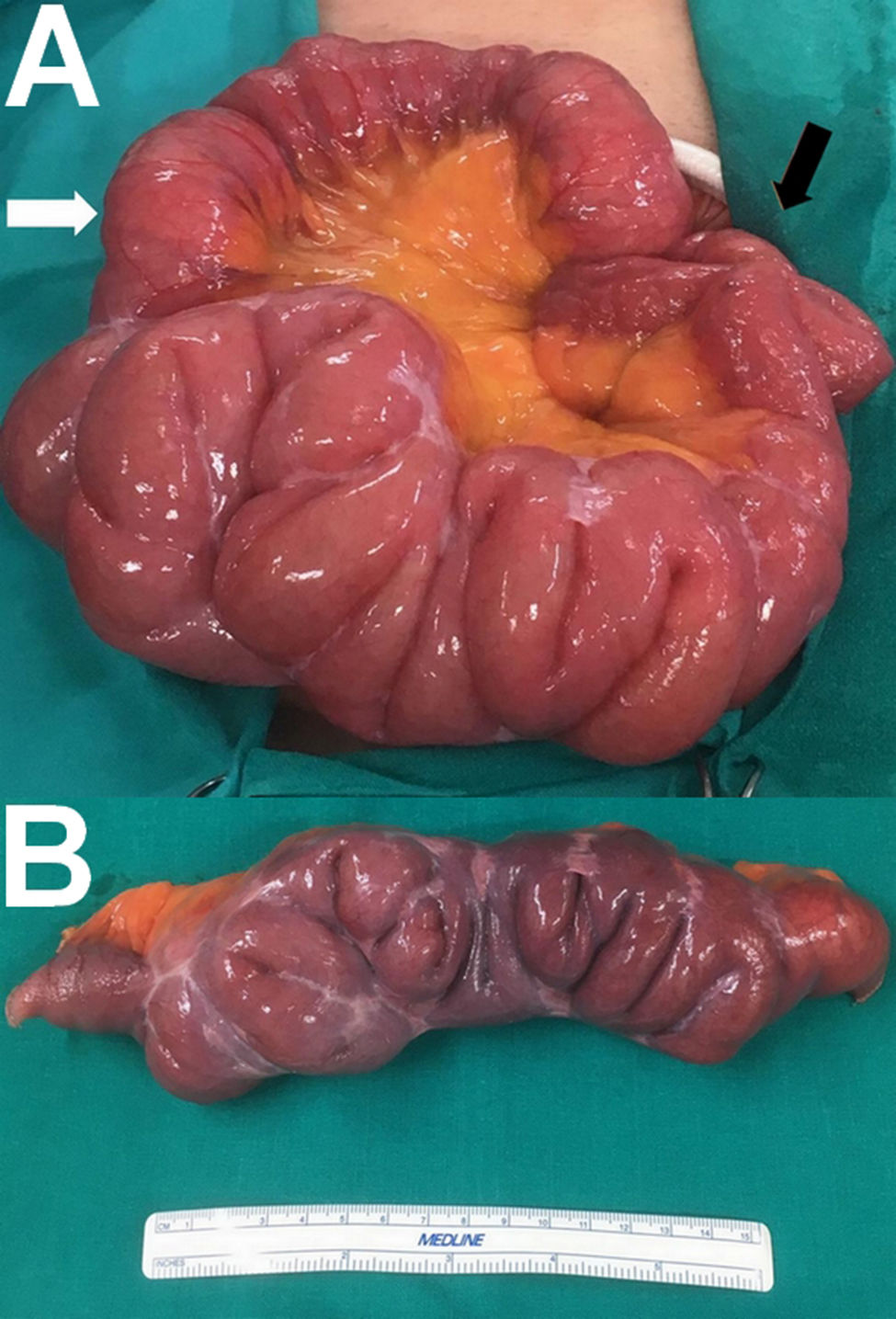
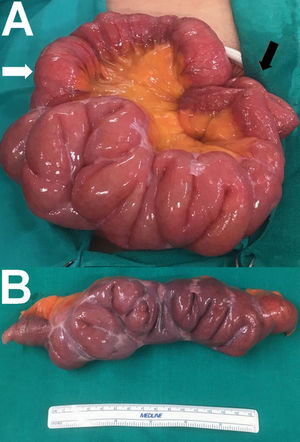
A 65-year-old man with no history of abdominal surgery visited the emergency department due to abdominal pain. He did have a history of scoliosis. The patient reported diffuse abdominal pain and vomiting lasting 24 h, with difficulty breaking wind and defecating. It was the third episode in the past year. On examination, he presented a distended abdomen with diffuse pain and no signs of peritoneal irritation. Laboratory testing revealed a leukocyte count of 17,600 and a C-reactive protein (CRP) level of 6.7 mg/dl. An abdominal X-ray and a computed tomography scan showed air-fluid levels in the small intestine, but did not show the cause of the patient’s signs and symptoms of subocclusion. After clinical improvement was not achieved with conservative treatment, an exploratory laparotomy was performed. This yielded the sole finding of multiple firm adhesions in a segment of middle jejunum measuring 50−60 cm, resulting in several bends interfering with bowel transit (Fig. 1A). The rest of the abdominal cavity was normal. A bowel resection including the affected bowel loop (Fig. 1B) and a mechanical laterolateral isoperistaltic anastomosis were performed. The histopathology analysis showed only fibrous adhesions and ruled out other underlying causes. After a year of follow-up, the patient was asymptomatic.
A. Segment of middle jejunum measuring 50-60 cm with multiple firm adhesions resulting in several bends interfering with bowel transit. The afferent loop (white arrow) and the efferent loop (black arrow) are visible. B. Bowel resection specimen from the affected segment showing multiple fibrous adhesions resulting in several bends.
Postoperative acquired intra-abdominal adhesions are the most common type of adhesion (accounting for 90% of all adhesions).4 They form in 50%-100% of patients who undergo abdominal and pelvic surgery,2 especially in those having undergone a laparotomy.4 Fortunately, the incidence of adhesions has decreased considerably in the era of laparoscopic surgery.4
In the absence of prior abdominal surgery, acquired adhesions may be due to inflammatory causes, infectious causes or radiotherapy sequelae. Notable inflammatory–infectious aetiologies reported include endometriosis and pelvic inflammatory disease in women,1,4 diverticular disease (especially of the small intestine), Crohn’s disease, and abdominal tuberculosis in endemic areas. Abdominal and pelvic radiotherapy in the treatment of gynaecological, prostatic, rectal and lymphoproliferative neoplasms may also cause adhesions. Their severity depends on the extent of the treated area, the degree of fractionation of the dose, and the total dose of radiation.4 In addition, post-inflammatory adhesions have been detected on autopsy in up to 28% of cases of patients with no history of abdominal surgery.2 In the case reported, a colonoscopy and a gastroscopy were performed to rule out inflammatory bowel disease. A tuberculin test was also done to rule out prior exposure to the tuberculosis bacillus. The results were negative. All other causes were ruled out given the patient’s sex and personal history and the histopathology examination of the resected bowel.
Congenital adhesions form during embryonic development,2 and are an extremely uncommon cause of bowel obstruction in adults.5 They are most often located between the terminal ileum or its mesentery and the ascending colon, ligament of Treitz, right liver lobe or bladder. In most cases, they consist of connective tissue containing vessels and nerves.5 In the case reported, a congenital aetiology was ruled out in light of the patient’s age and because he had multiple adhesions that contained neither blood vessels nor nerves and were not located in the typical locations described above.
With all acquired and congenital aetiologies having been ruled out, the patient’s adhesions were deemed to be of idiopathic origin. In conclusion, idiopathic adhesions should be borne in mind in the differential diagnosis of bowel obstruction in patients with no prior abdominal surgery, especially where radiological testing does not show any responsible lesion.
Conflicts of interestWe declare that there are no matters in relation to funding or of any other nature that might create any conflict of interest.
Please cite this article as: Ruiz Pardo J, García Marín A, Ruescas García FJ, Valiente Carrillo J. Suboclusión intestinal secundaria a adherencias idiopáticas en paciente sin cirugía intraabdominal previa. Gastroenterol Hepatol. 2020;43:481–482.