Gastrointestinal stromal tumors (GISTs) are rare clinical entities, representing less than 0.2% of all gastrointestinal tumors and only 0.04% of small intestinal malignant neoplasms. GISTs may occur anywhere along gastrointestinal tract, but most commonly arise in the stomach (40–60%) and jejunum/ileum (25–30%).1,2
The clinical presentation of GISTs is highly variable depending on their size, location and presence of mucosal ulceration. Abdominal pain and gastrointestinal bleeding (when mucosal ulceration is present) are the most common symptoms or signs although persistent significant bleeding is unusual. Intussusception and subsequent obstruction is a very uncommon presentation of these lesions because of their tendency to grow in an extraluminal fashion.3,4 Very few cases of small bowel intussusceptions from stromal tumor in adults have been described in medical literature.1–5 Intussusception is rather infrequent in adults, accounting for 0.1% of all surgical admissions and 1–5% of mechanical bowel obstructions. In contrast to childhood, where intussusception is idiopathic in 90% of cases, in adults a definable pathologic lesion is established in over 90% of cases, with neoplasms considered to be the cause in 65% of them. Preoperative diagnosis is often difficult because the symptoms are nonspecific.1–3 Intussusception is correctly diagnosed preoperatively in only one-third of cases.1,3
The relative rarity of GISTs combined with nonspecific presentation results in delayed diagnosis. Frequently, this is only possible after surgery and histological examination.2,3,5
We report an unusual case of jejunojejunal intussusception caused by a GIST which first presentation was a long-standing obscure gastrointestinal bleeding, incorrectly established as determined by a small bowel angyodisplasia after capsule endoscopy examination.
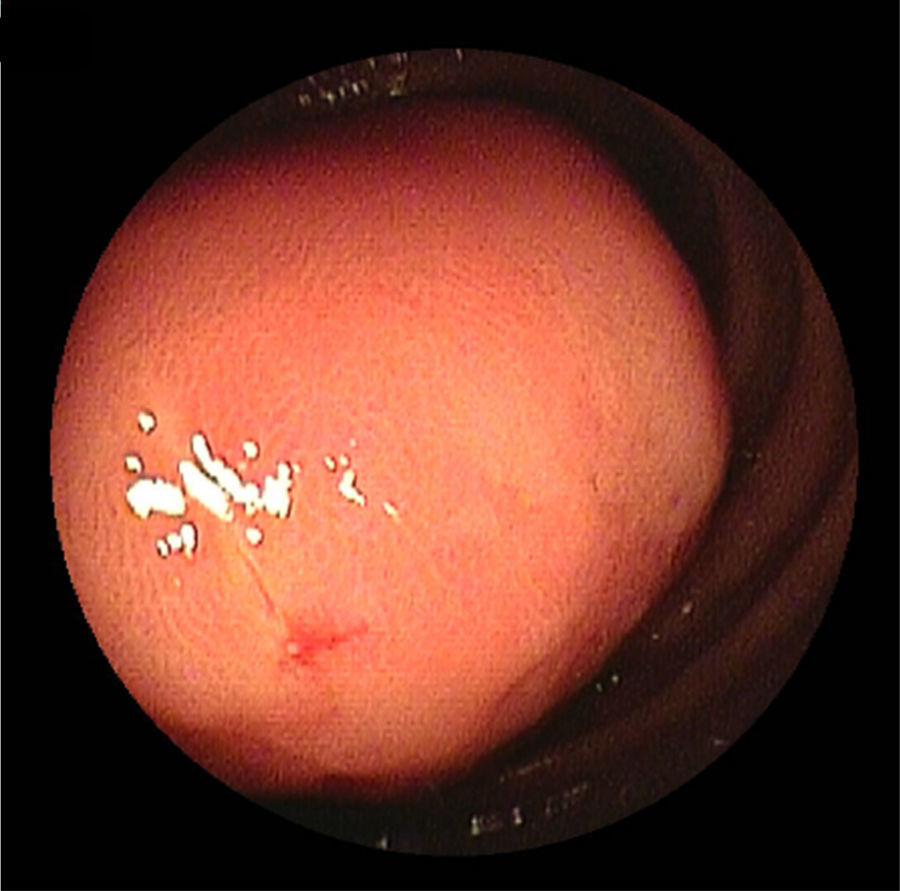
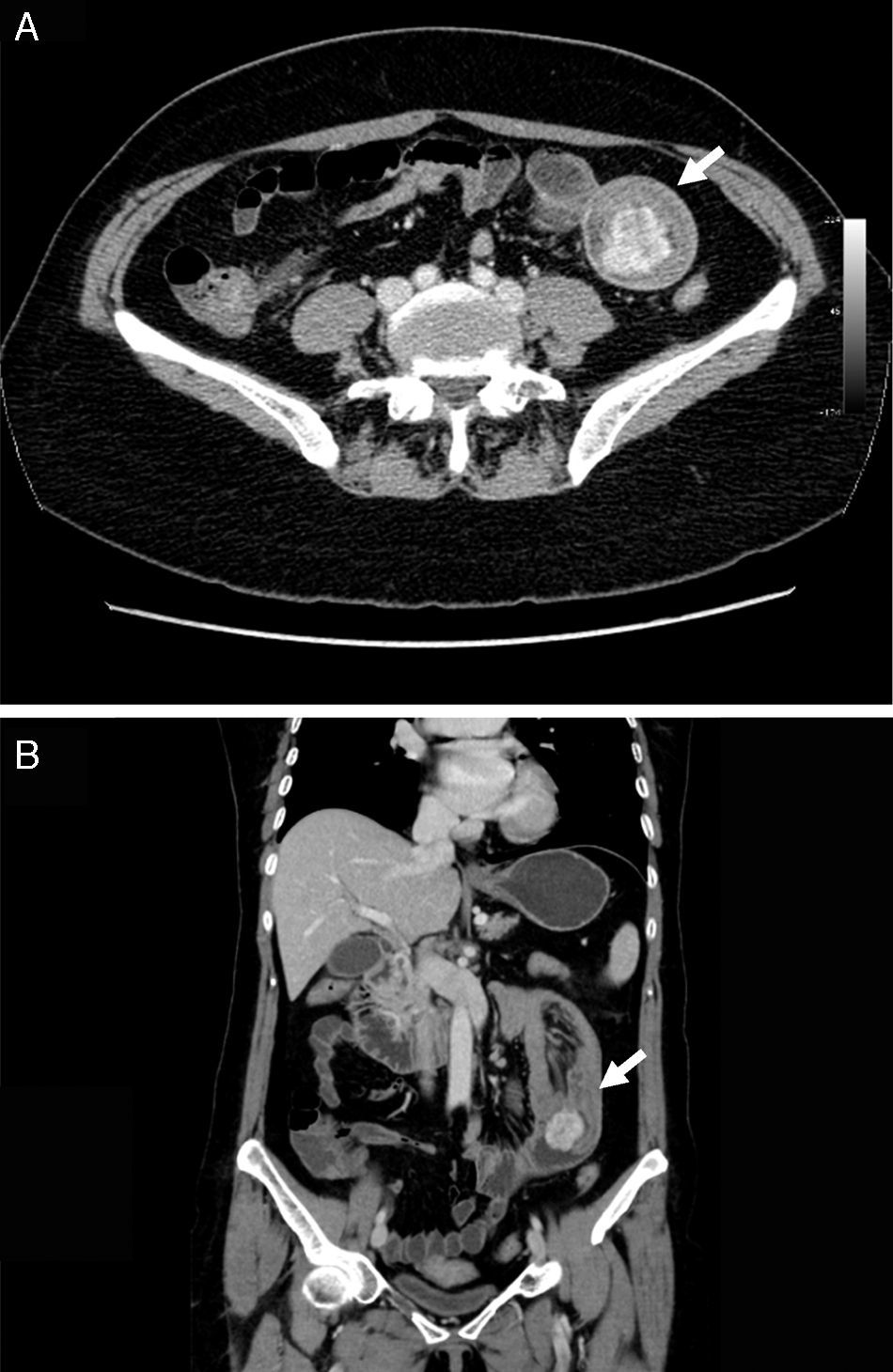
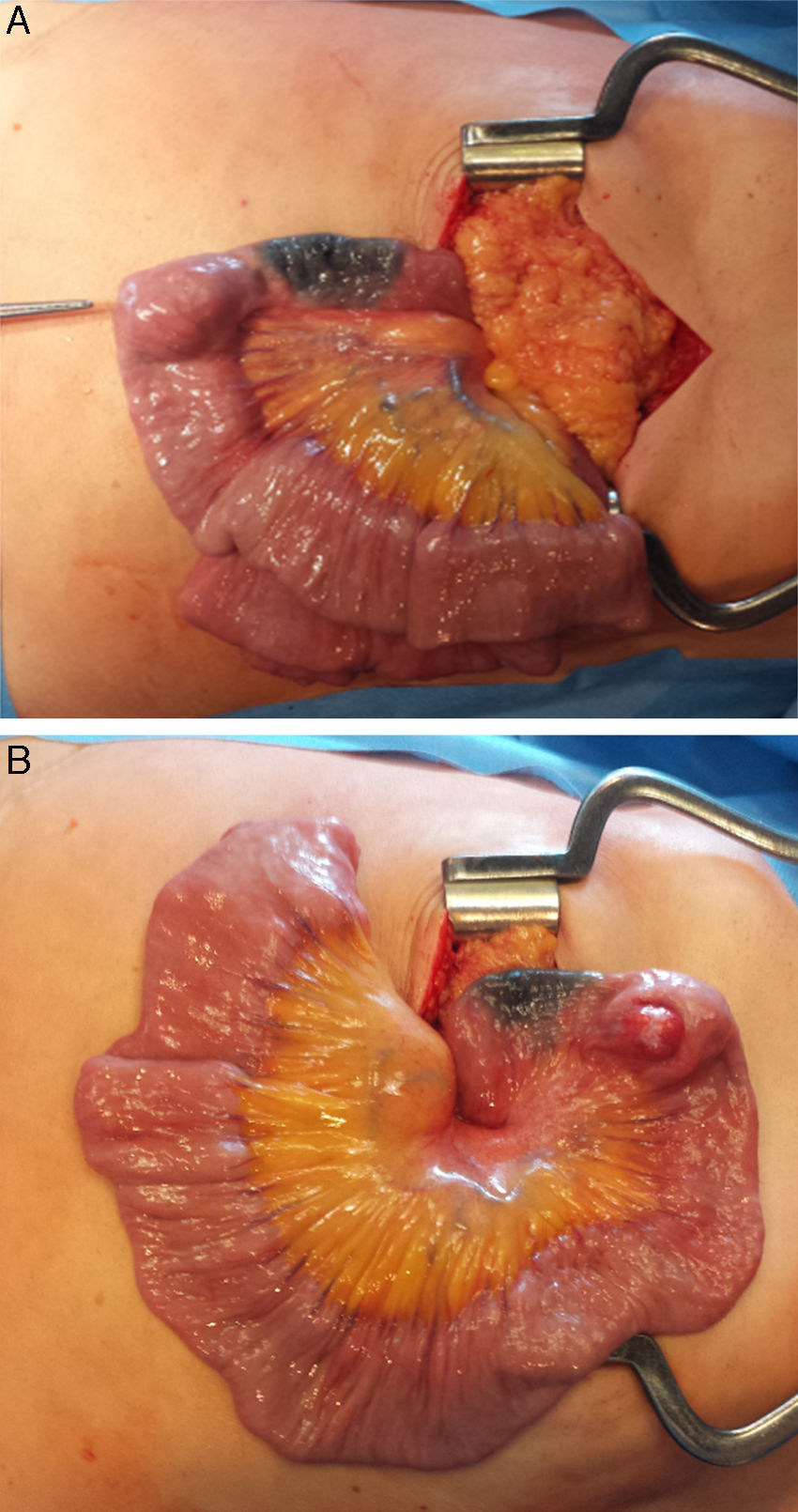
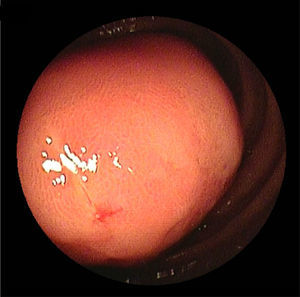
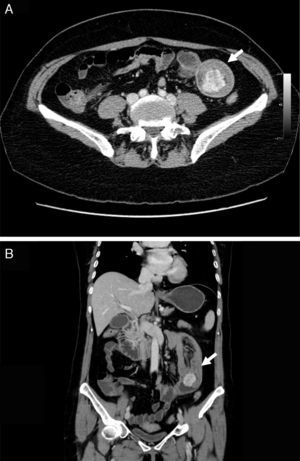
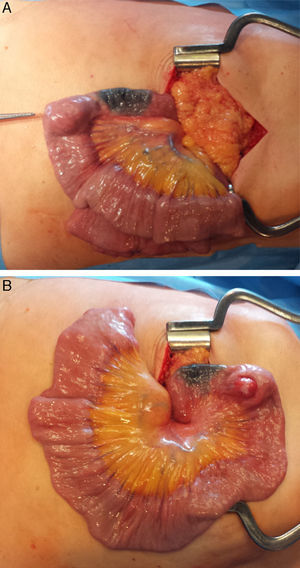
2Case descriptionA 58-year-old woman was previously hospitalized for gastrointestinal bleeding (melena) requiring frequent blood transfusion. Standard gastrointestinal endoscopic study (upper endoscopy, colonoscopy) revealed no gastrointestinal lesions. The patient underwent capsule endoscopy, which identified an angiodysplasia in the mid-jejunum. She was referred to double balloon enteroscopy for specific thermal therapy. While waiting for this intervention the patient started persistent nausea and postprandial vomiting, suggesting a suboclusive lesion. The enteroscopy revealed an ulcerative subepithelial lesion protruding to the lumen of the proximal jejunum (Fig. 1). Biopsies were performed (which were inconclusive) and the lesion, that was partially obstructive, was marked with India ink tattoo. Computed tomographic scan showed in the proximal jejunum a hypervascular mass with 3cm suggestive of GIST conditioning intussusception in this segment (Fig. 2A and B). The patient underwent laparotomy that identified a jejunojejunal intussusception secondary to jejunal tumor (Fig. 3A and B). The lesion was resected and histological examination revealed a GIST tumor (R0). The recovery was uneventful and the patient was discharged on the 7th postoperative day. There was no clinical or radiologic evidence of recurrence at follow-up (Stage I-T2, N0, M0).
Intraoperative view showing the jejunojejunal intussusception with the bowel proximal to this area dilated. There was an intraluminal mass arising from the wall of the jejuno making the lead point of intussusceptions (A). Resection of the jejunal segment bearing the mass (B) with end-to-end jejunojejunal anastomosis was done.
This case reveals a false negative of capsule endoscopy in a large proximal small bowel tumor, the simultaneous presentation of a GIST lesion as an intestinal intussusception and gastrointestinal bleeding as well as the importance of balloon enteroscopy and abdominal CT in the evaluation of these patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.