We present the case of a 40-year-old man with a history of depressive disorder who was admitted due to melaena for the past two weeks. He also reported constipation and diffuse abdominal pain, for which he was on treatment with a laxative and nonsteroidal anti-inflammatory drugs (NSAIDs) — up to 1500 mg of naproxen and 1725 mg of metamizole per day. At the same time, he was on treatment with selective serotonin reuptake inhibitors (SSRIs) — 400 mg of desvenlafaxine and 60 mg of duloxetine per day — for his underlying condition.
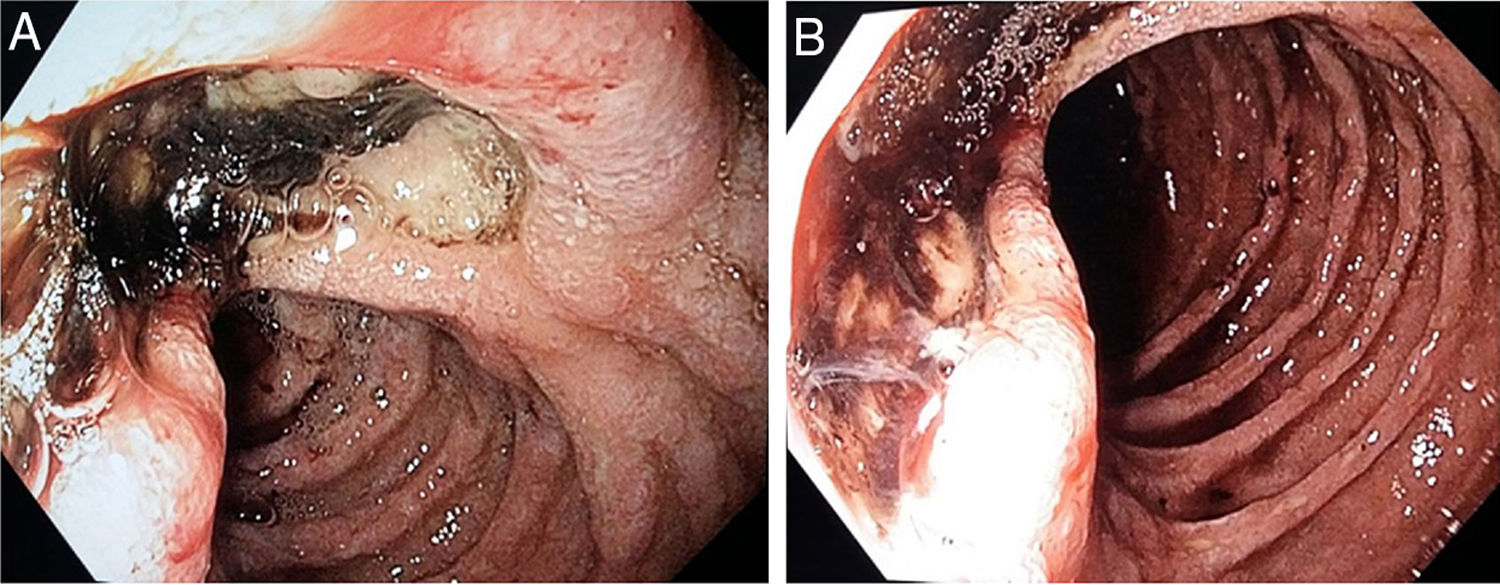
In the emergency department, he had a BP of 120/60, an HR of 120 bpm and skin pallor, and the presence of melaena was observed on digital rectal examination. Laboratory testing yielded the following values: haemoglobin 6.2 g/dl, MCV 85.7 (haemoglobin 14.6 g/dl and MCV 87.5 a week earlier). An emergency gastroscopy revealed multiple ulcerations, most notably a large, deep ulcer covered in fibrin and a black adherent clot (Forrest IIb) in the distal duodenum, half of the circumference of which had an infiltrative appearance (Fig. 1A and B). Biopsies were taken.
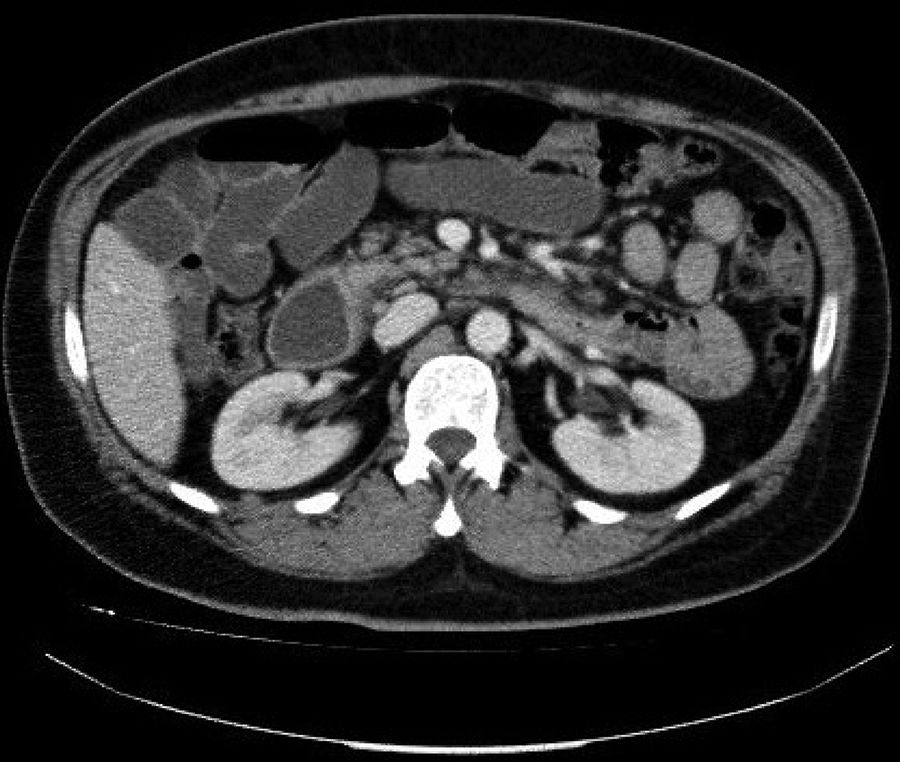
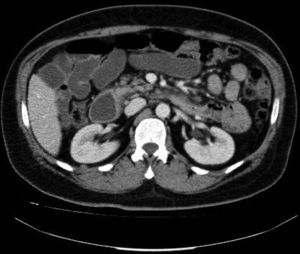
During his admission, the patient also underwent a thoracoabdominal CT scan, which confirmed wall thickening in the distal duodenum and proximal jejunum spanning 7−8 cm, infiltration of adjacent fat and localised lymphadenopathy spanning up to 20 mm. These findings were consistent with a tumour-infiltrating process and suggestive of lymphoma (Fig. 2). However, pathology found no signs of malignancy. The patient was discharged with proton pump inhibitors (PPIs) and instructed not to take NSAIDs pending an enteroscopy.
After a few days, the patient was re-admitted due to severe gastrointestinal bleeding (GIB) in the form of melaena. The patient reported that he was continuing to take metamizole and SSRIs daily. Gastroscopy revealed the persistence of multiple ulcers, including a deep Forrest III ulcer in the distal duodenum with irregular, hard borders on biopsy. Given the seriousness and persistence of the lesions, the patient was assessed by the general surgery department and a decision was made to take a wait-and-see approach in the absence of pathological evidence of malignancy.
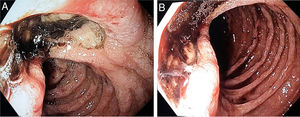
A single-balloon enteroscopy revealed remnants of retained food probably due to stenosis. The procedure was repeated following a three-day fast and confirmed the previously reported ulcers in the distal duodenum causing stenosis through which the endoscope could pass. Biopsies were again taken. The pathology results for all biopsies ruled out malignancy.
Finally, given the suspicion of GIB secondary to a combination of NSAIDs and SSRIs, following an assessment by a psychiatrist, the patient’s antidepressant medication was gradually suspended and the use of any type of NSAID was contraindicated. The patient was prescribed 40 mg of esomeprazole per day. After three months, the patient was found to be asymptomatic, with haemoglobin 16.1 g/dl and MCV 86.9. A follow-up gastroscopy corroborated the disappearance of the lesions, and the patient was not subjected to radiological follow-up given his obvious clinical and endoscopic improvement.
SSRIs are among the most commonly used drugs in psychiatry. They are used to treat depressive disorders, anxiety-related disorders and other disorders. Compared to other generations of antidepressant drugs, they possess a more favourable safety profile,1 although adverse effects in relation to changes in haemostasis have been reported.
Serotonin is an essential component in platelet activity as it enhances platelet aggregation and fibrin formation. SSRIs block reuptake of serotonin, thereby decreasing platelet content and altering platelet function.2 In addition, some of them inhibit some cytochrome P450 isoenzymes and thus increase plasma levels of certain NSAIDs; increased secretion of gastric acid following SSRI intake has even been reported.3
Several systematic reviews have found a slight increase in the risk of GIB with these drugs, accentuated by taking NSAIDs.4–6 Some data also indicate that their use does not increase the risk of rebleeding such that prevention of rebleeding with PPIs is not a cost-effective strategy.7
Our patient was taking two SSRIs at high doses as well as an NSAID without an associated PPI. At present, the Agencia Española del Medicamento y Productos Sanitarios [Spanish Agency of Medicines and Medical Devices] (AEMPS) recommends not exceeding doses of 200 mg of desvenlafaxine per day and 120 mg of duloxetine per day, pointing to an increased risk of bleeding if these drugs are administered with NSAIDs.8,9
At present, no prospective studies have been conducted on their actual involvement in GIB, and no data support the use of PPIs in this case. However, they should be considered to be an added risk factor for frequent users of NSAIDs, and tricyclic antidepressants or monoamine oxidase inhibitors should be weighed up as alternatives in these patients.10
Please cite this article as: Sanz Segura P, García Cámara P, Gotor Delso J, Monzón Báez RM, Llorente Barrio M, Fernández Bonilla E, et al. Hemorragia digestiva alta secundaria a sobreingesta de inhibidores selectivos de la recaptación de serotonina y antiinflamatorios no esteroideos. Gastroenterol Hepatol. 2019;42:622–623.