Pancreatic panniculitis is a rare skin disorder that occurs in 2–3% of pancreatic diseases, mostly associated with acute or chronic pancreatitis. Its pathophysiology is still unclear, but the release of pancreatic enzymes in circulation can be responsible for this disorder. The typical histological features are adipocyte necrosis with neutrophils infiltrate and typical “ghost cells”. Its treatment, clinical course and prognosis are usually related with the pancreatic disease.
We present a case of a 39-year-old man who presented with fever, abdominal pain, nausea and vomiting after a copious alcohol ingestion. Acute alcohol-induced pancreatitis was diagnosed. 9 days after admission he developed tender erythematous subcutaneous nodules, whose biopsy was consistent with pancreatic panniculitis. There was clinical and laboratory improvement with supportive treatment as well as skin nodules regression.
Although pancreatic panniculitis is a rare condition, physicians must be aware of it to avoid delay in the diagnosis.
A paniculite pancreática é uma condição cutânea rara que ocorre em 2–3% das doenças pancreáticas, estando sobretudo associada às pancreatites aguda e crónica. A sua fisiopatologia ainda é incerta, mas a libertação de enzimas pancreáticas na circulação parece estar implicada. Os aspectos histológicos característicos consistem em necrose dos adipócitos com infiltrado neutrofílico e as típicas “ghost cells”. O seu tratamento, evolução clínica e prognóstico estão habitualmente relacionados com a doença pancreática.
Apresentamos o caso de um homem de 39 anos com um quadro de febre, dor abdominal, náuseas e vómitos após uma ingestão copiosa de álcool. Foi diagnosticada uma pancreatite aguda alcoólica. 9 dias após a admissão, surgiram nódulos eritematosos subcutâneos dolorosos, cuja biópsia foi consistente com paniculite pancreática. Houve melhoria clinica e laboratorial com o tratamento de suporte, assim como regressão dos nódulos cutâneos.
Embora a paniculite pancreática seja uma condição rara, os médicos devem tê-la presente para evitar o atraso no diagnóstico.
Pancreatic panniculitis is a rare skin disorder, first described in 1883 by Chiari,1 associated with pancreatic diseases, mainly acute or chronic pancreatitis, but association with pancreatic carcinomas may also occur. Other pancreatic conditions (post-traumatic pancreatitis, pancreatic pseudocyst, pancreas divisum, and hemophagocytic syndrome) may be associated with panniculitis, however they are less frequent.2 It appears in 2–3% of pancreatic diseases,2,3 and it does not correlate with severity of the underlying condition. It may precede other symptoms of pancreatic disorder in 40% of the cases.4–6 The lesions frequently occur in the lower limbs, but they may also appear in the arms, chest, abdomen, buttocks and scalp.6
It appears as subcutaneous, purple-red tender nodules, which histology reveals adipocytes necrosis. Sometimes these nodules present spontaneous ulceration with the release of lipid derivatives from fat necrosis.6
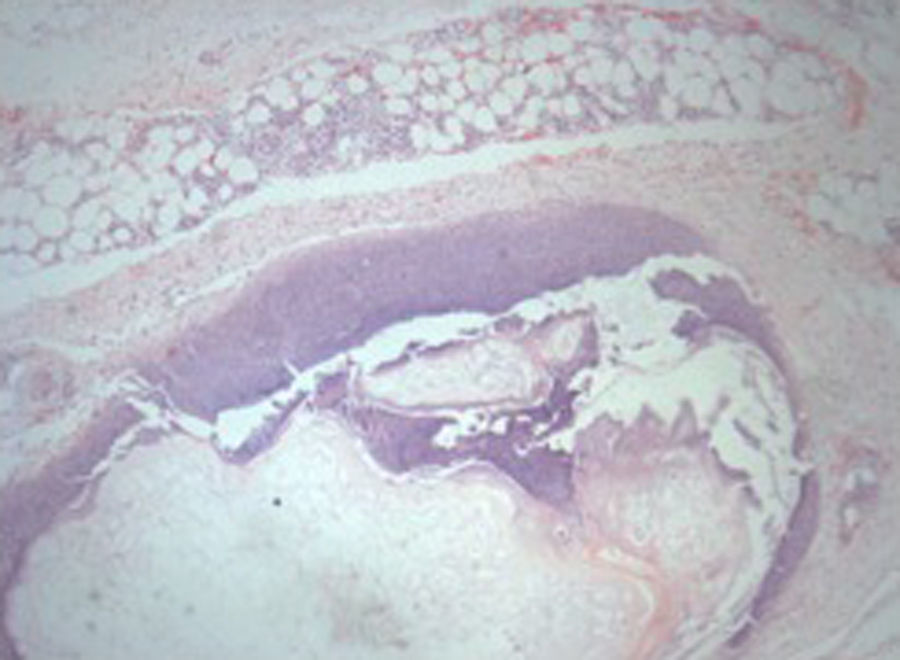
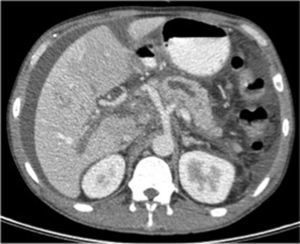
2Case reportA 39-year-old Chinese man presented to the emergency department with acute abdominal pain, fever, nausea and vomiting; he referred an abusive alcohol consumption in the previous day; he had no relevant medical history; no medication or other drug use were reported. On physical examination he was febrile (38.3°C), tachycardic (118bpm), is blood pressure was 127/84mmHg, he was dehydrated, his cardiac and thoracic examination were normal; in abdominal examination he had epigastric tenderness, with no masses or organ enlargement. He had no skin lesions at that time. An acute alcohol-induced pancreatitis was suspected and the blood tests confirmed elevation of serum amylase and lipase (1731U/L/3148U/L, respectively), leukocytosis (13,400/L) with neutrophilia (81%), elevation of C-reactive protein (200mg/L), and gamma glutamyltransferase (197U/L). Liver transaminase levels were normal. An abdominal CT-scan was performed and it showed a pancreatic diffuse enlargement, with peri-pancreatic fat tissue densification; mild peri-hepatic ascites; there was no suggestion of pseudocyst or abscess (Fig. 1).
According to the Atlanta classification, the patient presented a mild acute pancreatitis, with no organ failure. He was admitted to the internal medicine department and intravenous hydration and analgesia was performed with symptom improvement. Besides that, he maintained elevated pancreatic enzymes. At 9th day he presented multiple erythematous tender nodules mainly in the legs, but also in the right arm; they had 0.5–2cm diameter and there was no ulceration or exudate (Fig. 2).
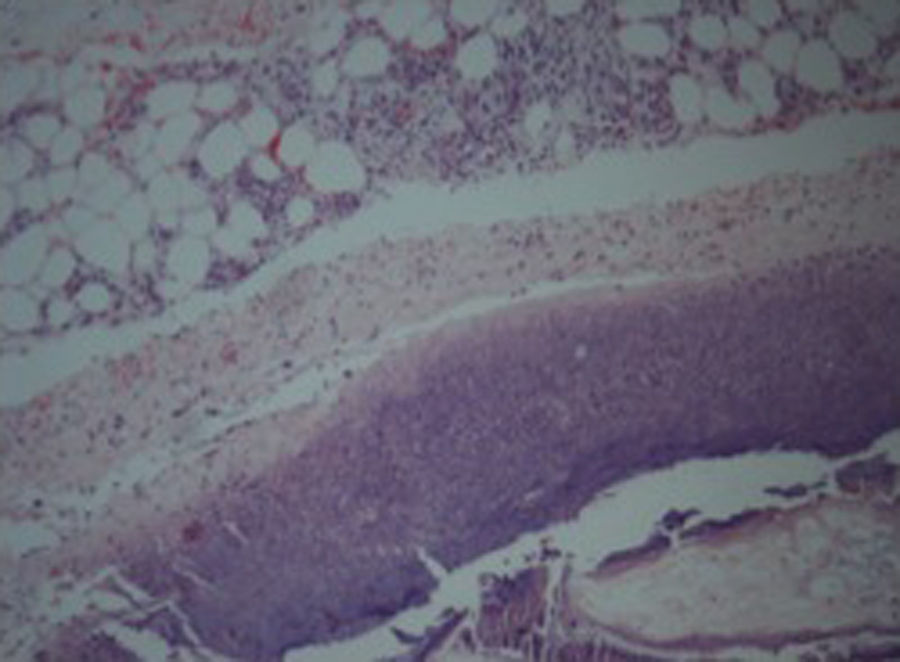
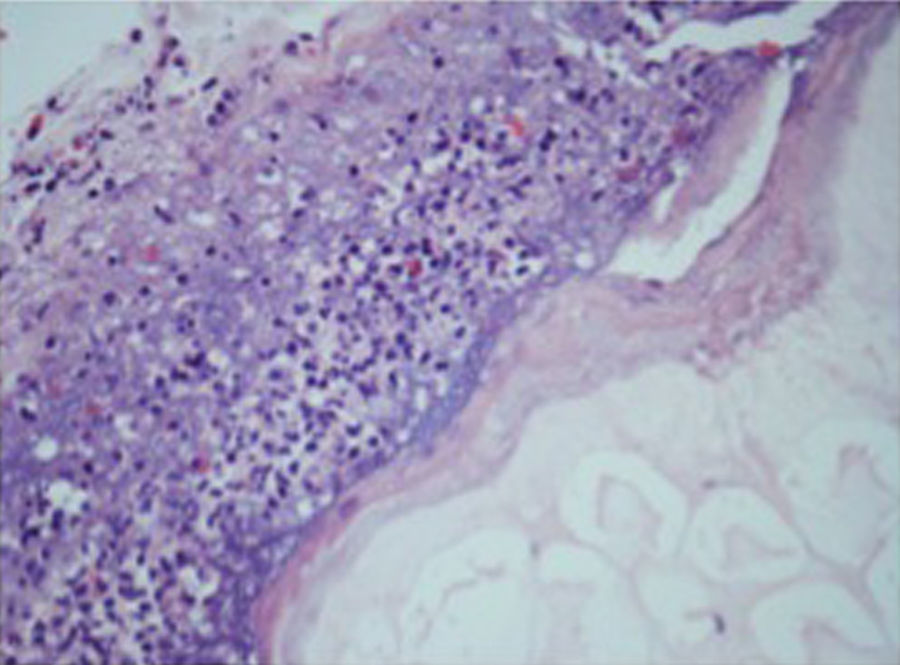
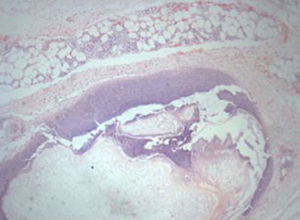
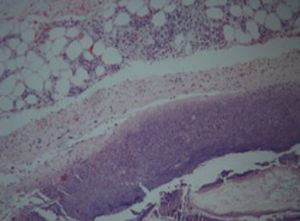
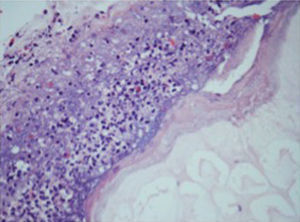
An incisional nodule biopsy was performed and it revealed “skin fragment with lobular panniculitis, with a steatonecrosis central area surrounded by neutrophils and cell degradation products – consistent with pancreatic panniculitis” (Figs. 3–5)
The diagnosis of pancreatic panniculitis was established. Supportive treatment was maintained and there was regression of subcutaneous nodules in five days. Brown skin scars were still visible when the patient was discharged, 21 days after admission.
3DiscussionPanniculitis is an inflammatory cutaneous disorder involving the adipose lobules of subcutaneous tissues. It can be associated with either inflammatory or infectious diseases7,8 and its clinical presentation may be challenging to physicians once there are clinical similarities between different kinds of panniculitis.8
Pancreatic panniculitis has extended necrotic areas, affecting mainly the adipose lobules and it has neutrophils predominance in the inflammatory infiltrate, without vasculitis.8,9 Its pathophysiology remains unclear, but the release of pancreatic enzymes, such as trypsin, amylase and lipase seems to be involved in the process.3,5 Trypsin may increase microcirculation permeability, allowing lipase and amylase to penetrate in fatty tissue and hydrolase the lipids, causing necrosis and inflammation. However, on the one hand this skin condition is only rarely associated with pancreatic diseases and, on the other hand, there are reports of pancreatic panniculitis associated with normal serum amylasemia and lipasemia, postulating that some other factors could also determine this clinical manifestation.2,3,9
In the early stages of the disease the “ghost adipocytes” – anucleate necrotic cells resulting from saponification of lipids followed by calcium deposition – may be present and they are pathognomonic. They result from the action of pancreatic enzymes in the subcutaneous fatty tissue.
Pancreatic panniculitis may precede the development of pancreatic disease,10 and its prognosis is related with the underlying pancreatic condition. Treatment is supportive and should be directed to the pancreatic disease.6
In some cases there may be joint manifestations of arthritis or arthralgia associated with that cutaneous disorder, however not much is known about its pathogenesis.11
Our patient first presented with common clinical and laboratory features of acute alcohol-induced pancreatitis. However, during the course of the disease, some tender erythematous nodules appeared in lower extremities and arm which histology revealed adipocyte necrosis and the diagnosis of pancreatic panniculitis was established; supportive treatment of the underlying pancreatic condition allowed resolution of cutaneous lesions.
4ConclusionPancreatic panniculitis is a rare condition, only present in 2–3% of pancreatic disorders. As far as we know, there are only two cases reported in portuguese literature. In the case of our patient the diagnosis of acute pancreatitis was first established; however, this skin condition may precede other pancreatic related symptoms, so awareness of the relationship between this entities is important to avoid delay in establishing correct diagnosis and treatment.
Conflicts of interestThe authors have no conflicts of interest to declare.