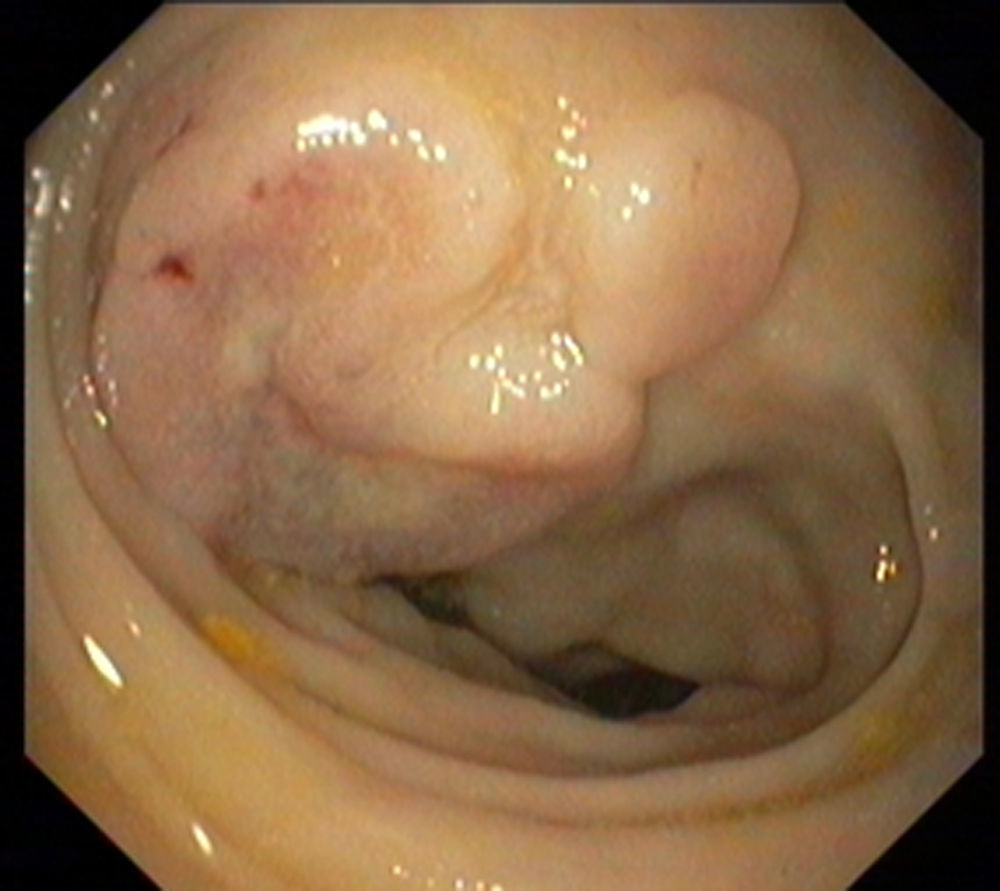
A 67-year-old caucasian man without significant past medical history presented with colicky abdominal pain, in the right lower quadrant, for the last 3 weeks. He also referred a total weight loss of 10% during the last month. Complete blood count revealed hemoglobin of 9.0g/dL with normal platelet and leukocyte count. Biochemical tests showed elevated C-reactive protein 148 (N: <3mg/L) and erythrocyte sedimentation 78 (N <20mm 1st hour). Serum lactate dehydrogenase levels were 1340 (N: 135–225U/L). Abdominopelvic computed tomography (CT) showed hepatomegaly and splenomegaly and a small amount of ascitis consistent with peritoneal carcinomatosis (Fig. 1). CT also revealed parietal thickening of the intestinal wall in the hepatic flexure. Colonoscopy showed in the hepatic flexure one round shape lesion, with 20mm of maximum diameter, predominately with normal mucosa and central ulceration (Fig. 2). Biopsies were performed and histologic examination revealed fragments of colorectal mucosa type, some with chorion occupied by some malignant cells of diffuse pattern consisting of intermediate to large cells. Immunohistochemical studies revealed positive lymphoid cells staining for CD20 in the absence of expression of CD5 and cyclin D1. Malignant cells had expression of CD10 and Mib 1/Ki-67, with proliferative index of about 100% (Fig. 3). Epstein–Barr antibodies were IgG (VCA and EBNA) positive and IgM and IgG (early) negative.
Bone marrow aspiration and biopsy were performed and flow cytometry revealed expression of surface immunoglobulin M, CD10, CD22, CD23, CD38 and CD79b. Fluorescence in situ hybridization was negative for (8:14) (q24; q32). However, the translocation MYC (8q24) was present in 53% of the malignant cells. The diagnosis of Burkitt lymphoma (BL) was performed and R-hiper-CVAD (cyclophosphamide, vincristine, doxorubicin and dexamethasone) chemotherapy regimen was started.
The authors describe a case of BL diagnosed by colonoscopy through a unique lesion in the hepatic flexure.1 The colonic involvement by a sporadic form of BL is not a rare phenomenon. However, it is usually present in the terminal ileum or with massive abdominal involvement.2,3
In this case, the colonic involvement allowed a prompt diagnosis and the initiation of an appropriate therapy of this aggressive lymphoma. Taking into consideration the rapid growth of a BL, the diagnosis should be performed as soon as possible and made by the least invasive procedure.
Conflicts of interestThe authors have no conflicts of interest to declare.