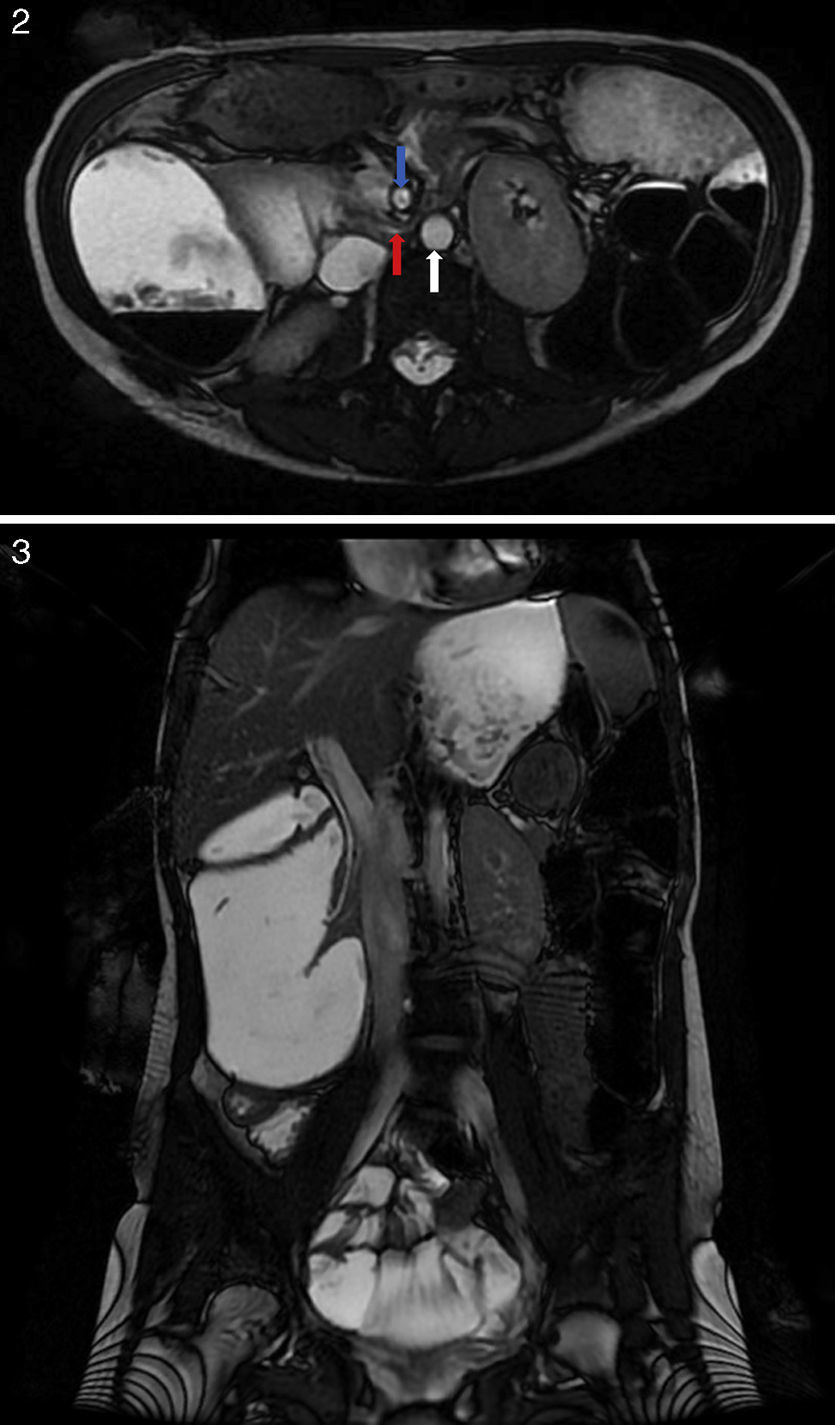
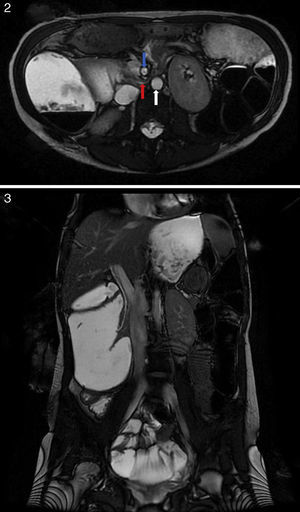
A 20-year-old woman presented to our department with a 10-year history of mild abdominal discomfort and postprandial vomiting slightly relieved by lateral decubitus position. These episodes occurred once a month and led to progressive weight loss. Her past medical history was otherwise unremarkable. She denied alcohol or drug abuse and was not on any kind of medication. The only positive finding on the physical examination was a low body mass index (18kg/m2). Her haemoglobin, blood sugar levels and reactive C-protein were on the normal range. Concerning the family history, her mother was diagnosed with superior mesenteric artery syndrome in her twenties. Upper endoscopy was incomplete due to loop formation but revealed a dilated stomach filled with undigested food material and a dilated duodenal bulb with normal mucosa. Upper gastrointestinal series (Fig. 1) showed a hypotonic stomach followed by a 10cm pouch corresponding to the duodenum where the contrast accumulated. For further evaluation, the patient underwent abdominal magnetic resonance imaging (Fig. 2 and 3) which revealed an abrupt reduction of the duodenal lumen (red arrow) at the transition of its 3rd to 4th part due to extrinsic compression between the superior mesenteric artery (blue arrow) and the aorta (white arrow). Hence it was diagnosed superior mesenteric artery syndrome (SMAS). The patient was then referred to the surgical department and underwent duodenojejunostomy, with complete resolution of the symptoms and subsequent weight gain.
Superior mesenteric artery syndrome, also known as Wilkie's syndrome or cast syndrome, is a rare cause of proximal intestinal obstruction characterized by the compression of the third portion of the duodenum when the space between the superior mesenteric artery and the aorta becomes narrower.1,2 In most cases it is related to the loss of the mesenteric fat pad in conditions with significant weight loss such as malignancy, malabsortion syndromes, drug abuse and anorexia nervosa. Some surgeries, such as corrective spinal surgery for scoliosis, may precipitate SMAS due to the distortion of normal anatomy, which can also occur as a congenital anomaly.1–3 A familial association of SMAS has rarely been reported in the literature.4,5
The diagnosis of SMAS requires a high index of suspicion since the symptoms are not specific; oral contrast imaging studies usually give the diagnosis.
The treatment can be conservative with gastrointestinal decompression, correction of electrolyte abnormalities and nutritional support but if it fails there are several surgical options.1,2
This is another rare case of familial clustering of SMAS suggesting a possible genetic predisposition. Interestingly, in this case the weight loss is most likely the consequence than the cause of the syndrome.
Conflict of interestThe authors have no conflicts of interest to declare.