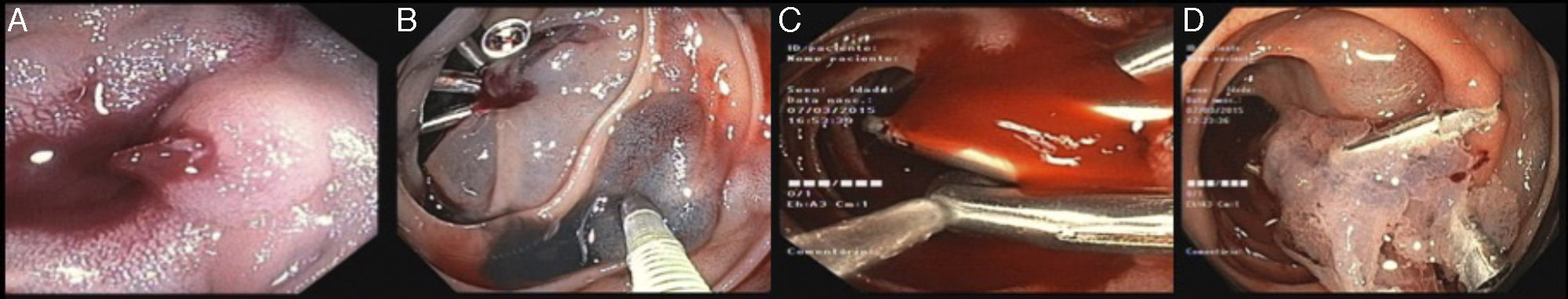
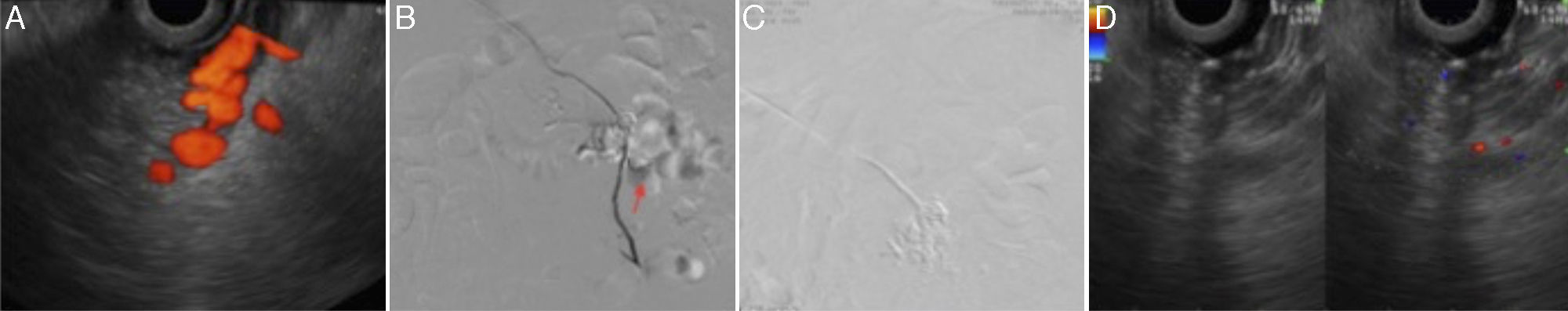
An 80-year-old male patient, with no past medical history of cirrhosis, was admitted to the emergency department of our hospital, with sudden massive hematochezia and syncope. Shortly after admission, the patient developed hemorrhagic shock, requiring substantial transfusion support (10 units of erythrocyte concentrate, 4 units of fresh frozen plasma, 1 platelet pool and 3g of fibrinogen), renal and respiratory failure with the need of invasive mechanical ventilation. Urgent esophagogastroduodenoscopy, ileocolonoscopy and CT-angiography were inconclusive. Push enteroscopy identified an intermittent spurting hemorrhage in the third portion of the duodenum. The underlying source of bleeding was initially misinterpreted as being a Dieulafoy's lesion. Thus, endoclips were applied, with initial effective hemostasis, and tattooing was performed (Fig. 1A and B). However, severe rebleeding occurred 48h after the procedure, with recurrence of hemodynamic instability. A second enteroscopy identified an ectopic duodenal varix with active oozing underlying the previously applied endoclips. Cyanoacrylate injection was hampered by compromised visualization of the varix (because of the previously applied endoclips and ongoing bleeding), but provided hemostasis (Fig. 1C and D). To evaluate the efficacy of cyanoacrylate injection, radial endoscopic ultrasound (EUS) was performed and showed patency (positive Doppler flow) of this large duodenal varix (Fig. 2A). In a multidisciplinary team meeting, it was decided to perform angiographic therapy, after post hoc evaluation of CT-angiography that suggested an ectopic varix with approximately 20mm fed by a collateral of the superior mesenteric vein. Percutaneous (transhepatic) portography allowed the identification and selective catheterization of the varix. A communicating collateral from the superior mesenteric vein feeding the duodenal varix was successfully embolized during angiography with coils (Fig. 2B and C). Postprocedure EUS confirmed absence of Doppler flow in the duodenal varix (Fig. 2D). The patient's recovery was uneventful. No signs of cirrhosis or portal hypertension were documented on follow-up and the etiology of the ectopic varix remained unknown.
Push enteroscopy identified an intermittent spurting hemorrhage in the distal duodenum, initially misinterpreted as being a Dieulafoy's lesion (A). Endoclips were applied, with initial hemostasis, and tattooing was performed (B). A second enteroscopy identified an ectopic duodenal varix with active oozing. Cyanoacrylate injection was hampered by compromised visualization of the varix (endoclips and ongoing bleeding), but provided hemostasis (C).
After two attempts of endoscopic therapy, EUS was performed and showed patency of a large duodenal varix (A). Percutaneous transhepatic portography allowed the identification and selective catheterization of the varix (arrow) and extravasation of contrast to duodenum (B). A communicating collateral from the superior mesenteric vein feeding the duodenal varix was successfully embolized with coils during angiography (C). Postprocedure EUS confirmed the absence of Doppler flow in the duodenal varix (D).
Ectopic varices account for 1–5% of all variceal bleeding in the setting of portal hypertension and may present as massive obscure gastrointestinal (GI) bleeding.1 Their presence should be considered in patients with portal hypertension and GI bleeding when both upper endoscopy and ileocolonoscopy are not conclusive.1 In the absence of liver disease or signs of portal hypertension this diagnosis can be challenging. The endoscopic approach to the underlying bleeding lesion was initially ineffective, stressing out the difficulty of the diagnosis and management of massive bleeding from an ectopic varix in this setting.
Although the role of EUS in GI bleeding is not well defined and not considered in the current guidelines,2 EUS can be useful in the diagnosis and management of refractory GI bleeding, particularly from vascular lesions.3,4 In this specific case, EUS was essential for the definitive diagnosis of the underlying ectopic varix and to monitor the efficacy of the delivered therapy, evaluating the permeability of the underlying bleeding varix. Therapy of ectopic varices is not well established and most authors consider endoscopic cyanoacrylate injection as the first-line therapy.1 As in the present case, angiographic techniques can be a valuable alternative in the management of bleeding vascular lesions, mainly in patients with massive obscure GI bleeding with hemodynamic instability.5
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
DisclosuresAll authors have approved the manuscript and agree with its submission to GE – Portuguese Journal of Gastroenterology. All authors have nothing to disclose and there are no funding to declare.
Conflicts of interestThe authors have no conflicts of interest to declare.