Protein-calorie malnutrition is a transversal condition to all stages of chronic liver disease. Early recognition of micro or macronutrient deficiencies is essential, because the use of nutritional supplements reduces the risk of complications.
The diet of patients with chronic liver disease is based on a standard diet with supplements addition as necessary. Restrictions may be harmful and should be individualized. Treatment management should aim to maintain an adequate protein and caloric intake and to correct nutrient deficiencies.
The large majority of patients with grade I/II hepatic encephalopathy can tolerate a regular diet. Protein restriction can aggravate malnutrition and is not recommended, except in cases of hepatic encephalopathy unresponsive to optimized therapy.
A desnutrição calórico-proteica é transversal a todos os estadios da doença hepática crónica. A deteção precoce de deficiências de micro ou macronutrientes é essencial, pois a utilização de suplementos nutricionais reduz o risco de complicações.
A dieta dos doentes com doença hepática crónica baseia-se numa dieta geral com a adição de suplementos, conforme necessário. As restrições dietéticas podem ser prejudiciais e devem ser individualizadas. Os objetivos do tratamento passam por permitir a ingestão de uma quantidade adequada de proteínas e calorias, bem como, corrigir as deficiências nutricionais.
A grande maioria dos doentes com encefalopatia hepática grau I/II consegue tolerar uma dieta normal. A restrição proteica pode agravar a desnutrição e não é recomendada, exceto em casos de encefalopatia hepática que não respondam a uma terapêutica otimizada.
Protein-calorie malnutrition (PCM) is a transversal condition to all stages of chronic liver disease (CLD) and may be present in 65–90% of patients with advanced disease.1–3 Malnutrition develops at an early stage of liver disease and there is, almost, a direct relationship between the severity of liver disease and the degree of malnutrition.4,5
The presence of PCM is associated with an increased number of complications such as esophageal varices, hepatic encephalopathy (HE), hepatorenal syndrome, impaired liver function and regeneration capacity and increased surgical morbidity and mortality.6–11 Malnutrition is an independent predictor of mortality in patients with CLD.7,12–15
Patients suffering from cholestatic liver disease are more susceptible to calorie deficiency and have an increased risk of fat-soluble vitamin deficits.16 Also, patients with hepatocellular disease are more susceptible to protein deficiency.16 Cirrhotic patients have a higher risk of micronutrient deficiency. Early recognition of micro or macronutrient deficiencies is essential, because the use of nutritional supplements has been proved to be associated with a reduced risk of infection, in-hospital mortality and improved liver function. The screening of all patients with CLD identifies those at risk of preventable complications.17
In this review, we describe the available evidence in the literature, including the more recent published guidelines, on nutrition of the patients with chronic liver disease, addressing the strategies for the clinician to overcome some of the obstacles that prevent adequate nutrition delivery in this population.
2Etiology and pathophysiologyMultiple factors contribute to malnutrition in CLD, including anorexia, inefficient digestion/absorption, iatrogenic measures or impaired metabolism.4
Many patients with CLD have a decreased food intake, often due to HE and digestive symptoms such as anorexia, nausea, early satiety (sometimes related to micronutrients deficiencies, such as zinc or magnesium, that may cause dysgeusia), gastroparesis, ascites or increased leptin levels.5,18,19 Overly restrictive diets (often with sodium restriction), frequent paracentesis or even some drugs, such as diuretics and lactulose, can lead to nutritional deficiencies.19,20 Heavy alcohol intake may also lead to a decreased appetite.4 Cirrhotic patients may also have an impaired digestion/absorption, often caused by the presence of portal hypertension that promotes changes in the intestinal mucosa, like increased permeability, contributing to an increased loss of proteins (protein loss can also occur due to bleeding from ulcers or varices).21–23 The deficiency of biliary salts (particularly in cholestatic diseases) and advanced degrees of pancreatic insufficiency (particularly in alcoholic disease) can cause steatorrhea, decreasing the absorption of certain nutrients.4,5 Intestinal dysmotility and bacterial overgrowth may also lead to an impaired digestion/absorption.24
Several metabolic changes occur in CLD. The studies report contradictory results; some claim that up to 34% of patients have a Rest Energy Expenditure (REE) of 120% above the expected value,25 while in other studies, the patient's majority had a normal REE.4 There are also changes in nutrients metabolism. Up to 70% of cirrhotic patients have some degree of glucose intolerance or insulin resistance, and between 14 and 40% have type II Diabetes mellitus.26 Decreased levels of hepatic and muscle glycogen are also common, leading to reduced availability of glucose as energy substrate, which results in increased consumption of fats and proteins.27 The muscle is a major metabolic organ and has an essential role in the amino acids (AA) metabolism and in the elimination of nitrogenous products through the kidneys glutamine synthesis and gluconeogenesis.6,26 However, the process of gluconeogenesis leads to muscle destruction as a source of protein substrates.28 This increased muscle destruction eventually leads to a protein synthesis decrease and in its degradation, explaining part of the protein deficiency of these patients.4 Sarcopenia is the most common complication of cirrhosis (up to 60% of patients).4 HE is more frequent in malnourished individuals, and thus cirrhotic patients with sarcopenia have an increased risk of HE.4,29
In CLD there occurs a decrease in branched chain amino acids/aromatic amino acids (BCAA/AAA) ratio, as observed in sepsis or major trauma.26,30 During overnight fast, ketogenesis and gluconeogenesis are increased (lipids represent 75% of the calories expended during this period), causing an increased AA consumption by the muscles.4 This condition is also observed in healthy subjects after 3 days of fasting, but in cirrhosis, this process is accelerated.4
Pancreatic dysfunction, increased lipolysis, fatty acids oxidation and ketogenesis lead to a reduction of plasma triglycerides, phospholipids, cholesterol, apoproteins and polyunsaturated fatty acids.4,31 This decrease is proportional to the severity of the liver disease and the degree of malnutrition, and is associated with decreased survival and is considered an independent predictor of mortality in alcoholic cirrhosis.4,31
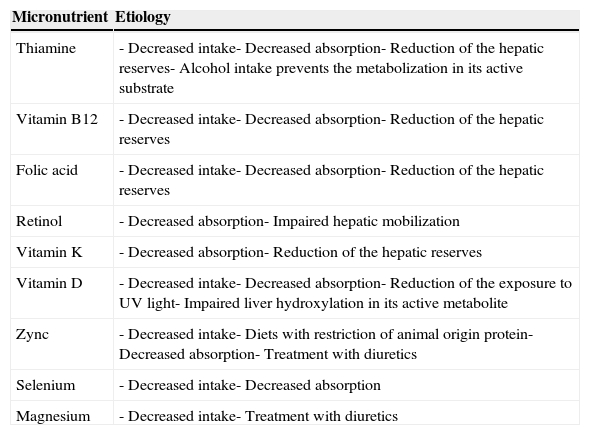
Micronutrient deficits are prevalent as well (Table 1). Deficiency of water-soluble vitamins, especially group B vitamins, is common in cirrhosis, particularly in alcoholic disease.32,33 Deficiency of fat-soluble vitamins has been reported in alcoholic disease, in the presence of steatorrhea associated with cholestasis and in the bile salt deficiency.34,35
Main micronutrient deficits in chronic liver disease and its etiologic contributing factors.
| Micronutrient | Etiology |
|---|---|
| Thiamine | - Decreased intake- Decreased absorption- Reduction of the hepatic reserves- Alcohol intake prevents the metabolization in its active substrate |
| Vitamin B12 | - Decreased intake- Decreased absorption- Reduction of the hepatic reserves |
| Folic acid | - Decreased intake- Decreased absorption- Reduction of the hepatic reserves |
| Retinol | - Decreased absorption- Impaired hepatic mobilization |
| Vitamin K | - Decreased absorption- Reduction of the hepatic reserves |
| Vitamin D | - Decreased intake- Decreased absorption- Reduction of the exposure to UV light- Impaired liver hydroxylation in its active metabolite |
| Zync | - Decreased intake- Diets with restriction of animal origin protein- Decreased absorption- Treatment with diuretics |
| Selenium | - Decreased intake- Decreased absorption |
| Magnesium | - Decreased intake- Treatment with diuretics |
Thiamine deficiency is quite common, and is not exclusive of alcoholic disease. Decreased intake, absorption and hepatic reserves may contribute to it. Alcohol intake also reduces intestinal absorption of thiamine and prevents metabolization in its active substrate. Thiamine deficiency may lead to Wernicke encephalopathy and Korsakoff dementia.36
Vitamin B12 deficiency is mainly related to the decrease of its liver reserves. Serum levels may be increased, but tissue levels are decreased.26 This deficiency is associated with anemia, glossitis and neurological symptoms. Folic acid deficiency develops faster in cirrhotic patients due to decreased hepatic storage levels.29
Retinol deficiency is related with decreased absorption and impaired hepatic mobilization.37 It can cause dermatitis, night blindness or photophobia and increased risk of neoplastic disorders, including hepatocellular carcinoma. A retrospective study reported that the majority of liver disease patients being considered for liver transplantation present with vitamin A and D deficiencies.38 Because high doses of vitamin A are potentially hepatotoxic, care must be taken to avoid excessive supplementation.11
Vitamin K deficiency is caused by decreased liver storage levels and is associated with increased risk of bleeding.4
Vitamin D deficiency results from ingest reduction, decreased absorption (due to cholestatic disease or portal hypertension enteropathy) and reduction of exposure to UV light. Since vitamin D is hydroxylated in the liver to produce calcidiol, patients with severe parenchymal or obstructive hepatic disease may have reduced production of this metabolite.39,40 The majority of the liver must be dysfunctional before calcidiol synthesis is reduced. Thus, these patients rarely manifest biochemical or histological evidence of osteomalacia, unless concomitant nutritional deficiency or interruption of the enterohepatic circulation occurs.39,40 Extremely low serum levels of vitamin D are associated with increased mortality in patients with chronic liver disease.41
Zinc and selenium deficiency have been described in patients with alcoholic and non-alcoholic liver disease.42–44 Zinc deficiency is caused by intake reduction (to which contributes a diet with restriction of animal origin protein), impaired intestinal absorption and treatment with diuretics.45–47 This deficiency may increase ammonia levels in circulation, increasing the risk of HE and may also induce anorexia, dysfunction of the immune system and dysgeusia, which further decreases its intake.48–52
Alcohol consumption may also cause folate and magnesium deficiency.53 It has been demonstrated that alcohol impairs magnesium transport and homeostasis in brain, skeletal muscle, heart and liver.11
3Nutritional status assessmentThe diagnosis of malnutrition can be challenging in the early stages of cirrhosis.54 There is no consensus about the best method for quantification and classification of malnutrition and the cost-effectiveness of evaluating all patients is not established.4
The dietary record is a simple tool and probably the best method available to recognize all data related to food intake.4 The Subjective Global Assessment (SGA) scale, which includes elements of the clinical history and physical examination (weight, food intake, gastrointestinal symptoms, functional capacity, nutritional requirements, metabolic requirements and physical examination), is validated for the assessment of nutritional status in cirrhotic patients and may provide prognostic information.55–57
Biochemical parameters such as albumin, pre-albumin and retinol binding protein are affected by hepatic dysfunction, which makes its use unreliable in these patients.5,58 The serum total proteins relate better with liver disease severity than with the level of malnutrition.59 Immunological parameters such as lymphocytes levels, hypersensitivity skin test or complement levels have low sensitivity and specificity.27 The creatinine/height index is a reliable method if the patient's renal function is normal.60
Anthropometric parameters, including weight and Body Mass Index (BMI), are altered by electrolyte disturbances, renal failure and the presence of edema or ascites and therefore have low sensitivity and reliability in these patients.4,61 Measuring skinfold thickness (tricep, bicep and subscapular) is less affected by hydropic changes (although it may be affected by the presence of edema, which only affect upper extremities in rare cases) and it is considered one of the best methods for indirect assessment.4 However, this method has low inter-observer reproducibility, which makes it not useful for follow-up.18,54
Bioimpedance (BIA) is a non-invasive, safe, easy to perform and relatively inexpensive and sensitive method that may provide prognostic information.4,62 However, it has some limitations in patients with electrolyte disturbances. Although it is a useful method in the evaluation of patients with ascites, it is more sensitive in its absence.4
Dynamometry (hand-grip strength) is one of the most sensitive methods.5 It is very useful in patients follow-up and can also predict complications. However, the method is less available and may overestimate malnutrition severity.
Indirect calorimetry can determine patient REE through the Weir equation, by measuring oxygen consumption and carbon dioxide production.25,63 Measured REE by BIA is compared to the predicted REE, according to the Harris-Benedict equation.5 The patient is generally considered hypermetabolic if the measured REE is 10–20% higher than expected.25,64 However, this method is expensive and available only in a limited number of centers. REE on ascites may increase up to 10%.25,65,66 So, commonly only the estimated REE is determined. In the absence of ascites, current body weight can be used to estimate REE; however, in its presence, the ideal weight should be used.67
There are still other methods, although less used, such as the amount of body potassium, IVNAA (Neutron Activation Analysis), DEXA (Dual Energy X-ray Absorptiometry), isotope dilution or the creatinine level in 24h urine. Some of these, such as the amount of body potassium or isotope dilution, are very accurate, but they virtually exist only as experimental methods.4,5
In this context, for reasons of sensitivity, specificity, cost or availability, there is no ideal method. Probably the best approach, which is recommended by the European Society for Clinical Nutrition and Metabolism (ESPEN), involves the use of multiparameter data.68 In the initial assessment, this society recommends the use of indirect methods such as SGA scale or anthropometry, because they are affordable, adequate and able to identify patients at risk of malnutrition.68 After the identification of malnourished patients, quantitative methods (such as BIA), that are more accurate, are recommended.68
Given the wide consensus that nutritional status should be routinely assessed in all patients with chronic liver disease in order to recognize malnutrition and prevent nutritional depletion, the development of a simple, well validated and reproducible tool for the assessment of nutritional status in these patients is long overdue.69
4TreatmentThe diet of patients with CLD is based on a standard diet with supplements addition as necessary.20 In fact, in most cases it is possible to give a practically normal diet.26 Restrictions may be harmful and should be individualized.4 The treatment goals are to improve the level of PCM, to ensure an adequate amount of nutrients, to achieve a positive nitrogen balance and to avoid hepatotoxic agents.5,69–71 Early correction of nutritional deficiencies improves long-term prognosis.72
Food should be well cooked, given the patient's increased susceptibility to infections, and should be distributed in 5–7 small daily meals in order to prevent protein overload and nausea/vomiting.4,26 Meal schedule may be more important than the amount of food ingested, because during the postprandial period there is a suppression of protein degradation in favor of synthesis stimulation. Increasing postprandial period can improve the patient's condition.73–76
A late evening snack has a positive effect on the nitrogen balance, increases muscle mass by reversing sarcopenia, can improve quality of life, reduce the severity and frequency of HE and increase survival.4,73,76,77 Thus, it is recommended to minimize overnight fasting period, in order to avoid fasting periods longer than 6h and reduce the catabolism rate.4,68 Although data on this topic is scarce, patient's compliance may be difficult because this late meal can worsen reflux complains, impair sleep quality and cause glucose intolerance.78
A late snack of at least 710kcal or 110g of carbohydrates increases lean mass, which was not demonstrated with a meal or 200kcal or 40g of carbohydrates.4,73 Although there is no consensus on the meal composition, foods with high caloric content (at least 50g of carbohydrates) and enriched with BCAA (leucine, isoleucine and valine) are preferred.4 If administered during the night, BCAA are preferably used in protein synthesis, while during daytime they are preferably used as energy.74 The normalization of serum BCAA levels promotes protein synthesis, reduces the concentration of nitrogenous products and prevents the formation of false neurotransmitters which may have a role in the development of HE.26
The use of BCAA-enriched formulae can improve the prognosis of patients with advanced cirrhosis.68 These supplements may reduce the progression of liver failure, improve quality of life, reduce the severity and frequency of HE and increase survival.4,68,79–82 However, some studies have failed to demonstrate these benefits and further data are lacking to clarify their long-term effects. In this context, ESPEN does not recommend its regular use, given the higher cost and oral intolerance, recommending, in general, a diet rich in whole protein formulae.68 The oral/digestive intolerance has been bypassed by the new formulations with new supplement flavors, but the high cost still prevents a broader use.4,83
In patients with compensated cirrhosis without malnutrition, the ingestion of 1.2–1.5g/kg(weight) daily protein is recommended.63 In malnourished patients, 1.0–1.8g/kg(weight) is recommended, depending on the severity of malnutrition and liver disease.11 Protein needs are higher in malnourished patients and in stress situations (such as bleeding, infection or surgery), provided that there is no renal dysfunction (in which may be necessary a protein restriction).
In patients with ascites, more concentrated high-energy formulae should be preferred.68 Sodium restriction may be required in patients with ascites/edema. In patients unresponsive to diuretic therapy, the amount of sodium should be restricted to 2g/day.44 Fluid restriction should only be recommended in severe hyponatremia (Na+ <120mEq/mL) and is not indicated in compensated liver disease.4
Carbohydrates are the base of the diet of cirrhotic patients and should cover 50–60% of non-proteic daily needs.44,67 An infusion of glucose (2–3g/kg(weight)/day) should be initiated when patients have to abstain from food for more than 12h.67 Diet should tend to be hypercaloric and foods rich in complex carbohydrates should be preferred.26,84 Lipids should cover the remaining non-proteic daily needs.67 Adjustments should be performed in the presence of steatorrhea.11
An energy content of 35–40kcal/kg(weight)/day is usually sufficient to restore/maintain nutritional status and enhance liver regeneration.11,68 Whenever possible, they should be provided an energy content to cover 1.3×REE.67 However, caloric excess must be avoided due to harmful effects of lipogenesis, which can cause liver dysfunction.6
The number of patients with cirrhosis who are overweight or obese has increased in recent years.69,10 These patients may be malnourished, despite the increase in their overall body weight. There is no information on energy or protein requirements in this patient population, and thus, generic recommendations should be applied.69 Weight loss should be encouraged in patients with well-compensated cirrhosis who are overweight, by carefully monitored and proportionate reductions in both total energy and protein intakes, together with an increase in physical activity.69 In patients with decompensated cirrhosis, attempts to reduce body weight should be very carefully monitored. These may be accomplished by reducing the carbohydrate and fat content of the diet, while maintaining the protein intake.69
In patients with preserved oral intake, there is little consensus regarding the empirical use of multivitamin or other micronutrient supplements vs cost-effectiveness of evaluation of nutritional deficiencies and for providing these supplements as necessary. ESPEN suggests that empirical daily supplementation should be considered to all patients.68 Whichever approach is chosen, there are some considerations to be kept in mind. Thiamine supplementation may be considered in all patients, especially in those who have alcoholic disease.22 In cholestatic disease, fat-soluble vitamins supplementation should be considered.22 Vitamin K supplementation should be considered only in situations of high hemorrhagic risk.85 The supplementation of zinc and magnesium can indirectly enhance food intake and nutritional status improving dysgeusia.86,87 Some authors propose supplementation with calcium (1–1.2g/day) and vitamin D (400–800UI/day), especially in cholestatic disease and in patients with osteopenia.67,85
In cirrhotic patients who cannot meet their nutritional requirements from normal food despite adequate individualized nutritional counseling, ESPEN recommend starting enteral nutrition (EN) in order to prevent progression of malnutrition.68
In severely undernourished patients with advanced liver cirrhosis, supplemental enteral nutrition, in addition to normal food ad libitum, is of documented value; however, in less severe cases, it seems not to be more effective than normal diet under dietary counseling.67,68,72,88,89 EN improves the nutritional status of cirrhotic patients, reduces complications and improves their survival.68
EN should be initiated as soon as possible (first 24–48h) in patients unable to ingest a minimum of 1g/kg(weight) (>50g) daily proteins.44,90 Oral supplementation is the first EN option, initially only during night period and, if necessary, also during daytime.68 Tube feeding is the second option of EN and may improve nutritional status, liver function, reduce complications and increase survival.68
Concerns about the potencial bleeding risk from nasogastric tube placement are not supported by the current literature.67 Fine bore nasogastric tubes are safe even in patients with esophageal varices,68 but their use should be postponed at least 24h after endoscopic treatment.20
The use of PEG/PEJ is associated with a higher risk of complications (due to ascites or varices) and is not recommended.68
Parenteral nutrition (PN) is a second choice in relation to EN, but should be initiated if the patient cannot be fed orally or enterally.67 This can occur in cases of severe HE (III/IV) and in the absence of cough reflex or impaired swallowing.67 In the presence of sleepiness or psychomotor dysfunction, oral intake may be insufficient even in less severe stages of HE.91 PN should also be considered in cases of nonfunctioning gastrointestinal tract, intestinal obstruction, unprotected airway, intolerance to enteral feeding or if a fasting period exceeding 72h is expected.67
In patients with transjugular intrahepatic portosystemic shunt (TIPS), EN may be harmful, due to higher risk of hyperammonemia, and PN is preferred.44,92
The greatest risk of infection of PN versus the risk of aspiration of EN should always be considered. When PN is initiated, supplements of fat and hydrosoluble vitamins should be added.67 Recently, some authors suggested the supplementation with high doses of thiamine (250mg/day, prophylactic dose) in alcoholic patients.36 Thiamine supplementation should be initiated prior to an infusion of glucose, to reduce the risk of Wernicke encephalopathy.67 Other micronutrients should also be initiated. A zinc supplementation with twice the usual daily requirement (2×5mg/day) is recommended.67
A pragmatic approach, recommended by ESPEN, is the liberal supplementation during the first two weeks of nutritional support, because the evaluation of each micronutrient deficiency would have higher costs and delays the replacement.67
In patients with steatorrhea, the diet content of long chain fatty acids must be reduced at the expense of medium and short chain fatty acids.20,26 Some patients, such as those with alcoholic disease, may require supplemental pancreatic enzymes due to the presence of pancreatic insufficiency.20
5Therapeutic considerations in hepatic encephalopathyThe large majority of patients with grade I/II HE can tolerate a regular diet. An energy content of 30–35kcal/kg(weight)/day, similar to the patient without HE, should be provided to this patients, according to the American Society for Parental & Enteral Nutrition (ASPEN).44 The recommended protein content is 1–1.5g/kg(weight)/day.44 However, the International Society for Hepatic Encephalopathy and Nitrogen metabolism (ISHEN) recommends the same energy (35–40kcal/kg(weight)/day) and protein contents (1.2–1.5g/kg(weight)/day) as those that are recommended for patients without HE.69 Carbohydrates are the mainstay of the diet and should constitute 50–60% of all nutrients. Lipids should provide 10–20% and proteins 20–30% of the remaining nutrients.44 The diet should be divided over 4–6 small meals per day (including a carbohydrates-enriched meal), according to the ability of each patient in chewing and swallowing.44
In cirrhotic patients with HE, contrary to what has been advocated in the past, protein restriction is not recommended, since most patients present with an advanced protein-calorie deficit.12,44 A maintained negative nitrogen balance through protein restriction leads to an increase in PCM and cachexia.6,92,93 Several recent studies have demonstrated the importance of maintaining a positive balance of nitrogen products.
Protein restriction can aggravate malnutrition leading to an increased muscle breakdown, and release of amino acids with a consequent increase of ammonia levels, worsening the prognosis of HE.10,94 Even transient protein restriction does not have any proven benefit during an episode of HE.68 In cases of severe protein intolerance in HE unresponsive to optimized therapy (control of precipitating factors, lactulose, rifaximin),20,44 a transitional restriction (0.8g/kg/d) can be attempted for the shortest time possible (less than 48h); and normal protein intake should be resumed as soon as possible.6 Other possible exceptions are the patients with gastrointestinal bleeding, in whom a protein restriction, for very short periods, may be necessary while they are being stabilized.69 An alternative approach for initial intolerance would be a gradually increase of the protein dosage.4,6 Paradoxically, the protein excess can induce HE, for so, the treatment must always be individualized.
The ISHEN recommends that patients with recurrent or persistent HE should take a diet richer in vegetable and dairy protein than meat and fish protein.69 Also, the ASPEN suggests an increase in the content of milk or vegetable protein origin and BCAA-enriched supplements in patients with protein intolerance.26,44 Studies showed that dairy protein is better tolerated than protein from mixed sources and that vegetable protein is better tolerated than meat protein.69 The proteins of vegetable and dairy origin may improve the nitrogen balance and, if well tolerated by the patients, they may be provided without constraints.44,95,96 The vegetable proteins are better tolerated than those of animal origin, and they may influence intestinal transit, have a higher content of fiber and BCAA and a lower content of AAA.95,96
The ISHEN recommends that the daily ingestion of diets containing 25–45g of fiber should be encouraged, due to its ability to eliminate the nitrogen products of the colon and to reduce the degree of the patient constipation.4,29,69
Some studies have shown that patients with grade III/IV HE benefit from a diet rich in BCAAs and low in AAA.67,97 The use of oral BCAA supplements, in daily divided doses, may facilitate the provision of an adequate nitrogen intake in the occasional patient who is truly protein intolerant.98 The greatest consensus for use of BCAA-enriched supplements is in patients with HE unresponsive to standard treatment and in the presence of protein intolerance.68 These supplements improve HE, particularly if administered in chronic cases.99 There is evidence that BCAA-enriched supplements may improve clinical outcome when prescribed to patients with an established nutritional deficit68,80,100 and there are no studies suggesting that their use is harmful to HE.26
Probiotics may reduce ammonia levels through its influence on intestinal transit. Although its use is not consensual and recent systematic reviews of the use of probiotics to treat HE have not been as encouraging, some studies suggest that they may improve the HE severity, liver function and reduce the number of infections.69,100 Another strong argument for its use is that these adjuvants have virtually no side effects.29 The yogurt may be a useful food in HE, because they are rich in lactose and milk proteins and have a natural bacterial content.92,95
Vitamin status is not easily assessed; multivitamin supplementation is cheap and generally free of side effects. Thus, use of oral vitamin supplements could be justified in patients admitted with decompensated cirrhosis.69
The zinc and selenium deficiency is very common in the advanced stages of cirrhosis. Its supplementation was associated with an improvement of the metabolism of amino acids and HE.48,101,102 Although ASPEN recommends its empirical supplementation, studies on the HE improvement with zinc supplements are controversial and there is no consensus on the optimal dosage.20,26,44,48,49,103,104
Total body manganese stores are increased in patients with liver disease, which may lead to selective manganese accumulation in several areas of the brain.11 Manganese deposition in basal ganglia structures of the brain has been proposed as the cause of cirrhosis related Parkinsonism.11,105 Long-term treatment with manganese containing nutritional formulations should be avoided.69
There are no randomized studies comparing enteral vs parenteral nutrition in patients with HE; however, parenteral nutrition should be considered in severe case (HE grade III/IV).67
6ConclusionsNutritional deficiencies in chronic liver diseases are very prevalent and are associated with compromised outcomes in this population. The cause of malnutrition in patients with cirrhosis is multifactorial, and includes anorexia, inefficient digestion/absorption and impaired metabolism.
The diagnosis of malnutrition can be challenging in the early stages of cirrhosis. Although there is no consensus about the best method for quantification of malnutrition, probably, the best approach involves the use of multiparameter data, using the SGA scale or anthropometry in the initial assessment in order to identify the patients at risk of malnutrition. After the identification of malnourished patients, BIA may be used in order to provide prognostic information.
Most patients with CLD can have a practically normal diet with supplements addition as necessary. Restrictions may be harmful and should be individualized. Treatment management should be based on maintaining adequate protein and caloric intake and correct nutrient deficiencies. The consumption of frequent small meals and a late evening snack can reduce protein breakdown. A maintained negative nitrogen balance through protein restriction leads to an increase in PCM and should be prevented. Protein restriction can aggravate malnutrition and is not necessary except in cases of HE unresponsive to optimized therapy.
Efforts to improve the nutritional status of patients with cirrhosis are warranted, preferably through EN or, when necessary, by PN. Enteral feedings are a safe and effective way to provide increased nutrition when a patient is unable to meet their basic needs by oral intake. The use of BCAA-enriched formulae remains controversial, but the most recent data promote their therapeutic potential in patients with advanced cirrhosis.
Malnutrition is a potentially reversible condition that, when identified and treated appropriately, can lead to improvement of the outcomes of patients with CLD.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interest and source of fundingNone declared.