In 1958, Leslie Zieve described a series of 20 patients who presented with acute hyperlipidaemia, jaundice and haemolytic anaemia, all resolving spontaneously on cessation of alcohol consumption. These patients shared the common context of alcoholic liver disease. This condition is now known as Zieve's syndrome. The syndrome is rare, but probably underdiagnosed.
We present the case of a 51-year-old male with no relevant previous medical history but average consumption of 50g of alcohol a day. He went to Accident and Emergency with generalised malaise and asthenia, and diffuse abdominal pain. He also had signs of mucocutaneous jaundice and choluria. He denied recent consumption of drugs, toxins or herbal products. On examination, he had pain on palpation in the right hypochondrium, with hepatomegaly. The patient was admitted with suspected alcoholic hepatitis.
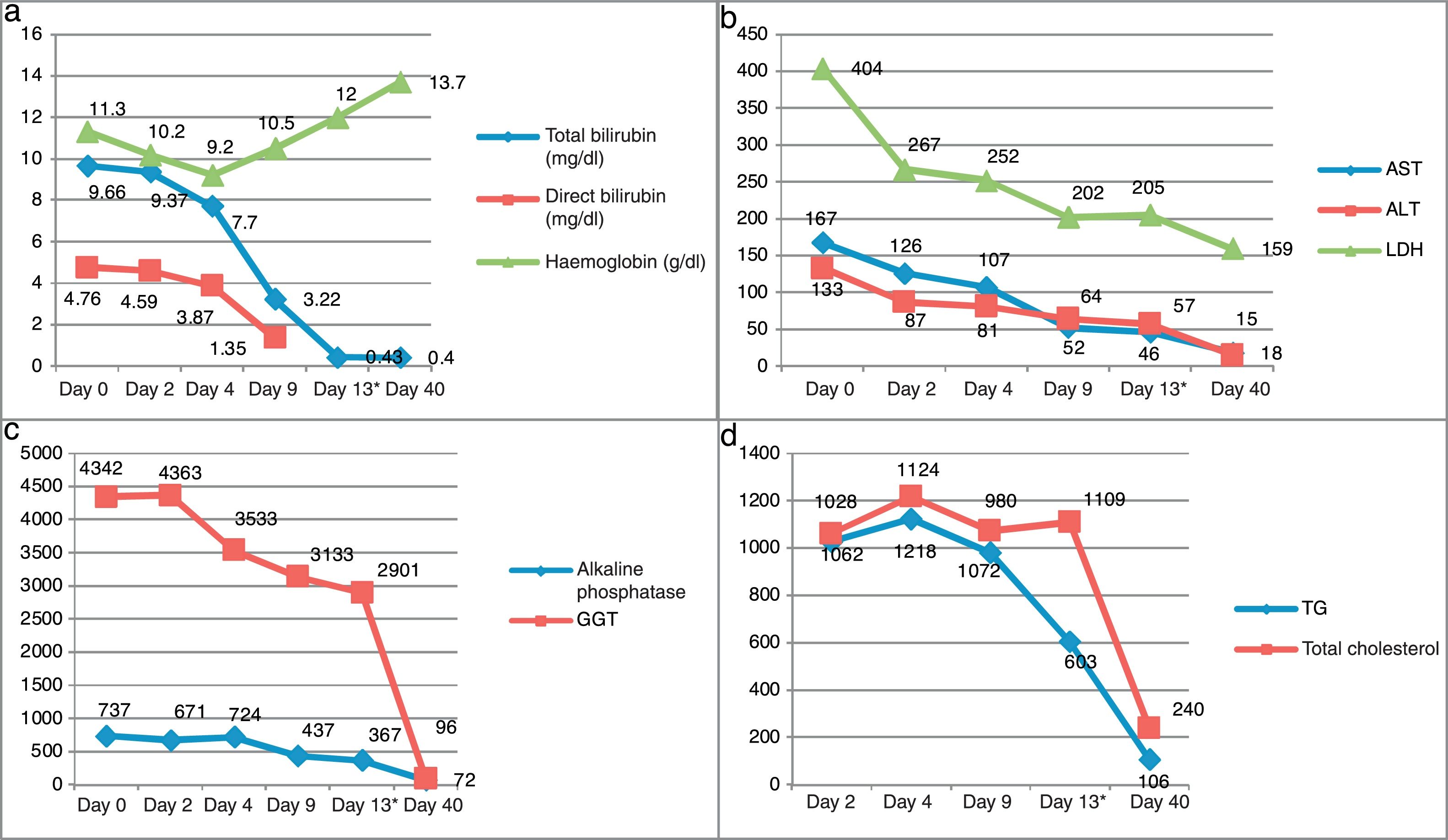
Blood analysis showed total bilirubin 9.66mg/dl; direct bilirubin 4.59mg/dl; Cr 0.69mg/dl; ALP 855IU/l; GGT 212IU/l; GOT (AST) 167IU/l; GPT (ALT) 133IU/l; LDH 454IU/l; Hb 11.3g/dl; Haematocrit 35%; MCV 95fl; platelets 234,000; INR 1.03; triglycerides 1.124mg/dl, and total cholesterol 1.109mg/dl. Coombs test and serology for hepatitis A, B and C viruses were negative. Severe hyperlipidaemia was found, not present in previous laboratory tests, as well as anaemia, with elevated LDH and reticulocytes, and decreased haptoglobin, suggestive of non-autoimmune haemolytic anaemia. No coagulopathy or hypoalbuminaemia were detected. Vitamin B12 and folic acid values were normal.
Investigations were completed with an ultrasound and an abdominal CT which showed the liver with a marked increase in refraction in relation to hepatic steatosis, without signs of cirrhosis or portal hypertension or space-occupying lesions.
In the first 48h the patient had symptoms of anxiety and distal tremor in the context of alcohol withdrawal, but responded well to clomethiazole and benzodiazepines. As he was clinically stable and his blood test results had improved, he was discharged from hospital.
Three weeks later the patient was assessed in the hepatology outpatient clinic, and his lipid profile and bilirubin, transaminase and haemoglobin levels had virtually returned to normal (Fig. 1). He was asymptomatic and had been abstaining from alcohol. He had liver elasticity of 4.1kPa.
The signs and symptoms are compatible with Zieve's syndrome, fulfilling the criteria of acute onset of haemolytic anaemia, hyperlipidaemia and jaundice. We opted for conservative management and the patient made a spontaneous recovery with supportive treatment and abstinence from alcohol.
It is over 50 years since Zieve's syndrome was first described and the aetiopathogenesis remains unclear today. Many different theories have been put forward. Zieve1 initially suggested that the presence of haemolytic anaemia could be secondary to the exposure of the erythrocyte membranes to a high presence of haemolysins (lysolecithin and lysocephalin). Circulating blood lipids would perform a protective role against these enzymes but, when abruptly reduced, the high persistence of haemolysins could lead to the onset of haemolysis.2 However, that has been questioned, as cases have been reported in which the haemolysis coincided with the acute phase of plasma lipid elevation.3 Melrose et al.4 proposed that it could be a reaction to excessive alcohol consumption in predisposed individuals, perhaps secondary to an enzymatic defect, which prevents adequate detoxification of alcohol metabolites in blood. This would lead to an excess of acetaldehyde,5 which has been shown to be able to bind to the red blood cell membrane and create stomatocytes, affecting the flow of ions through the membrane and so making it unstable. Another aspect they identified was a transient instability of pyruvate kinase, which results in adenosine 5′ triphosphate (ATP) depletion in the blood cells.
Because of its relationship with chronic alcohol consumption, Zieve's syndrome can be misinterpreted as alcoholic hepatitis.
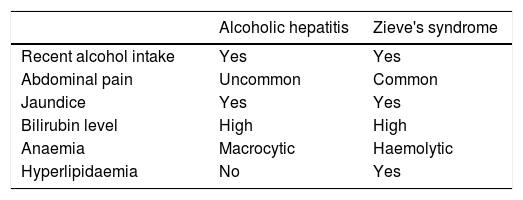
Our aim with this case was to provide a reminder about the existence of Zieve's syndrome, which occurs in patients who do not necessarily have underlying chronic liver disease and who recover spontaneously in 3-4 weeks after stopping drinking alcohol,5 compared to severe alcoholic hepatitis, which can require invasive diagnostic tests and administration of corticosteroids, as well as having a worse prognosis. Table 1 shows a comparison between the two conditions (Table 1).6
Comparison between acute alcoholic hepatitis and Zieve's syndrome.6
| Alcoholic hepatitis | Zieve's syndrome | |
|---|---|---|
| Recent alcohol intake | Yes | Yes |
| Abdominal pain | Uncommon | Common |
| Jaundice | Yes | Yes |
| Bilirubin level | High | High |
| Anaemia | Macrocytic | Haemolytic |
| Hyperlipidaemia | No | Yes |
Please cite this article as: Gotor Delso J, Espina Cadena S, García Cámara P, Sanz Segura P, Llorente Barrio M, Monzon Baez R, et al. Síndrome de Zieve, una entidad infradiagnosticada. Gastroenterol Hepatol. 2019;42:431–432.