Acinar cell carcinoma (ACC) of the pancreas is a rare pancreatic malignancy, constituting only 1–2% of all exocrine pancreatic tumors.1–3 There is a slight male preponderance and it mostly presents in 5–7th decades of life. ACC arise more commonly from the head of the pancreas. Clinical symptoms are usually non-specific. In contrast to ductal adenocarcinoma, ACC rarely obstructs the common bile duct because it generally compresses and does not infiltrate into adjacent structures, so jaundice is infrequent (12%). It has a unique ability to produce pancreatic enzymes. Paraneoplastic syndrome may be the only presenting symptom in 15% of patients. Lipase hypersecretion syndrome characterized by subcutaneous fat necrosis, polyarthralgia and peripheral eosinophilia is a type of paraneoplastic syndrome associated with it. Skin nodules in this syndrome are commonly seen on the lower extremities and often mistaken for metastatic disease.1–3 Surgical resection is the best treatment for localized ACC but this is a highly aggressive tumor. Approximately 50% of the cases presented with metastasis at diagnosis. More than 70% the patients who undergo surgical resection are eventually confirmed to show recurrent disease.2,3 Chemotherapy and radiotherapy are therapeutic options when ACC is unresectable or recurs after resection, but no effective treatment strategies have been established. Although recent studies have clarified the characteristics of ACC it still has not been fully understood.4,5
We report a rare case of ACC with widespread metastases in a 35-year-old woman who presented with subcutaneous nodules as the initial symptom without evidence of subcutaneous fat necrosis. To our knowledge, this is the second report of ACC with skin metastases.3
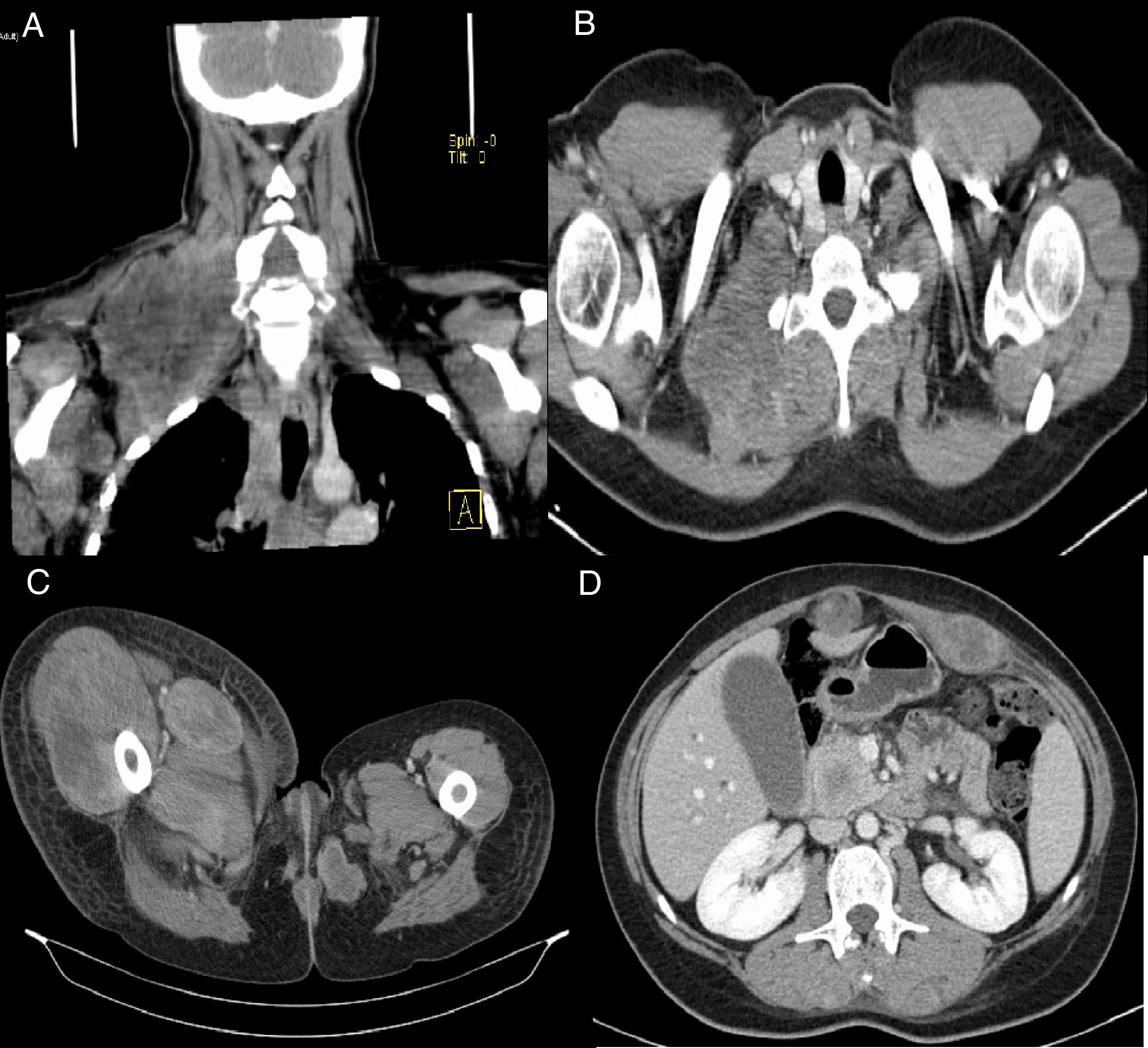
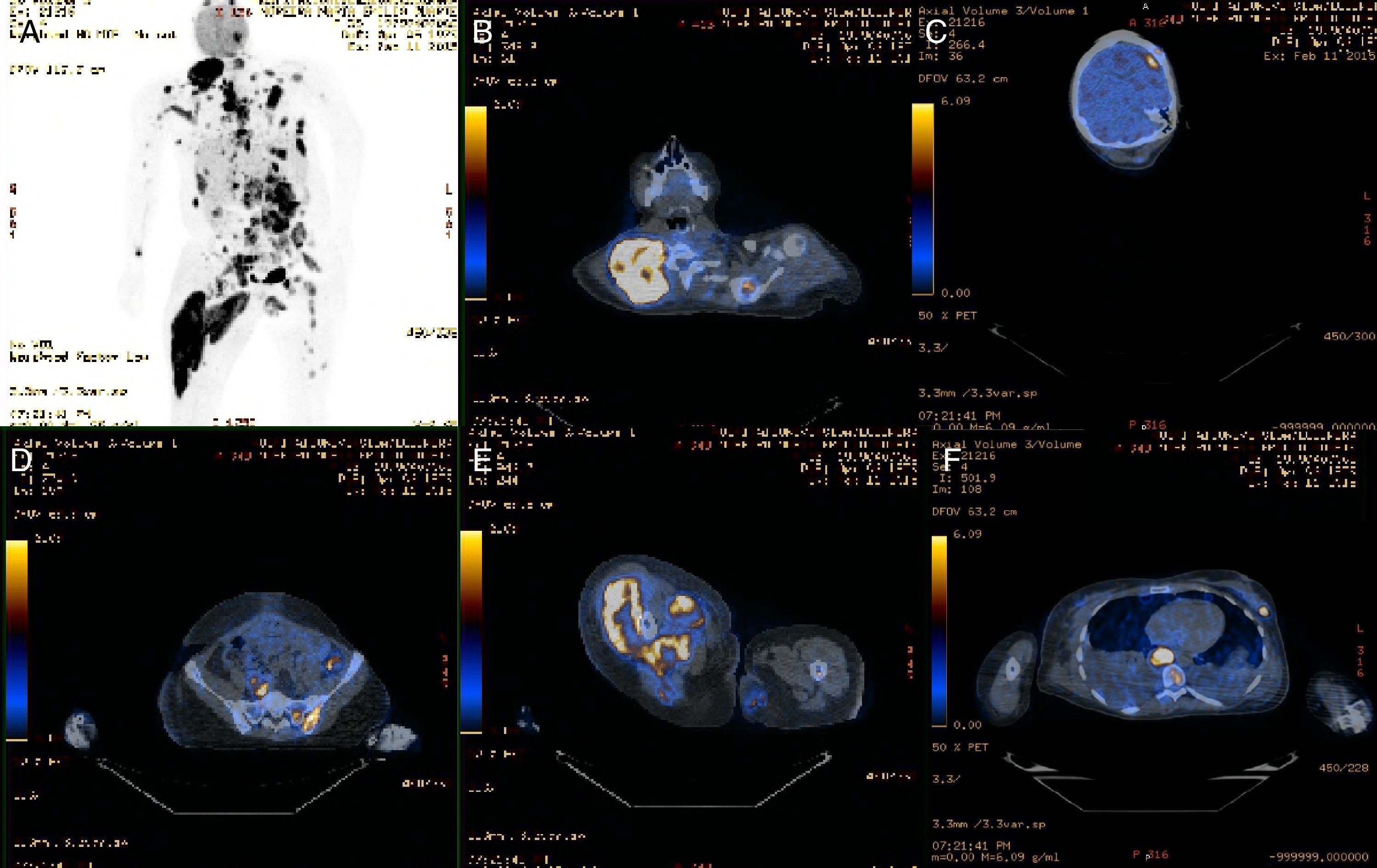
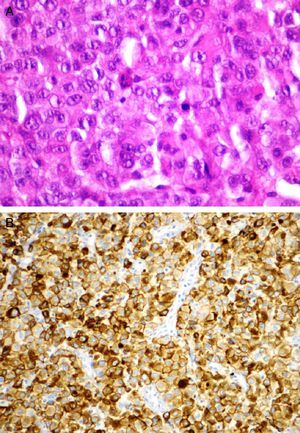
2Clinical caseA 35-year-old woman presents with a one week history of jaundice, abdominal discomfort and intensive asthenia associated with abrupt growth of painful nodules in the neck, abdominal wall and lower right limb. No history of trauma and fever. Without significant previous medical history. She had a delivery eight months ago without complications. Laboratory tests showed cholestasis (gamma glutamyl transpeptidase 346U/L (<55); alkaline phosphatase 230U/L (40–150); total bilirubin 4.4mg/dL (0.3–1.2); direct bilirubin 2.8mg/dL (0.1–0.5)) without other alterations. Ultrasonography showed moderate dilatation of the main bile duct and could not define the cause of obstruction. Computed tomography revealed multiple metastases in the lymph nodes (the largest with 10cm, Fig. 1A and B), in the skin/subcutaneous tissue, muscular (Fig. 1C) and also showed a 3cm mass involving the uncinate process suggestive of neoplastic nature (Fig. 1D). Positron emission tomography confirmed a hypermetabolic mass in the topography of the pancreas (probable primary lesion) and extensive metastasis of the lymph nodes and also in the muscle, lung, bone, cutaneous/subcutaneous tissue and brain (Fig. 2). A biopsy of the cervical node was performed and histological analysis revealed an undifferentiated carcinoma but with immunohistochemistry findings suggestive of ACC of the pancreas (Fig. 3). Under palliative care, patient died tree months after the diagnosis.
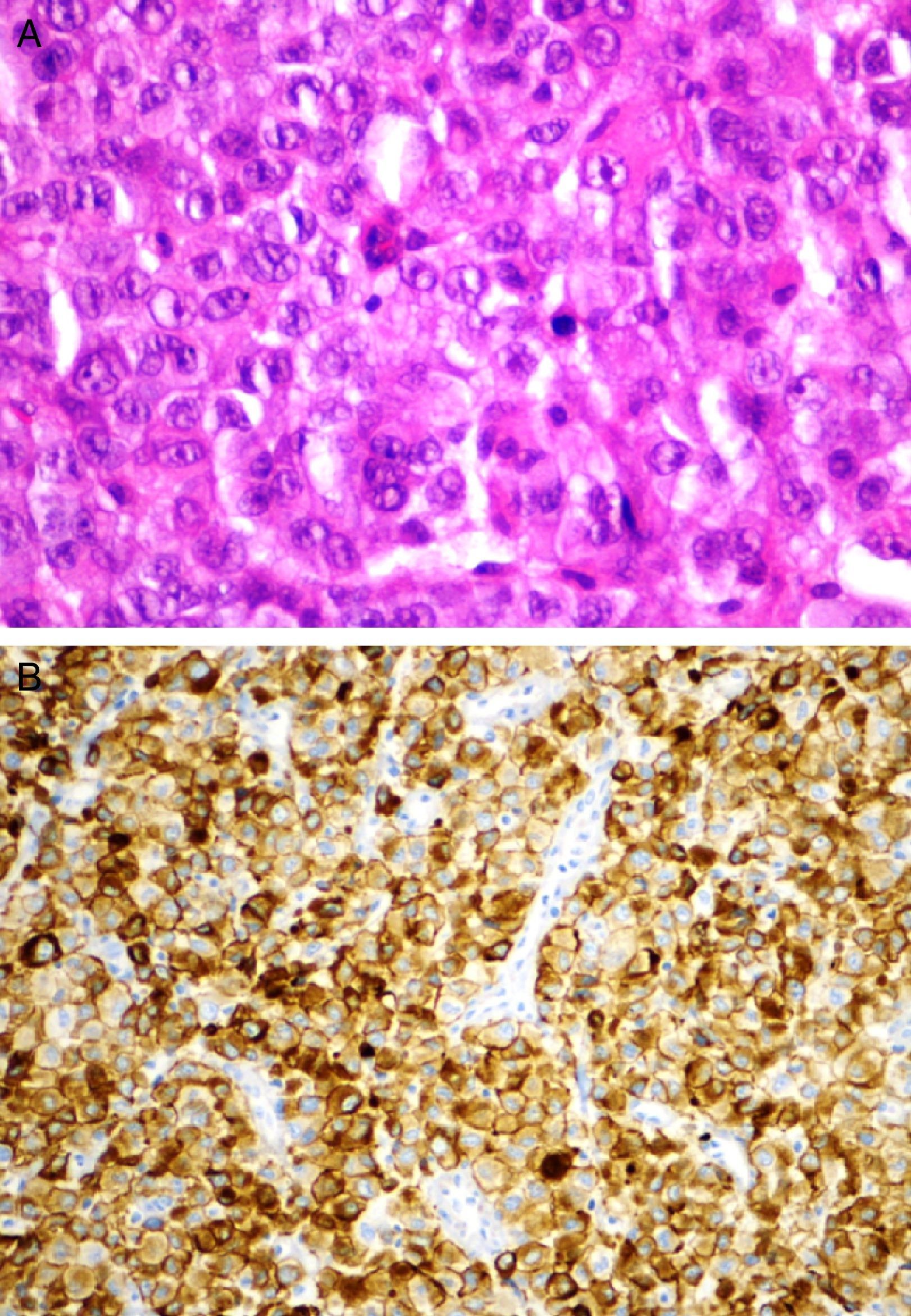
Histological analysis of the biopsy of the cervical node. Hematoxylin and eosin staining (A): poorly differentiated neoplastic cells with focal acinar formations, large nuclei exhibiting irregular chromatin clumping, size variation, and many mitotic figures are present, consistent with aggressive growth. Immunohistochemical staining (B): neoplastic cells express cytokeratin 8/18, cytokeratin CAM5.2, cytokeratin AE1/AE3, BCL10, β-catenin and alpha 1 antitrypsin.
Our patient was an uncommon presentation of a rare tumor with widespread metastases to various organs including the skin. This case emphasizes that ACC diagnosis although rare and usually associated with advanced ages cannot be ruled out in young patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.