A 56 years-old male was admitted to the emergency department with retrosternal pain and progressive dysphagia starting one week before. He had total dysphagia in the last 12h. Patient denied weight loss, heartburn or other symptoms, as well as a relevant medical history. Results of physical examination and blood tests were unremarkable. Chest radiograph and electrocardiogram were normal.
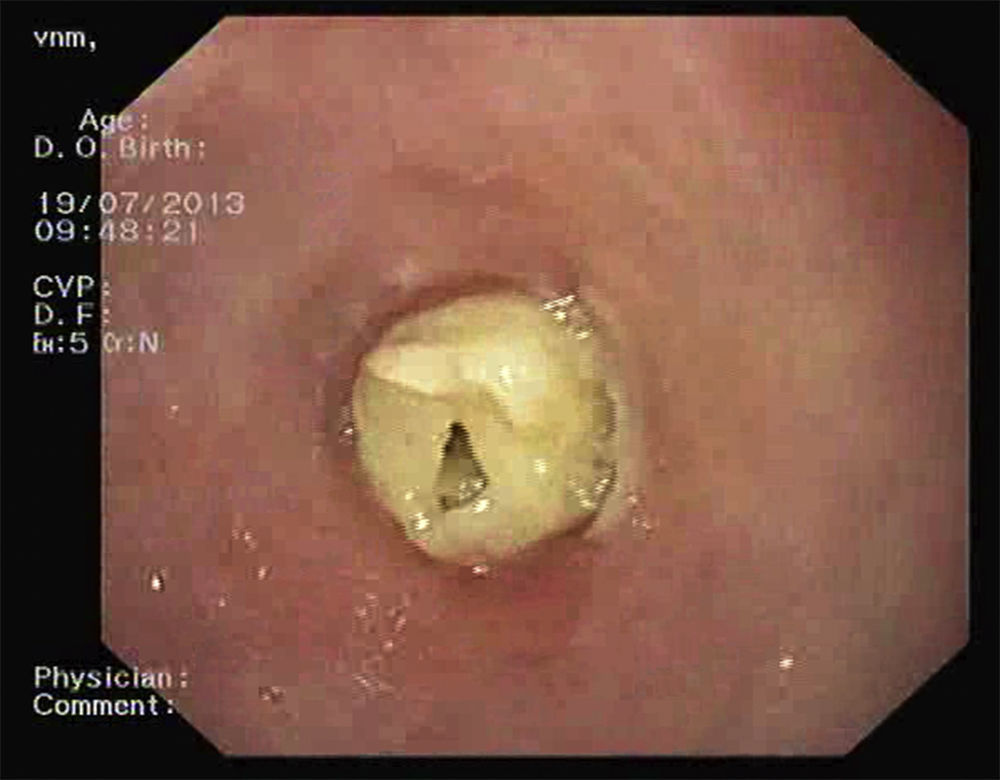
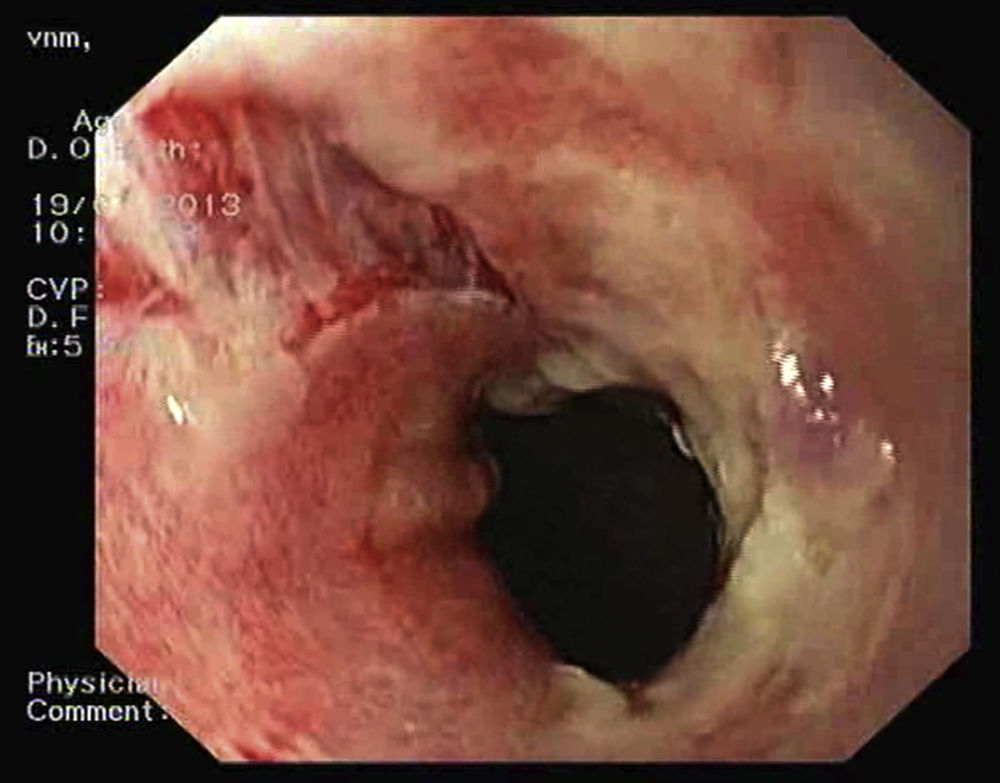
Upper endoscopy revealed a yellowish, soft consistency content in the distal esophagus, causing a total lumen occlusion, initially interpreted as a possible food impaction (Fig. 1). After removal, an ulceration and extensive sloughing of the underlying mucosa, with vertical laceration and horizontal cracks, was observed (Fig. 2). In the gastroesophageal junction, mucosa had an irregular appearance, simulating a neoplastic lesion and causing parcial stenosis of the lumen. Biopsies were taken.
Patient was again questioned about ingestion of caustics, hot beverages or drugs such as potassium chloride, nonsteroidal anti-inflammatory drugs or bisphosphonates. He was taken alendronate 10mg/day for the last three months, due to an osteoarticular disease, but was not complying with recommendations for bisphosphonates intake.
Patient was admitted with the probable diagnosis of sloughing esophagitis caused by biphosphonates. Intravenous acid suppression and oral sucralfate were started and alendronate was stopped. On the next day, he began a liquid diet and had a progressive improvement of complaints.
Biopsies revealed an inflammatory infiltrate, with hyperplastic cells, without dysplasia or neoplastic cells. Computed Tomography scan showed a 4cm regular and circumferential thickening of the distal esophagus. Cleavage planes with adjacent structures were preserved.
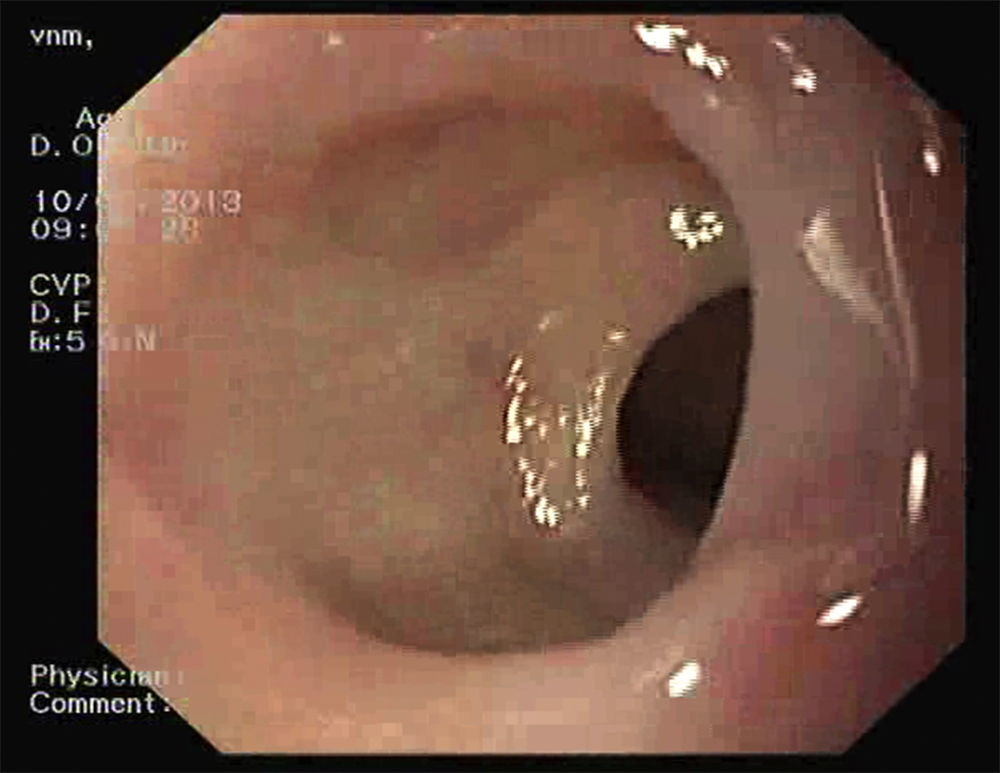
Upper endoscopy performed one week and two months later (Fig. 3) showed a progressive mucosal healing, maintaining minimal friability, with no stenosis. Repeated biopsies were negative for neoplasia.
Sloughing esophagitis is a rare diagnosis in clinical practice.1 Although the exact pathogenesis remains unexplained and the histopathologic features are inadequately described, an association with caustic or hot beverages ingestion, autoimmune bullous dermatosis (such as pemphigus vulgaris), and drugs such as potassium chloride, nonsteriodal anti-inflammatory drugs and bisphosphonates, has been reported.1–4 Mechanisms underlying biphosphonates esophageal injury appears to be related with production of a caustic alkali solution that causes a direct mucosal damage. This damage was described more frequently with alendronate use.5 To minimize the risk of esophageal injury, patient should be advised to take biphosphonates with 250ml of water and to remain in a upright position for at least 30min after taking the pill. A combination of acid suppression and the discontinuation of precipitating medications has been reported to result in the healing of the mucosa.1,2
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.