Gastroesophageal variceal bleeding is the most common cause of upper gastrointestinal bleeding in patients with liver cirrhosis. In contrast, duodenal varices are rare and their potential to bleed is low. However, when it occurs, it can be fatal – mortality rate of 35–40%.1 Although the recognition of ectopic varices has long been described, therapeutic procedures have not yet been established for bleeding from duodenal varices. Endoscopic band ligation, sclerotherapy, transjugular intrahepatic portosystemic shunt, balloon-occluded retrograde transvenous obliteration, and resection of a segment of bleeding site have been used for treatment.2–5
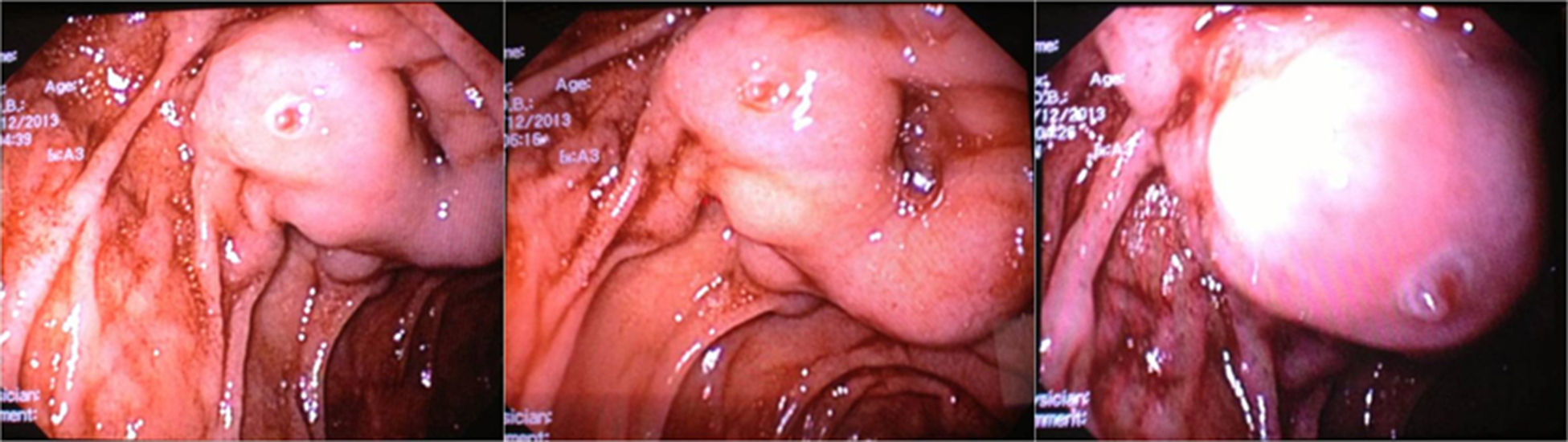
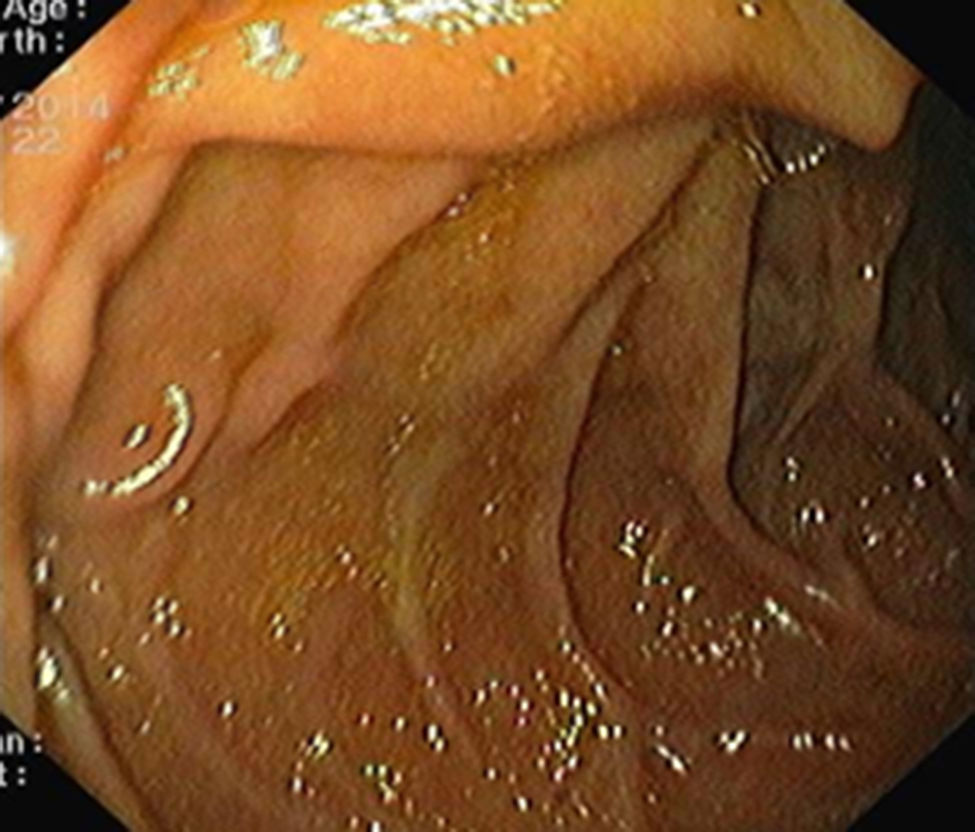
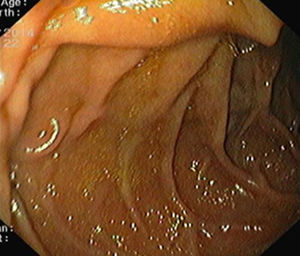
We present a case of a 48-year-old man with a known history of liver cirrhosis secondary to chronic hepatitis C infection. He was admitted in emergency department due to hematemesis and melena for 24h. He was hemodynamically stable, and had a hemoglobin level of 7.1g/dL. The patient was treated with intravenous (IV) pantoprazole, IV octreotide and IV cetfriaxone. Emergency esophagogastroduodenoscopy revealed small esophageal varices without stigmata of hemorrhage. Apart from mild portal gastropathy, no other gastric lesions suggestive of bleeding were noted. Finally, a duodenal varix with a fibrin plug at the second portion, approximately 1cm in diameter, was found (Fig. 1). N-butyl-2-cyanoacrylate (histoacryl) was injected to the duodenal varix, and bleeding was successfully controlled. Subsequently, the patient remained hemodynamically stable, with no recurrent bleeding. Six months later, a follow-up endoscopy showed large esophageal varices, which were treated with endoscopic band ligation, and severe hypertensive gastropathy. There were not any signs of duodenal varices (Fig. 2).
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.