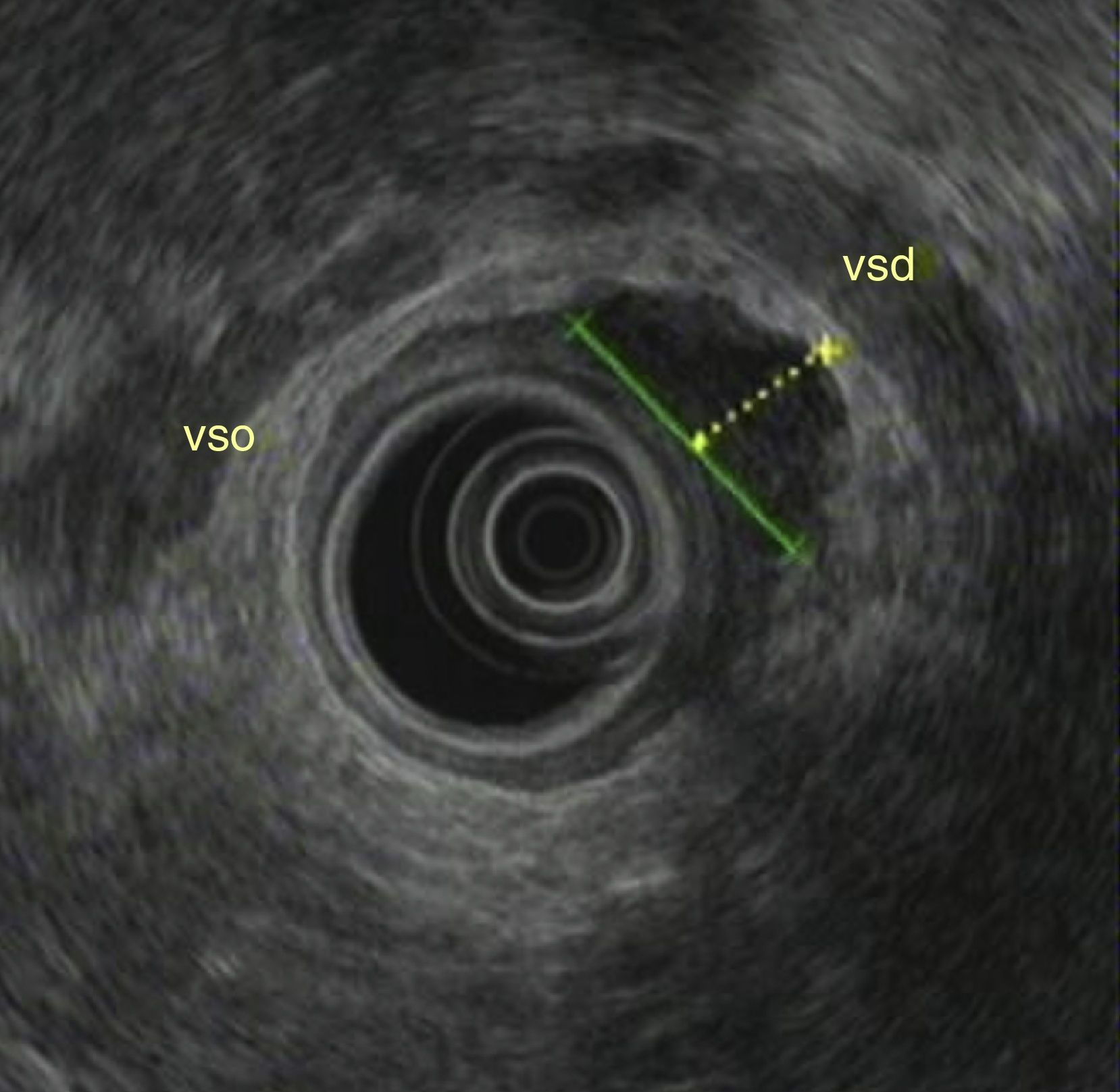
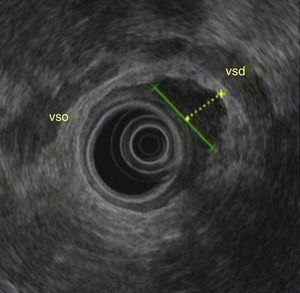
A 73-year-old male patient with a history of pulmonary tuberculosis in childhood, a gastric adenocarcinoma (intestinal type) T1N0M0 (TNM classification), submitted to a partial gastrectomy Roux-en-Y, 10 years before, and a T1 low-grade papillary bladder urothelial carcinoma treated with a transurethral resection and epirubicin, 1 year before, reported anal pain and fever for the last 5 days. The patient denied diarrhea, hematochezia or weight loss. In the anoscopy a painful bulging lesion with 2–3cm was detected in distal rectum. Anorectal endoscopic ultrasonography (EUS) showed a heterogeneous, irregular lesion in the distal right rectal wall, with a central hypoechogenic area measuring 26mm on its longest axis and 14mm on its shortest axis, originated in the muscularis propria (Fig. 1). We performed a (ultrasound guided) fine needle (22 gauge) aspiration (FNA), three passages, with collection of solid and fluid material (Fig. 2). The patient did prophylaxis with ciprofloxacin for 5 days after the procedure. Culture of fluid revealed polymicrobial flora, probably contamination. Cytology revealed the presence of leukocytes and necrosis material, supporting the hypothesis of rectal abscess. The drainage of the abscess was proposed to the patient, but he refused the procedure. An antibiotic treatment with trimethoprim–sulfamethoxazole was given during 14 days, with resolution of symptoms. After 1 month, another endoscopic ultrasonography showed no lesions (Fig. 3).
1CommentaryPerirectal abscesses are frequently the manifestation of an infected anal gland,1 usually originating anal pain.2 In this case, anorectal abscess was the most probable diagnosis, so anorectal EUS was performed. Nevertheless the image was atypical and the internal orifice or fistula was not observed, so FNA was executed to achieve a definitive diagnosis, which was supported by the cytology sample. Drainage is the first choice for therapy,3 but in this case, because the patient refused that solution, we chose to treat him only with antibiotics, achieving an effective management of the abscess.
We emphasize the image of this perirectal abscess and the importance of fine needle aspiration for the diagnosis of atypical rectal abscess.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestNo conflicts of interest to declare.