We present a case report of a 78-year-old man that was admitted in our Intensive Care Unit after an urgent surgical repair of a stent-grafting endoleak and an aortobronchial fistula. Five years before this event, he had been submitted to a thoracic endovascular repair of a descending thoracic aorta aneurysm.
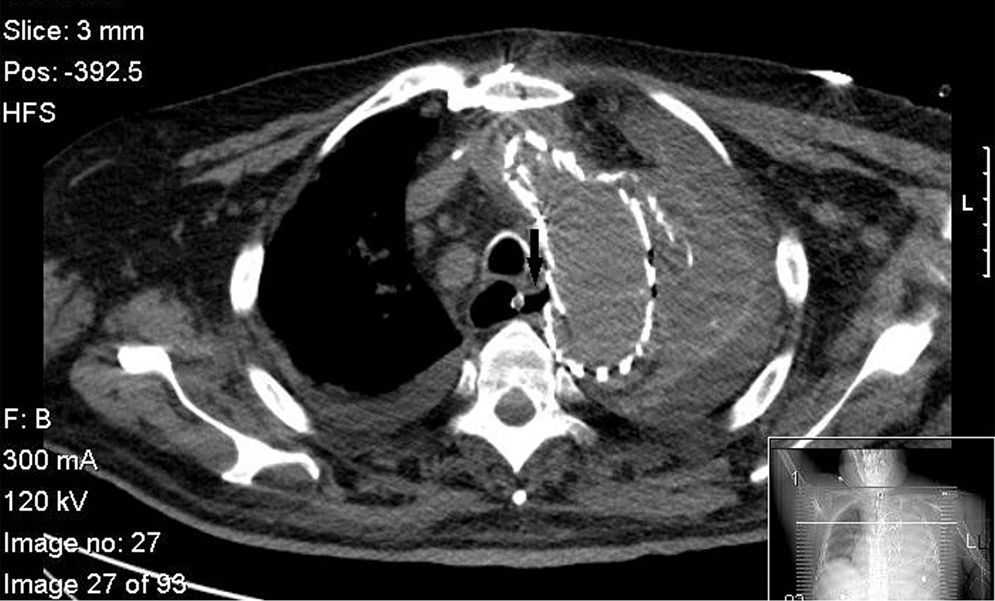
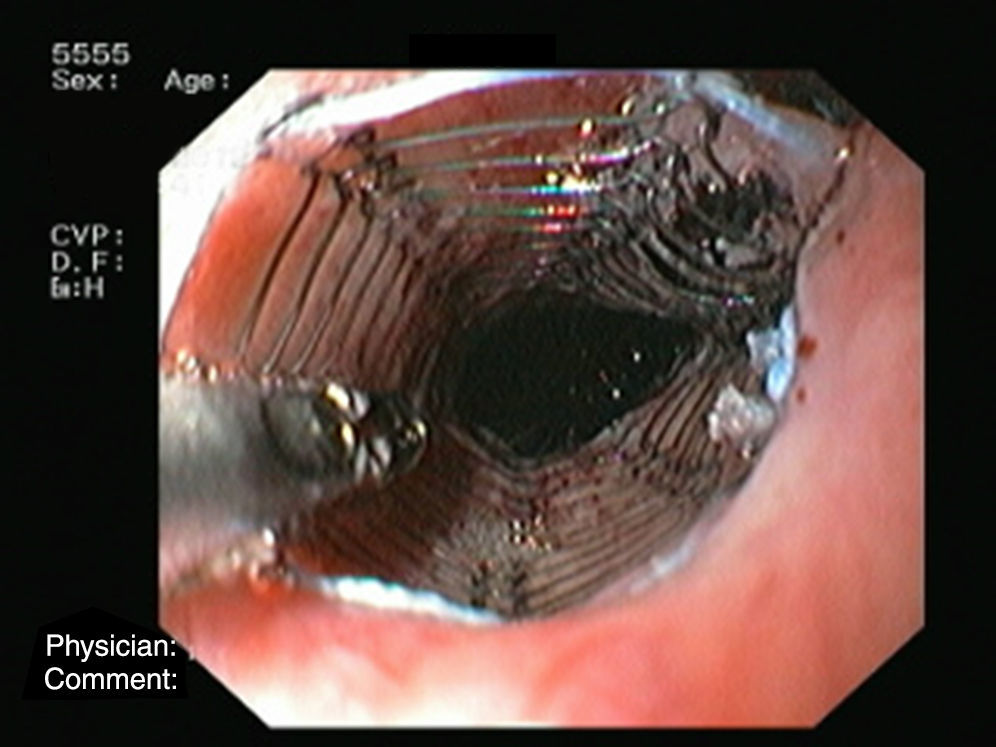
The immediate post-operative course was uneventful. Four days after surgery, the patient developed acute renal failure, elevated inflammatory markers, bacteremia and refractory shock, although he was under therapy with broad-spectrum antibiotics and there was no evidence of bleeding. A CT-scan revealed a thickened esophageal wall and small gas bubbles near the aortic stent graft suggesting an aortoesophageal fistula (Fig. 1). He was referred to our department for upper endoscopy and a fistula on the posterior surface of the middle third of the esophagus was recognized, through which the aortic stent was observed (Fig. 2). With the diagnosis of an aortoesophageal fistula secondary to the previous thoracic endovascular repair technique, esophageal stenting with a covered self-expanding esophageal stent with Ultraflex Esophageal NG 23×100mm (Boston Scientific®, United States) was performed to help local infection control (Fig. 3). The medical treatment was optimized with intravenous proton pump inhibitors and parenteral nutrition, maintaining broad-spectrum antibiotics. In the next three weeks, no signs of hemorrhage or infection were noticed. The patient recovered from shock, with subsequent suspension of amines and ventilator support. Despite this clinical improvement, the patient died unexpectedly a few days before his scheduled surgery. The autopsy identified rupture of the aortic arch.
Aortoesophageal fistula is a catastrophic complication of thoracic endovascular repair techniques with a reported incidence of 1.5%.1 Despite being the most frequent symptom, upper gastrointestinal bleeding is absent in some reported series in which new-onset fever and/or elevated inflammatory markers are the only clinical finding.1,2 When a fistula is established, only surgery can offer definitive treatment. However, in most cases, patients are considered unsuitable for emergent invasive procedures due to their poor general condition.1–4 In this particular case, we believe that esophageal stenting had a role in improving the septic shock and preventing bleeding. In the literature this endoscopic approach has been described more commonly in the presence of massive hemorrhage, and there is no bibliography specifying the secondary sepsis as indication for esophageal stenting.1,4,5
In conclusion, we highlight that esophageal stenting may play a role as a bridging procedure, improving the condition of these patients while awaiting surgery.
Ethical disclosuresRight to privacy and informed consentThe authors declare that no patient data appear in this article.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Conflicts of interestThe authors have no conflicts of interest to declare.