Mucosal prolapse polyps (MPPs) are rare inflammatory lesions that are part of the mucosal prolapse syndrome. We present the case of a 40-year-old male with history of constipation referred to our institution with suspected rectal malignancy due to hematochezia and a palpable rectal mass. Colonoscopy revealed a 25mm wide lesion suggestive of subepithelial origin but with marked erythema and erosion in the mucosa. Crypt dilatation and distortion, mixed inflammatory infiltrate and fibrosis were apparent on histological evaluation after bite-on-bite biopsies. Due to the initial suspicion of malignancy, resection was decided after discussion with the patient. However, due to non-elevation partial resection was performed allowing the diagnosis of MPP. Hematochezia ceased after obstipation treatment and endoscopic follow-up showed maintenance of the lesion with the same characteristics except for reduced dimension. MPP may mimic neoplastic lesions and should be considered in the differential diagnosis of rectal masses. History, endoscopy and histological characteristics are all necessary and important in the diagnosis of MPP.
Os pólipos de prolapso mucoso (MPPs) são lesões inflamatórias raras enquadradas na síndrome de prolapso mucoso. Apresentamos o caso de um homem, 40 anos, com antecedentes de obstipação, referenciado à nossa instituição por suspeita de neoplasia do reto devido a hematoquésias e lesão palpável ao toque retal. A colonoscopia mostrou uma lesão com 25mm, de aspeto subepitelial, com mucosa marcadamente eritematosa e erosionada. As biopsias bite-on-bite revelaram dilatação e distorção das criptas, infiltrado inflamatório misto e fibrose. Devido à suspeita inicial de neoplasia foi decidida resseção após discussão com o doente, que não foi possível devido à elevação inadequada da lesão. Efetuada resseção parcial, permitindo o diagnóstico seguro de MPP. As hematoquésias cessaram após tratamento da obstipação. Os MPPs podem mimetizar lesões neoplásicas anorrectais devendo ser incluídos no diagnóstico diferencial. A conjugação da história clínica com os aspetos endoscópicos e histológicos é fundamental para o diagnóstico correto e orientação adequada.
Prolapsing mucosal polyps were first described by Franzin et al. in 1985 and are benign colonic lesions macroscopically resembling inflammatory polyps and histologically characterized by elongated and distorted glands with hyperplastic features, surrounded by proliferation of smooth muscle fibers from the muscularis mucosae.1,2 These benign colonic lesions were associated with diverticular disease,2 solitary rectal ulcer syndrome,1 rectal prolapse3 and they were also found in patients without associated conditions. Here we present the case of a patient with a mucosal prolapse polyp (MPP) without associated rectal prolapse that was initially mistaken with a malignant lesion.
2Clinical caseA 44 years old male with history of constipation was referred to our institution due to hematochezia and a palpable mass on rectal examination, without other symptoms namely weight loss. Constipation was present for years; the patient had bowel movements every other day, with hard stools and straining but without rectal digitation. There was no familial history of colorectal cancer. The abdominal palpation was normal, without masses or tenderness and on rectal examination a mobile tender mass was palpated on the anterior rectal wall. Hemoglobin level was normal (13.6g/dL). The patient had a colonoscopy in another institution suggesting a rectal malignancy although biopsies were inconclusive.
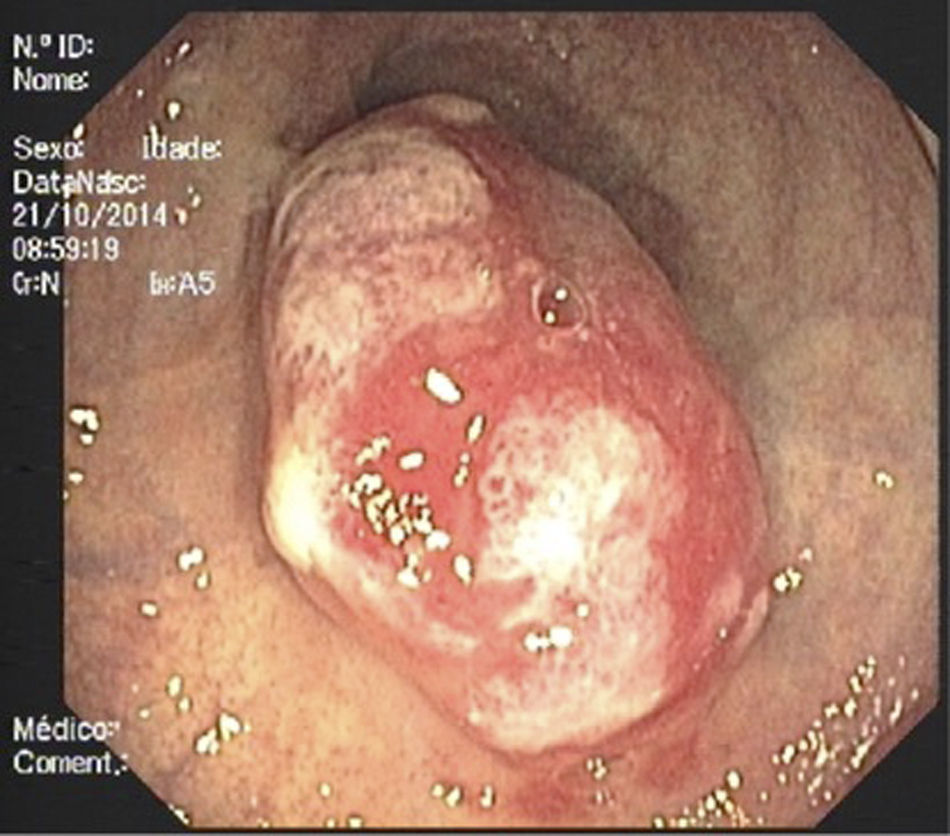
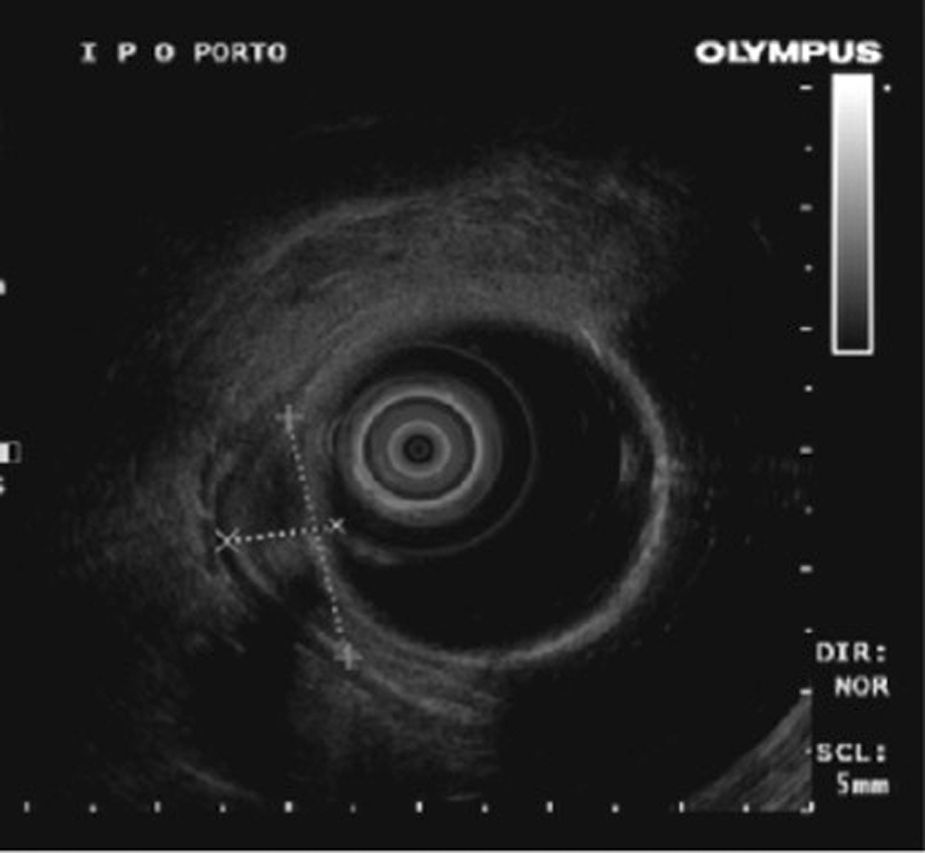
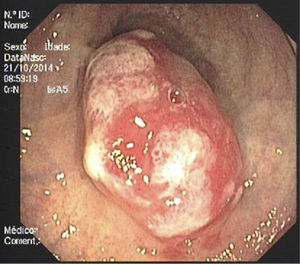
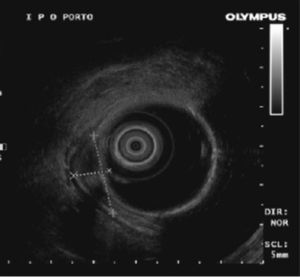
A second colonoscopy at our institution revealed a 25mm soft lesion suggestive of subepithelial origin although the mucosa was erythematous, with areas of irregularity and erosion (Fig. 1). Endoscopic ultrasonography showed a well demarcated, hypoechogenic lesion with origin in muscularis mucosae and there were no regional adenopathies (Fig. 2). Crypt dilation and disorganization, granulation tissue, fibrosis and a polymorphic inflammatory infiltrate in lamina propria were found on histological evaluation after bite-on-bite biopsies.
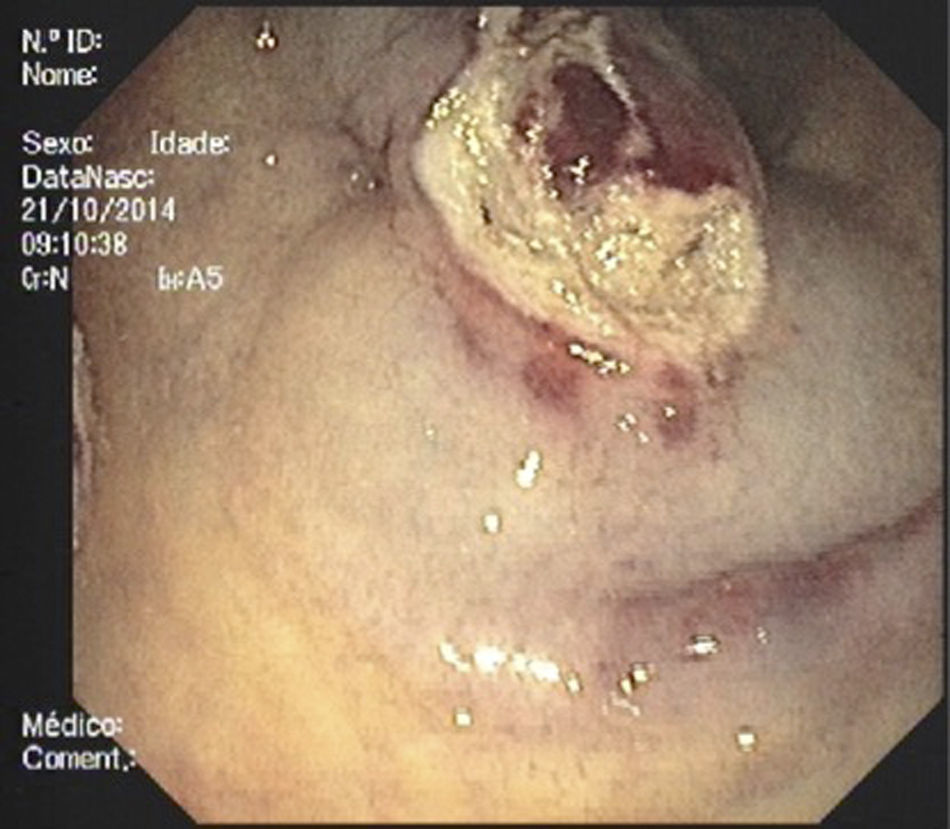
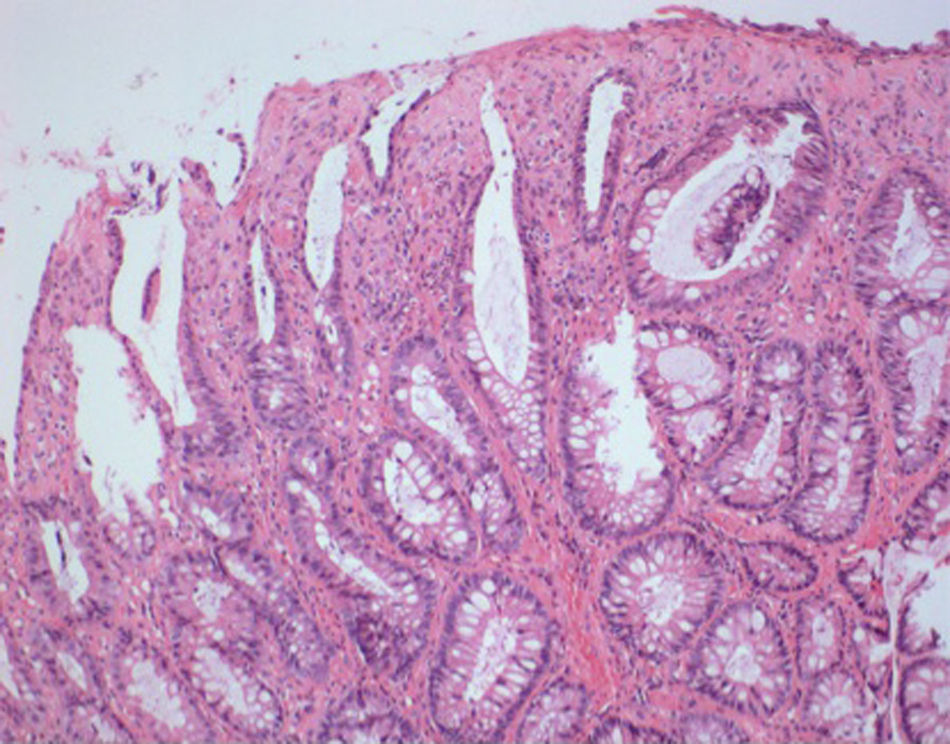
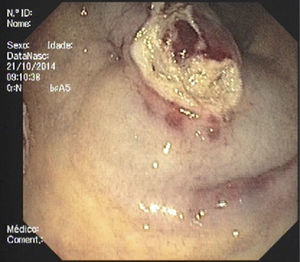
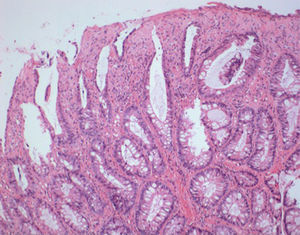
Due to the initial suspected malignancy and the absence of a definite diagnosis, endoscopic resection was decided after discussion with the patient. However, after submucosal injection with saline and epinephrine the lesion did not achieve adequate elevation. We then decided to perform a partial resection with diathermic snare to allow a more accurate histological diagnosis. After partial resection of the superficial part of the lesion extensive fibrosis was seen on the base of the lesion (Fig. 3). Histopathological evaluation of the resected specimen showed hyperplastic glands with polypoid configuration, epithelial denudation, dense fibrosis in lamina propria with polymorphic inflammatory infiltrate, dissociation of muscularis mucosae and vascular congestion (Fig. 4). The abovementioned findings – history of constipation, endoscopic findings of an inflammatory polypoid lesion with erosion and the presence of epithelial denudation, hyperplastic proliferation, dense lamina propria fibrosis and muscularis mucosae dissociation – allowed the definite diagnosis of mucosal prolapse polyp and the patient was advised to increase water and fiber intake and avoid straining. Constipation improved without the need of laxatives and there were no more episodes of hematochezia. Follow-up colonoscopy performed six months after resection showed maintenance of the lesion with the same characteristics except for reduced dimension.
The differential diagnosis of masses in the anorrectum includes adenomas, adenocarcinomas, mucosal prolapse polyps, fibroblastic polyps, juvenile polyps, hamartomas, inflammatory fibroid polyps, mucosal ganglioneuromas and leiomyomas of the muscularis mucosae.
Mucosal prolapse is the common underlying pathogenic mechanism of rectal prolapse, solitary rectal ulcer syndrome (SRUS), proctitis cystica profunda, inflammatory cap polyps, inflammatory cloacogenic polyps and inflammatory myoglandular polyps and it was proposed that these entities should be grouped under the term of “mucosal prolapse syndrome”.3–5 Mucosal prolapse can thus manifest as ulcerated lesions, flat erythematous mucosa or polypoid lesions. Polypoid lesions part of mucosal prolapse syndrome (inflammatory cap polyps, inflammatory cloacogenic polyps, myoglandular polyps and mucosal prolapse polyps) have been described with different names, although they share common endoscopic and histological features, raising the unsolved question if they are the same lesions with different denominations or if they are truly independent entities. Indeed, a common physiopathology (association with constipation and spastic contraction of bowel wall leading to congestion, prolapse and inflammation) and common histological findings of fibromuscular obliteration, glandular crypt abnormalities, thickening or dissociation of muscularis mucosae and dilation of glands have been found to overlap in these entities.6 However, mucosal prolapse polyps may mimic adenomas and even adenocarcinomas, both endoscopically and histologically.7
Thus, history, endoscopic findings and careful histopathological evaluation of the polyps are all important in the diagnosis of mucosal prolapse polyps in order to establish a confident diagnosis and rule out neoplastic changes, since it is important in the management and surveillance strategy. MPP are typically found in the 4th to 6th decades of life with male preponderance (3:1).5 Most of the times single, multiple rectal prolapse polyps have also been described in patients with mucosal prolapse syndrome.3,5,8
Clinically, almost all the patients have defecatory disorders associated with constipation, excessive straining, incomplete evacuation or rectal digitation. These disorders generally present with rectal bleeding, abdominal pain and constipation. The etiology of mucosal prolapse polyps is unknown although it is postulated that spastic contraction of the bowel wall lead to redundancy, passive venous congestion and obstruction.9 Endoscopically, mucosal prolapse often appears as bright red hyperemic mucosa that can be sessile, pedunculated or broad-based.10 Despite endoscopic appearance by itself does not allow the diagnosis of mucosal prolapse polyps, the annual tree ring sign (concentric circular innominate grooves surrounding the lesion seen with chromoendoscopy) was recently described as a specific endoscopic feature of these polyps and may help in the distinction of prolapsed polyps and malignancy.11 EUS may also be of value in the diagnosis of prolapsing folds and when a subepithelial origin is suspected.12
Histologically, mucosal prolapse polyps are characterized by crypt distortion, branching and inflammatory alterations. Mucosal prolapse may lead to thickening and disruption of the muscularis mucosae and muscularisation of the lamina propria.13 Chronic inflammation with mild disruption of the normal crypt architecture (elongation, displacement and distortion of glands) and epithelial denudation/ulceration is also common.14 Hyperplastic and serrated changes, including crypt branching, hypermucinous appearance of the epithelium and regenerative hyperplastic changes such as high incidence of mucous cell proliferation and dilatation of glands are also characteristic.15 However, the presence of villiform epithelial hyperplasia and regenerative atypia may lead to difficulties in differentiating mucosal prolapse polyps and villous adenoma7 and misplaced glands with mucus lakes within the submucosa may simulate invasive adenocarcinoma and pose additional difficulties.14 Additionally, adenomatous foci were reported in patients with MPP but there were no firm conclusion as if these MPP represented adenomas with secondary prolapse changes or adenomatous changes produced by the mucosal prolapse and inflammation.16 Besides, since the diagnosis of sessile serrated adenomas (SSAs) is mainly based on crypt architecture and given that rectal mucosal prolapse causes distorted crypt architecture, MPP may also mimic hyperplastic polyps and serrated adenomas.14,16 In fact, a recent study found that 26.9% of originally diagnosed rectal SSAs were reclassified as MPP (hyperplastic polyps associated with prolapse) when strict diagnostic criteria for SSAs were applied.17 Small biopsies, fragmented or tangentially orientated specimens may contribute with additional difficulties in the distinction of SSAs and MPP.
In conclusion, the diagnosis of mucosal prolapse polyps may be challenging and misdiagnosis is common. It is important to be aware of this infrequent entity in the differential diagnosis of anorrectal masses and a definite diagnosis and exclusion of adenomatous foci is important and should be pursued in order to establish proper management. Even when dysplasia is absent in biopsies, resection or repeat biopsies may be prudent due to the focal presence of dysplasia.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.