Current trend in the treatment of non-complicated diverticulitis is the outpatient management with antibiotic or even anti-inflammatory regimens in selected cases. We present a comparison of the results in our hospital with different protocols applied in 2016 and 2017.
Material and methodsAll patients selected for this study were diagnosed with diverticulitis grade Ia of Hinchey's classification according to radiological findings on abdominal CT. We have analyzed two retrospective cohorts: 100 patients treated in 2016 according to the old protocol and 104 patients treated in 2017 with a new protocol. In 2016, the candidates for ambulatory treatment remained under observation for 24 h before being discharged. The treatment consisted of 14 days of ciprofloxacin and metronidazole. In 2017, only patients with more acute symptoms were observed 24 h and amoxicillin-clavulanic acid was prescribed for only 5 days.
ResultsThe persistence of the disease in 2016 was 6% and in 2017 was only 5.77% (P = .944). Recurrence during the first year was 13% in the first group, while in the second it was 5.7%, although this difference was not statistically significant. Likewise, a significant reduction in health costs was achieved.
ConclusionsOutpatient treatment of acute uncomplicated diverticulitis with oral treatment seems to be a safe and effective therapeutic strategy in selected patients with low comorbidity.
La tendencia actual en el tratamiento de la diverticulitis aguda no complicada es el manejo ambulatorio de los pacientes con pautas cortas de antibiótico o incluso con antiinflamatorios en casos seleccionados. Presentamos una comparativa de los resultados obtenidos en nuestro hospital con distintos protocolos aplicados en 2016 y 2017.
Material y métodosTodos los pacientes seleccionados para este estudio fueron diagnosticados de diverticulitis grado Ia de la clasificación de Hinchey según los hallazgos radiológicos en la TC abdominal. Hemos analizado dos cohortes retrospectivas: 100 pacientes tratados en 2016 según protocolo antiguo y 104 pacientes tratados en 2017 con protocolo nuevo. En el año 2016 los pacientes candidatos a tratamiento ambulatorio permanecieron en observación durante 24 horas antes de ser dados de alta. El tratamiento consistió en 14 días de ciprofloxacino y metronidazol, En 2017 solo se observaron 24 horas los pacientes con sintomatología más aguda y se prescribió amoxicilina-clavulánico durante sólo 5 días.
ResultadosLa persistencia de la enfermedad en 2016 fue del 6% y en 2017 sólo alcanzó el 5,77% (P = .944). La recidiva durante el primer año fue del 13% en el primer grupo, mientras que en el segundo fue un 5,7%, si bien esta diferencia no fue estadísticamente significativa. Así mismo se consiguió una significativa reducción del coste sanitario.
ConclusionesEl tratamiento ambulatorio de la diverticulitis aguda no complicada con pauta corta de antibiótico oral parece ser una estrategia terapéutica segura y efectiva en pacientes seleccionados con escasa comorbilidad.
Traditional treatment of uncomplicated acute diverticulitis has been based on hospitalising the patient for IV administration of antibiotics and serum therapy until clinical and laboratory improvement is achieved.1–3
At present, there are sufficient sources in the literature supporting the use of outpatient antibiotic treatment in mild or uncomplicated acute diverticulitis.4–10 Despite this evidence, in Spain, according to existing publications, outpatient treatment seems to be in limited use.
Some recent studies have gone a step further and affirmed that this is an inflammatory disease and not an infectious one, as postulated by classic theories.11,12 However, evidence for incorporating an exclusively anti-inflammatory treatment into clinical practice guidelines remains insufficient.
At our centre, treatment for uncomplicated acute diverticulitis did not require hospital admission in all patients until 2010; in that year, the first change was made based on published studies having demonstrated the efficacy and safety of outpatient treatment, and stricter admission criteria were established. Given the gradual trend towards decreasing the use of oral antibiotics for this disease, in 2017, we decided to shorten the length of stay in the emergency department and reduce the days of administration of oral antibiotics.
This study had two objectives: first, to demonstrate the effectiveness of a shorter antibiotic regimen, this being equally safe for the patient; and second, to measure the impact of this change on reduction of healthcare costs.
Material and methodsWe conducted a retrospective study of two cohorts of patients: those who received care in 2016 under the old protocol, and those who received care in 2017 under the new one.
All patients diagnosed with uncomplicated acute diverticulitis (stage Ia according to Hinchey’s classification) were enrolled in this study. The diagnosis was made through a medical history, physical examination, blood testing and findings on an abdominal CT scan. Cases with colon wall thickening (>4 mm), trabeculation of pericolic fat and/or isolated gas bubbles against the colon wall (thus not free pneumoperitoneum) were considered to be cases of mild acute diverticulitis.
The group of 100 patients who received care in 2016 followed the protocol described below:
- -
Direct hospitalisation in case of patients with a history of insulin-dependent diabetes mellitus, cirrhosis, kidney failure and immunosuppression (corticosteroid treatment, chemotherapy, HIV, etc.). Age and prior episodes of diverticulitis were not considered as criteria for admission. These patients were treated with intravenous ertapenem 1 g/24 h for seven days.
- -
By contrast, patients who did not meet these criteria stayed in the emergency department for 24 h on intravenous treatment (ciprofloxacin and metronidazole) and were discharged with outpatient treatment if they exhibited clinical and laboratory improvement. Oral antibiotic treatment was maintained for 14 days, using ciprofloxacin 500 mg/12 h and metronidazole 500 mg/8 h along with oral analgesia (paracetamol 1 g/8 h). Finally, patients were scheduled for an appointment in the emergency department for assessment by surgery, with clinical and laboratory monitoring on days 4 and 14 of treatment.
The cohort of 104 patients who received care in 2017 received short-term antibiotic treatment as set out in the new protocol:
- -
Same admission criteria as the previous group. Patients who were admitted received oral ceftriaxone 1 g/24 h and intravenous metronidazole 500 mg/8 h, for approximately 48−72 hours, until clinical and laboratory improvement were confirmed. Following discharge, patients completed the seven days of antibiotic treatment with oral amoxicillin/clavulanic acid 875−125 mg/8 h. The majority of these patients followed a favourable clinical course, as in 2016; however, follow-up of admitted patients was not an objective of this study.
- -
Patients without admission criteria were discharged with amoxicillin/clavulanic acid 875−125 mg/8 h for five days (using oral ciprofloxacin and metronidazole for five days in just two patients who were allergic to beta-lactam antibiotics), with monitoring in the emergency department by surgery on the last day of treatment. Observation in the emergency department for 24 h was reserved solely for patients with more acute symptoms, with poor management of pain, fever or vomiting. During this period, patients who did not report clinical and/or laboratory improvement were administered intravenous antibiotic treatment (amoxicillin/clavulanic acid) and admitted.
In all cases (both protocols), patients were referred for outpatient care from the Colorectal Surgery Unit and a colonoscopy was ordered for one to three months after the episode to confirm the diagnosis and rule out the presence of other lesions.
Similarly, all cases of persistence in the first 30 days following completion of treatment were admitted with intravenous piperacillin/tazobactam. If they had a recurrence after the first month, patients followed the protocol corresponding to the year of the first episode.
The primary endpoints in this study to assess the effectiveness and safety of the new treatment were disease persistence, which, according to the literature, was not to exceed 7%, and recurrence, which was to be less than 15%.
Statistical analysisMeans for independent samples were compared using Student’s t test, and proportions were compared using the χ2 test. A P value less than .05 was considered statistically significant. Data analysis was performed using the Stata statistics software program, ver. 15.1, and comparative analysis was done by intention to treat.
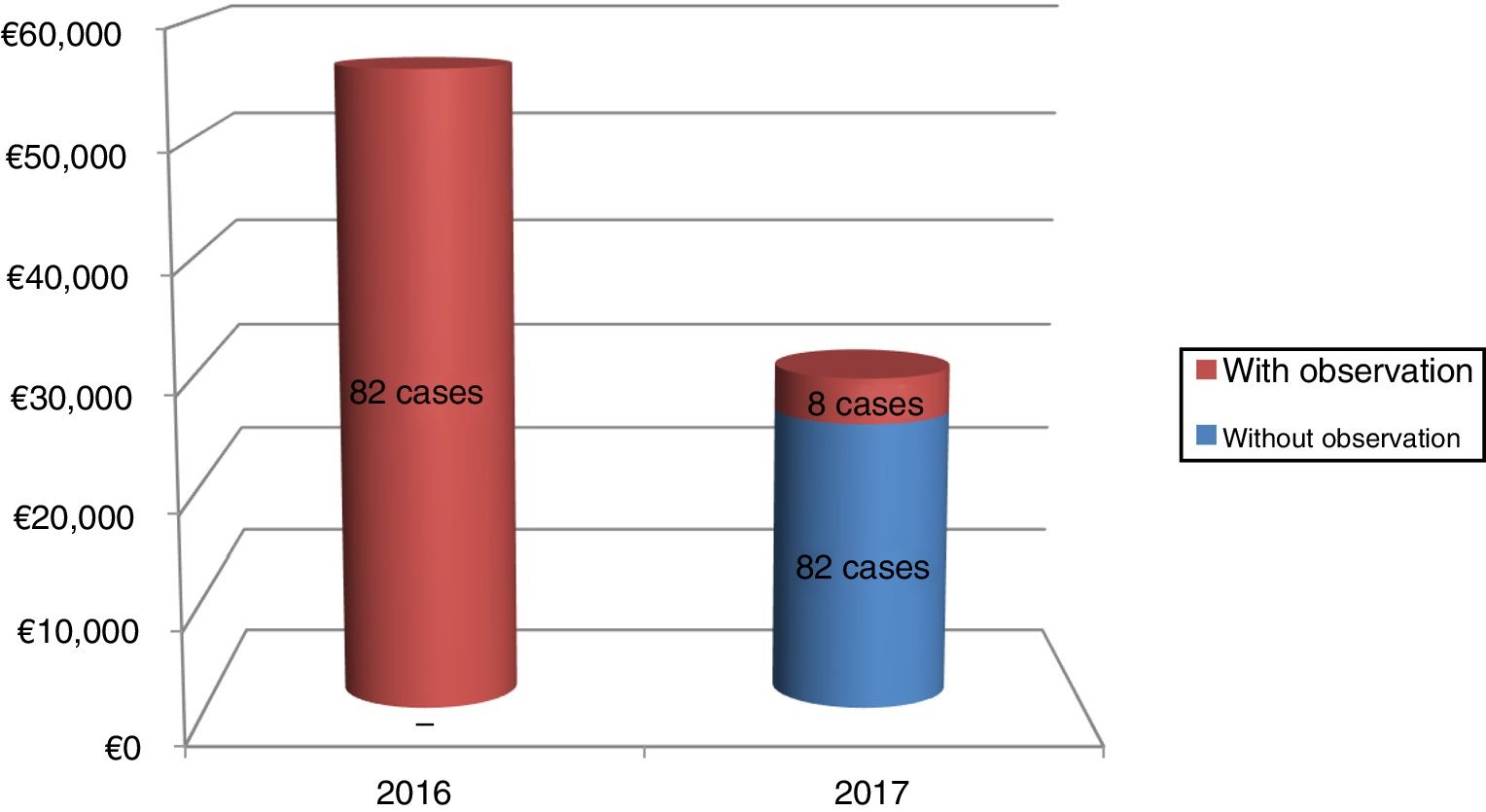
To study costs the diagnosis-related group (DRG) classification system was used, and partial and overall healthcare costs according to each protocol were estimated.
ResultsIn accordance with the criteria set out, 100 patients were diagnosed with uncomplicated acute diverticulitis in 2016, and 104 patients were diagnosed with this disease in 2017. Of these, 82 in the former group of patients and 90 in the latter met the criteria for outpatient treatment. Reasons for hospital admission were those established for each protocol. In some subsidiary cases of outpatient treatment (five patients in 2016 and two patients in 2017), persistent signs and symptoms and laboratory abnormalities following 24 h of observation prompted the surgeon on duty to decide to admit the patient.
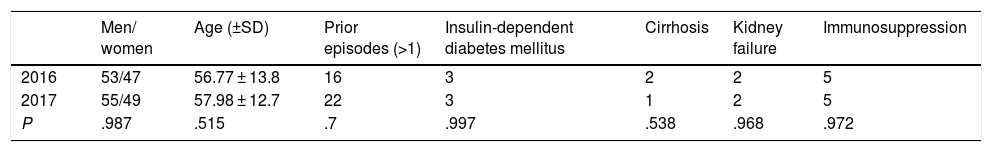
Table 1 summarises the patients’ clinical characteristics. We found no statistically significant differences in age, sex, comorbidities or number of prior episodes of diverticulitis.
Just one case in 2016, and two cases in 2017, involved impairment of the right colon, but followed a favourable clinical course with application of the corresponding protocol.
In the first 30 days after diagnosis, six patients (6%) in 2016 and six patients (5.7%) in 2017 returned to the emergency department owing to persistent symptoms, abdominal pain being the most common. This difference was not statistically significant (P = .94). All these cases were resolved with intravenous treatment during readmission and none required emergency surgery.
Mean duration of follow-up for each cohort was 12 months. During this time, rates of recurrence were 13 cases (13%) in the 2016 group and six cases (5.7%) in the 2017 group, without this difference attaining statistical significance (P = .076).
From an economic point of view, overall healthcare costs were significantly lower in the 2017 cohort compared to the 2016 cohort, with a year-on-year reduction of є26,482.50 (47.2%), as Fig. 1 shows. This calculation accounted for only those patients who were treated on an outpatient basis in each year (82% in 2016 and 86.54% in 2017); observation for 24 h in the emergency department was the most important factor for cost reduction between the two protocols (all 2016 patients required this observation, but it was only necessary in 8.9% of 2017 cases). Cost reduction due to shorter duration of antibiotic treatment also contributed to the results (є6.56 per patient comparing oral presentations).
DiscussionDiverticulosis is a common disease within ageing populations in industrialised Western countries. Its prevalence increases with age and can be as high as 60%–80% in the population 80 years of age and older. Most patients remain clinically asymptomatic throughout their lives; however, a variable percentage of them (9%–25%) experience acute diverticulitis.13 Nevertheless, a recent prospective study found that this long-term risk is lower (around 4%).14 In most cases, diverticulitis presents no complications and is self-limiting, whereas in 15%–20% of cases it is reported as a "complicated" presentation with an abscess, perforation, fistula, obstruction, peritonitis or sepsis. In addition, one-third of these patients will experience a recurrence after the first acute episode in the following five years and up to 10% will require emergency surgery.15
The growing prevalence of diverticular disease has brought about a gradual increase in the corresponding healthcare burden and healthcare costs in Spain in recent years. It represents the fifth most significant gastrointestinal disease in terms of medical care costs both in the United States and in Europe.16 The United States reports more than 200,000 hospitalisations per year and annual costs exceeding two billion dollars.17
At present, patients with uncomplicated acute diverticulitis are usually managed on an outpatient basis. A study by Martin Gil et al.18 compiled a total of 74 patients with a diagnosis of Hinchey stage I or stage II diverticulitis with an abscess measuring less than 3 cm (though this subgroup comprised just 3% of the total) who were treated with oral ciprofloxacin and metronidazole for 7–10 days with satisfactory outcomes.
Lorente et al.19 conducted a retrospective study comparing a group of 90 patients who received outpatient treatment with amoxicillin/clavulanic acid for seven days to another group of 46 hospitalised patients and found no significant differences in outcomes. They also included a detailed economic study which found a reduction by up to 60% in healthcare spending with the adoption of the new protocol.
Another option in patients with comorbidity is home hospitalisation with intravenous administration of antibiotics, which has achieved good clinical outcomes and a high degree of patient satisfaction.20
Recently a randomised clinical trial recruited 528 patients from 22 Dutch centres and divided them into two groups: anti-inflammatory treatment, and antibiotic treatment with amoxicillin/clavulanic acid for 10 days. The results showed no significant differences in terms of rates of recovery from, complications in, or recurrence of the disease.21
Although the current literature seems to focus on treating mild acute diverticulitis without antibiotics, the classic regimen for intravenous treatment with hospitalisation remains a reality in some hospitals in Spain. Given that our centre has had experience in outpatient treatment with demonstrated efficacy, we decided to take things a step further and shorten the hospital surveillance and treatment period. Patients who had also been treated with the prior protocol were found to be satisfied with the reduced number of antibiotics and duration of treatment. The results obtained shown that this is an effective and safe regimen for patients and yields a significant reduction in healthcare costs.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: González Plo D, Plá Sánchez P, León Gámez CL, Remirez Arriaga X, Rial Justo X, Artés Caselles M, et al. Actualización del manejo de la diverticulitis aguda no complicada en nuestro centro. Igualmente efectivo, más eficiente. Gastroenterol Hepatol. 2020;43:426–430.