In 2008, ESPGHAN published a position paper on complementary feeding providing recommendations to health care professionals. Cultural and socio-economic factors might affect the compliance to these orientations.
AimTo estimate the prevalence of inadequacies during complementary feeding (ESPGHAN, 2008) and its association with different ethnic backgrounds.
MethodsCross-sectional survey of a convenience sample of caretakers of children up to 24 months of age in a single community health centre in Greater Lisbon, through a volunteer, self-applied questionnaire.
ResultsFrom a sample of children with wide cultural diversity, 161 valid questionnaires were obtained (median child's age 9 months, median mother's age 32 years). The prevalence rate of at least one complementary feeding inadequacy was 46% (95%CI: 38.45–53.66). The commonest inadequacies were: avoiding lumpy solid foods after 10 months of age (66.7%), avoidance or delayed introduction of foods beyond 12 months (35.4%), introduction of gluten beyond 7 months (15.9%) or salt before 12 months (6.7%). For each increase of 1 month in the age of the child, the odds of inadequacies raised 36.7% (OR=1.37; 95%CI: 1.20–1.56; p<0.001). The odds for inadequacies in children of African or Brazilian offspring was three times higher that of Portuguese ancestry (OR=3.31; 95%CI: 0.87–12.61; p=0.079). The influence of grandparents was related to an increase in the odds of inadequacies (OR=3.69; 95%CI: 0.96–14.18; p=0.058).
ConclusionInadequacies during complementary feeding are frequent and may be influenced by the cultural background.
Em 2008 a ESPGHAN publicou recomendações sobre diversificação alimentar para os profissionais de saúde. Fatores socioeconómicos e culturais podem, no entanto, afetar o cumprimento destas orientações.
ObjectivosPretendemos estimar a prevalência de inadequações às orientações publicadas e explorar a associação entre inadequações e as diferentes influências culturais.
MétodosEstudo transversal, baseado num questionário voluntário de autopreenchimento, fornecido a uma amostra de conveniência de pais de crianças até aos 2 anos de idade, que frequentava um Centro de Saúde da Grande Lisboa.
ResultadosObtivemos 161 questionários válidos de uma amostra de crianças com ampla diversidade cultural (idade mediana das crianças 9 meses, idade mediana das mães 32 anos). A taxa de prevalência de pelo menos uma inadequação foi de 46% (IC95%: 38,45-53,66). As inadequações mais frequentes foram: evicção de alimentos grumosos ou menos triturados após os 10 meses de idade (66,7%), evicção ou atraso na introdução de alimentos após os 12 meses (35,4%), introdução de glúten após os 7 meses (15,9%) ou introdução de sal antes dos 12 meses (6,7%). Por cada aumento de um mês na idade da criança o risco de inadequação aumentou 36,7% (OR=1,37; IC95%: 1,20-1,56; p<0,001). Para além disso, o risco de inadequação para descendentes de famílias africanas ou brasileiras foi 3 vezes superior ao dos descendentes de portugueses (OR=3,31; IC95%: 0,87-12,61; p=0,079). A influência dos avós aumentou o risco de inadequações (OR=3,69; IC95%: 0,96-14,18; p=0,058).
ConclusõesNeste estudo foi encontrada uma elevada prevalência de inadequações durante a diversificação alimentar e este facto poderá ser influenciado por características culturais.
Complementary feeding (CF) is defined as the introduction of solid foods and liquids other than breast milk, infant formula or follow-on formula into an infant's diet.1 Timely introduction of appropriate complementary foods is essential for adequate nutritional supply and development of children.1,2 In 2008, the European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) published a position paper on CF providing recommendations for health care providers.1 However, different cultural and socio-economic factors (e.g., low-income of the family, mother's age and education) can interfere with the compliance to some of the health-care provider's recommendations.2–4 Fear of food allergy may also influence parents and caregivers during the weaning process.5
The primary aim of this exploratory study was to estimate the prevalence of inadequacies during CF, according to the ESPGHAN position.1 It was further aimed to identify inadequacies in families with different cultural or ethnic backgrounds. We tested the hypotheses that inadequacies are frequent and that caretakers with self-reported non-Portuguese cultural background have more inadequacies according to the ESPGHAN recommendations.
2Materials and methods2.1Study designA cross-sectional exploratory survey on a convenience sample of caretakers of children up to 24 months of age, attending well-child visits, was conducted at a single public Health Primary Care Centre in Greater Lisbon, Portugal, between September and December 2010.
2.2Local contextThe Primary Care Centre where the study was undertaken served a multicultural community, with 7% being immigrant people. Children were attended by family physicians and paediatric specialist nurses. Most of the family physicians received paediatric formation, including about the weaning process, as part of a continuous education programme or during their residency. Because there was a paediatrician until 2008 in this Centre, older family physicians may have been less aware of more recent recommendations.
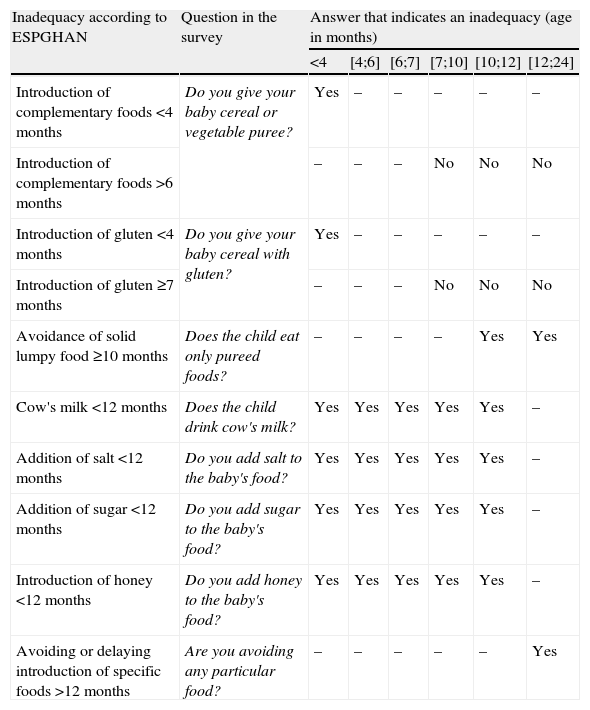
2.3Data collectionA self-applied questionnaire to collect information about current feeding practices, based in the complementary feeding milestones, was designed (Annex 1). This information, together with the age of the child, was used to assess the presence of inadequacies (main endpoint) (Table 1). Inadequacies were defined as unconformities in relation to published ESPGHAN recommendations.1 Information on self-reported cultural background, assumed as a possible explanatory variable, was also collected. Furthermore, we inquired about potential confounders such as social characteristics (mother's age, years of school, working status and self-reported economic difficulties in buying food), family features (main caretaker, number of siblings), place where the child spent most of the day and place where food was prepared (at nursery, home or by the nanny). Face validity of the questionnaire was agreed by an expert panel of paediatricians and family physicians; the questionnaire was tested on-site with a small convenience sample of parents. The study was approved by the involved institutions, following current procedures. An oral informed consent was obtained from each participant.
Summary of expected inadequacies in complementary feeding, according to the 2008 ESPGHAN recommendations (1).
| Inadequacy according to ESPGHAN | Question in the survey | Answer that indicates an inadequacy (age in months) | |||||
| <4 | [4;6] | [6;7] | [7;10] | [10;12] | [12;24] | ||
| Introduction of complementary foods <4 months | Do you give your baby cereal or vegetable puree? | Yes | – | – | – | – | – |
| Introduction of complementary foods >6 months | – | – | – | No | No | No | |
| Introduction of gluten <4 months | Do you give your baby cereal with gluten? | Yes | – | – | – | – | – |
| Introduction of gluten ≥7 months | – | – | – | No | No | No | |
| Avoidance of solid lumpy food ≥10 months | Does the child eat only pureed foods? | – | – | – | – | Yes | Yes |
| Cow's milk <12 months | Does the child drink cow's milk? | Yes | Yes | Yes | Yes | Yes | – |
| Addition of salt <12 months | Do you add salt to the baby's food? | Yes | Yes | Yes | Yes | Yes | – |
| Addition of sugar <12 months | Do you add sugar to the baby's food? | Yes | Yes | Yes | Yes | Yes | – |
| Introduction of honey <12 months | Do you add honey to the baby's food? | Yes | Yes | Yes | Yes | Yes | – |
| Avoiding or delaying introduction of specific foods >12 months | Are you avoiding any particular food? | – | – | – | – | – | Yes |
The parents or caretakers of children attending the well-child clinic were invited to fill in the questionnaire, which was available in the waiting room of the Paediatric Health Department. A single questionnaire was applied, regardless of the child's age or self-reported cultural background. Questionnaires were mostly self-reported, although caretakers who could not read Portuguese properly could ask to have it read and filled in by one of the researchers (SN, MAn), who were paediatric residents, temporarily working in this setting. To reduce social-acceptability bias, anonymity of the questionnaires was pursued and no personal identification data was asked. Questionnaires were available in the waiting room and, after filled in, they were returned into a sealed box in the same room. To reduce recall bias, we have only enquired about current feeding practices, not about past ones. Additionally, questions were formulated to avoid inducing responses (e.g., “Do you feed him/her cereals or soup?” or “Do you add sugar to his/her food?”). The health professionals involved in providing care were unaware of the caretaker's participation in the study. Data from self-reported cultural background and possible confounders were extracted directly from the questionnaires. However, each of the 10 individual inadequacies was defined considering both the answer given and the age of the child at the time of the survey. For instance, “late complementary feeding” was defined as children aged over 6 months reported as not having introduced CF yet. Similarly, “early introduction of cow's milk” was defined as children younger than 12 months already drinking cow's milk. Since a single child could have multiple inadequacies, the number of children with at least one of the possible inadequacies for each age group was calculated. Finally, self-reported cultural background was reclassified into categories (Portuguese/Brazilian/African/other). Missing data on outcomes were managed by excluding the cases.
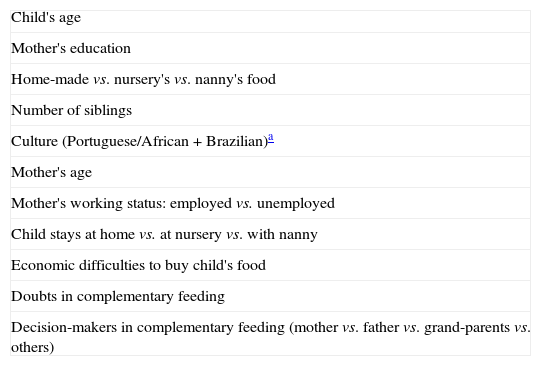
2.4Statistical analysisBeing an exploratory study, no calculation of sample size was made. Prevalence rates were calculated with 95% confidence interval (95%CI). Continuous variables are described with mean and standard deviation or median and centiles, as appropriate. Categorical and binary variables are described using proportions. A logistic regression model was used to test the association between self-reported cultural background and the presence of at least one inadequacy. The variables considered in the model are listed in Table 2. The final variables in the model were included through backward selection, adopting a significance level of p<0.1. Statistical analysis was performed using SPSS® 16.0 (SPSS Inc., Chicago, IL) and OpenEpi software.6
Variables related to feeding patterns introduced in the logistic regression model.
| Child's age |
| Mother's education |
| Home-made vs. nursery's vs. nanny's food |
| Number of siblings |
| Culture (Portuguese/African+Brazilian)a |
| Mother's age |
| Mother's working status: employed vs. unemployed |
| Child stays at home vs. at nursery vs. with nanny |
| Economic difficulties to buy child's food |
| Doubts in complementary feeding |
| Decision-makers in complementary feeding (mother vs. father vs. grand-parents vs. others) |
Complete questionnaires from 161 children were collected (female 53.5%), with median age 9 months (4 months 21st centile (14 children); 6 months 39th centile (43 children); 10 months 55th centile (68 children); 12 months 60th centile (77 children)). The questionnaire was answered by the mother (79.4%), father (19.3%) or other caretakers (1.2%). The mothers had a median age of 32 years (P25=27; P75=36; min=15; max=50 years), had on average 1 child and 77% of them were employed.
The cultural background of the sample was diverse: Portuguese 65% (102/161 cases), African 15.5% (24/161), Brazilian 7.7% (12/161), Slavic 3.2% (5/161), Roma 2.6% (4/161), Chinese 2.6% (4/161), Indian 1.3% (2/161) and other 1.3% (2/161).
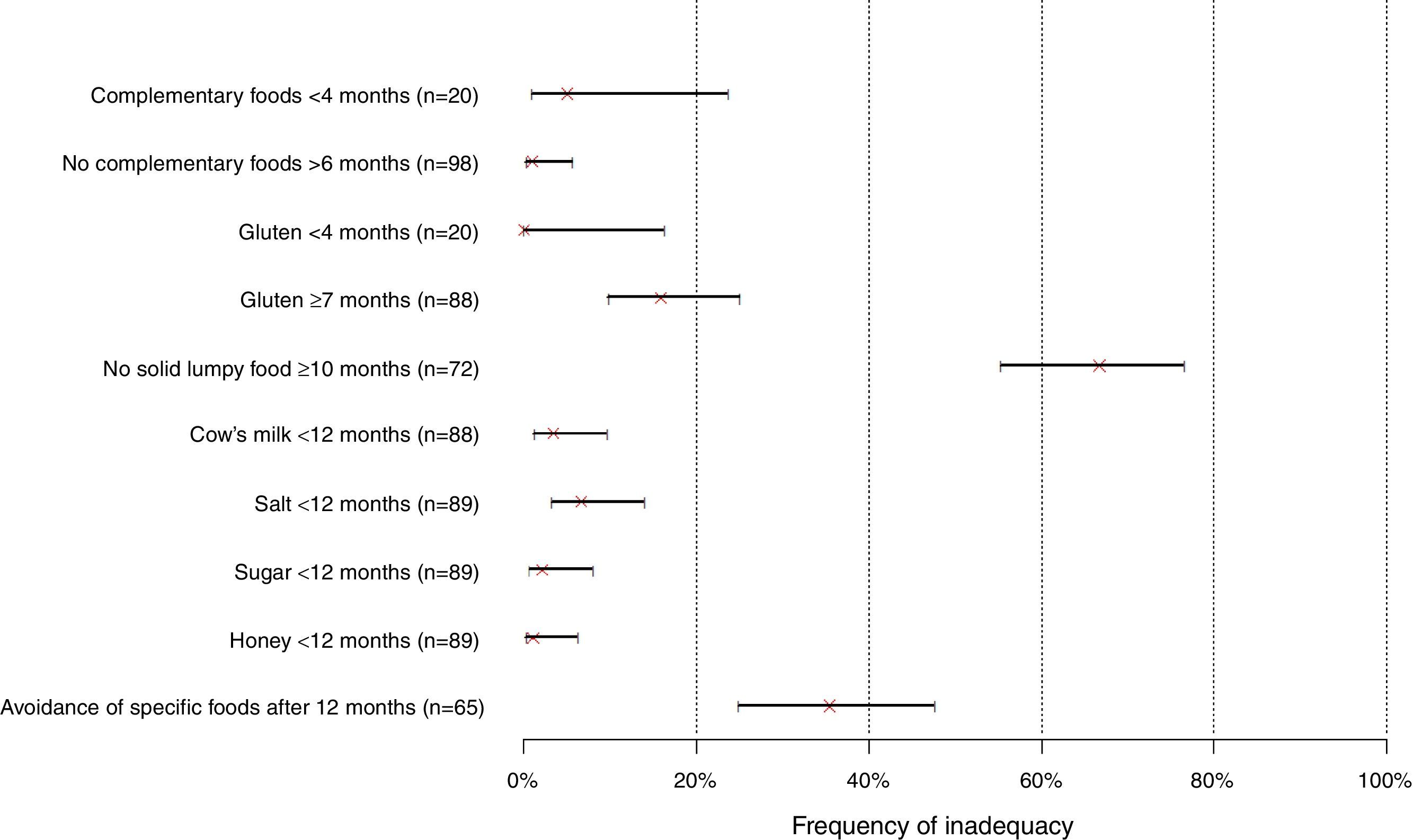
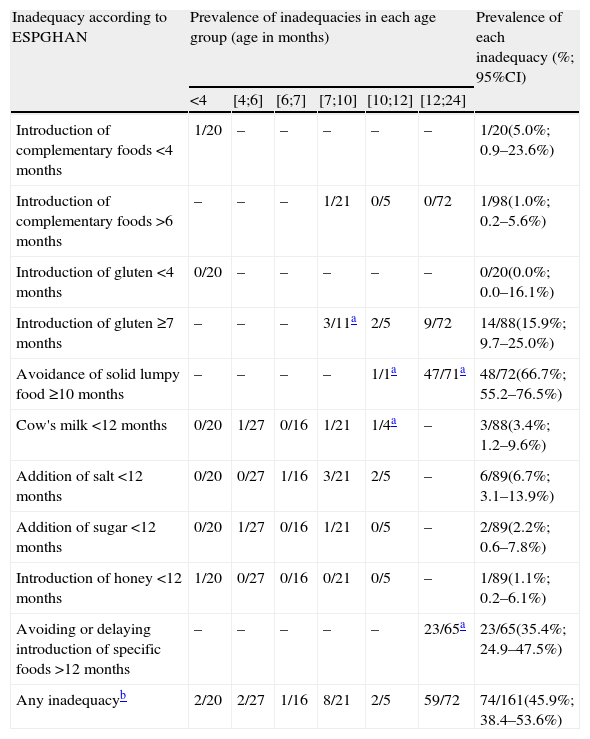
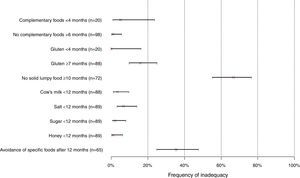
Besides the mother, other decision-makers in CF were the father (60.7%), grandparents (27.7%) and others (11.6%). Economic difficulties to buy the child's food were stated by 13% of the repliers. The global prevalence of inadequacies was 46% (95%CI: 38.45–53.66). The commonest inadequacy was avoidance of lumpy solid foods after 10 months (66.7%; 95%CI: 55.18–76.46) and the least common was introducing cow's milk before 12 months (3.4%; 95%CI: 1.17–9.55). Actual figures and proportions of the inadequacies are presented in Table 3 and Fig. 1. Surprisingly, some expected inadequacies were not reported.
Prevalence of inadequacies, according to the 2008 ESPGHAN recommendations.
| Inadequacy according to ESPGHAN | Prevalence of inadequacies in each age group (age in months) | Prevalence of each inadequacy (%; 95%CI) | |||||
| <4 | [4;6] | [6;7] | [7;10] | [10;12] | [12;24] | ||
| Introduction of complementary foods <4 months | 1/20 | – | – | – | – | – | 1/20(5.0%; 0.9–23.6%) |
| Introduction of complementary foods >6 months | – | – | – | 1/21 | 0/5 | 0/72 | 1/98(1.0%; 0.2–5.6%) |
| Introduction of gluten <4 months | 0/20 | – | – | – | – | – | 0/20(0.0%; 0.0–16.1%) |
| Introduction of gluten ≥7 months | – | – | – | 3/11a | 2/5 | 9/72 | 14/88(15.9%; 9.7–25.0%) |
| Avoidance of solid lumpy food ≥10 months | – | – | – | – | 1/1a | 47/71a | 48/72(66.7%; 55.2–76.5%) |
| Cow's milk <12 months | 0/20 | 1/27 | 0/16 | 1/21 | 1/4a | – | 3/88(3.4%; 1.2–9.6%) |
| Addition of salt <12 months | 0/20 | 0/27 | 1/16 | 3/21 | 2/5 | – | 6/89(6.7%; 3.1–13.9%) |
| Addition of sugar <12 months | 0/20 | 1/27 | 0/16 | 1/21 | 0/5 | – | 2/89(2.2%; 0.6–7.8%) |
| Introduction of honey <12 months | 1/20 | 0/27 | 0/16 | 0/21 | 0/5 | – | 1/89(1.1%; 0.2–6.1%) |
| Avoiding or delaying introduction of specific foods >12 months | – | – | – | – | – | 23/65a | 23/65(35.4%; 24.9–47.5%) |
| Any inadequacyb | 2/20 | 2/27 | 1/16 | 8/21 | 2/5 | 59/72 | 74/161(45.9%; 38.4–53.6%) |
The logistic regression model showed a weak evidence that children of African or Brazilian parents have more inadequacies (OR=3.31; 95%CI: 0.87–12.61; p=0.079) and that Brazilian children have a higher burden of inadequacies (1 vs. >1 inadequacy) comparing with Portuguese or African descendents (p=0.073). Moreover, for each increase in 1 month in the age of the children, there was a 36.7% increase on the odds of inadequacies (OR=1.37; 95%CI: 1.20–1.56; p<0.001). Finally, a weak evidence of increased odds on inadequacies from the influence of grandparents on complementary feeding was found (OR=3.69; 95%CI: 0.96–14.18; p=0.058).
4DiscussionThe results of this study emphasize the high prevalence of inadequacies during the complex and multifactorial process of CF. Almost half of the sample reported at least one inadequacy during the weaning process. The most frequent inadequacy was the delay in introducing lumpy solid food. Furthermore, we observed a tendency for higher proportion of inadequacies in children of parent-reported African/Brazilian compared to Portuguese background, although with a low level of evidence.
This study has an exploratory nature. The setting for the study was chosen to increase the probability to collect data from a wide range of families from the different cultural backgrounds found in Greater Lisbon. Convenience sampling limits the confidence and ability to generalize the results. Caretakers of children that attended well-child visits at the community health centre were invited to answer the questionnaire. Thus, children from families with higher incomes may be underrepresented, as traditionally they are assisted by paediatricians in their private offices. On the other hand, underprivileged children are known not to attend well-child visits regularly. In fact, families reported a 23% unemployment rate, much higher than officially declared for this same region at the end of 2010.7 Therefore, the study may have suffered from a recruitment bias towards the central socio-economic quintiles.
This cross-sectional study was based on the feeding practices of each child at the time of the questionnaire and targeted contemporary children from 3 to 24 months of age, in an attempt to avoid recall bias. This option, however, precluded the assessment of prior inadequacies (e.g., if a child had been weaned before 4 months, but the questionnaire was filled at the age of 6 months, that inadequacy was missed).
The entirely voluntary participation may have led to a healthy volunteer bias, which cannot be accounted for, since data on non-responders were not collected. Also, in spite of the efforts to make the survey results anonymous, two of the researchers in the study (SN, MAn) were also health care providers involved in the health surveillance of the children included in the study. This may have induced a social acceptability bias. Taken together, it is expected that these biases may reduce the reporting of inadequacies, leading to an underestimation of its true prevalence.
In spite of the short time span of the study (4 months) and a scheduled interval of 3 months for well-child visits in children above the age of 6 months according to the Portuguese Health Surveillance Program, it is impossible to rule out that the questionnaire might have been answered more than once by caretakers of the same child (e.g., at ages 4 and 6 months). This would lead to a violation of the assumptions of the logistic regression model. Due to the anonymous data collection, one cannot be sure of how often this multiple observations (if any) might have happened. Nevertheless, cases were matched for child's gender, mother's level of education, self-reported cultural background and age and only three cases were found that might match with each other. Hence, one may assume that no major violation of the assumptions of the model occurred. Finally, due to time restrictions, the number of children recruited was low. This explains the large width of the confidence intervals, especially for inadequacies occurring before 4 months of age.
The most frequent inadequacy was the delay in introducing lumpy solid food. This trend has already been reported in other studies with significantly more feeding problems in these children notably at the age of 7 years-old.8 One possible explanation to keep offering homogeneous consistency food may be the general tendency of parents to overprotect and turn their child's meals easier. Nevertheless, it is assumed that around 10 months of age, there may be a “window of opportunity” to introduce more solid food, after which, feeding difficulties may develop.1
Only two children had either premature (before 4 months) or delayed (after the age of 6 months) introduction of CF, which is less frequent than reported in previous studies conducted in Portugal.9,10 Also in Sweden, few children receive early or late CF.11 Besides, cow's milk had only been introduced in 3.4% of the children younger than 12 months in our study, which is substantially inferior to the 30% previously verified in Greater Lisbon.9
In most Portuguese Public Primary Health Centres, including the one where the study was performed, caregivers are advised to delay the introduction of some foods until 24 months (e.g., soft fruits, seafood, nuts), egg white (until 13 months) and to maintain a gluten-free diet until the 6th month of life. This may help to explain the high reported prevalence of these behaviours in our survey, meaning that parents are adhering to some local recommendations. In the Primary Health Centre where the study was undertaken and before its beginning, healthcare professionals used to promote delayed introduction of these foods to protect against allergy and celiac disease. Delaying food introduction is not in agreement with the latest evidence-based practice as summarized in the ESPGHAN recommendations and can actually increase the incidence of these diseases. It is now recommended to introduce small amounts of gluten between 4 and 7 months of age, preferably along with breastfeeding. This attitude showed a decrease in the occurrence of celiac disease autoimmunity in children at increased risk for the disease.12 Delaying or avoiding potentially allergenic foods (such as fish or eggs) do not seem to reduce allergy, not even in children with a family risk of atopy, moreover, it can cause nutritional deficits with cognitive and immune repercussion.1 Evidence shows that regular fish consumption before 12 months of age appears to be associated with a reduced risk of allergic disease and sensitization to food and inhalant allergens during the first 4 years of life.13 Another example, a decrease in the incidence of peanut's allergy in Israeli children was found in those that had introduced peanuts earlier, at a regular and important quantity basis. Therefore, some authors support early introduction of peanuts during infancy, rather than its avoidance.14 On the contrary, Cow's milk should still be postponed until 12 months of age. Premature introduction of cow's milk is associated with iron deficiency, since cow's milk is a poor source of iron and early introduction can lead to microscopic intestinal bleeding.1,15
This survey took place in a multicultural urban area. It has been suggested that non-native cultures tend to comply worse with local CF recommendations.2,3 We found an increased trend for inadequacies in children with African or Brazilian backgrounds, with an estimated threefold increase of the occurrence of inadequacies in these children comparing with children with Portuguese ancestry. Immigrant mothers, usually develop some “acculturation” to the new society but it may be incomplete. Pak-Gorstein et al. reported that foreign mothers with less American “acculturation” (not USA born, nor English speakers or on a short stay) practiced more and more prolonged breastfeeding than native Americans, mainly if originated from a low socio-economic level.16
The ESPGHAN committee recognizes that the evidence supporting CF practices is weak and often focused on surrogate outcomes.1 In this context, it is difficult to know the impact of the inadequacies found in our study in the children's future health. It is also largely unknown if the trend for more reported inadequacies in children of Brazilian and African backgrounds will have a negative repercussion in their health. A longitudinal study designed to assess the impact of these inadequacies on weight, height, blood pressure and neurodevelopment would provide insight into this issue.
Some evidence of the influence of grandparents on inadequate CF decisions was unexpected. This issue was not a pre-specified hypothesis in our study and must be interpreted with caution due to low statistical significance. In the Portuguese society, grandparents have an important influence in child bearing and feeding counselling, due to the respect for family traditions and the acknowledgement of their experience on childcare. Hence, the role of grandparents should be further explored.
Some information provided by the healthcare professionals in this Primary Health Centre about CF was not supported by the current best evidence. One possible explanation for this is the lack of national guidelines for child weaning endorsed by the Portuguese Health Authorities and the major scientific societies. It is also important to note that between the publication of ESPGHAN recommendations (January 2008) and our data collection (last quarter of 2010) 30 months had lapsed. This points out to the problem of dissemination of information. Furthermore, it has been repeatedly shown that guideline development alone does not change clinical practice.17,18 Our study highlights that paediatric residents, who have a mandatory rotation in Primary Care Centres, could disseminate relevant and recent paediatric evidence to busy primary care nurses and doctors who also have to care for non-paediatric populations.
This exploratory study suggests that inadequacies in CF practices may be highly prevalent in the population served by this Portuguese urban Primary Health Centre. Due to several biases that can underestimate the prevalence of inadequacies, these figures should be seen as the best case scenario. The inadequacies may be more common in children pertaining to immigrant families. In a multicultural society, ethnic feeding practices with unproved harmful effect should not be discouraged. More attention should be given to immigrant communities if further studies show poorer clinical outcomes associated to feeding inadequacies related to the cultural background.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.