The authors present the clinical case of a 14-year old girl with weight loss, anorexia, epigastric abdominal pain and postprandial vomiting with 5 months duration. There was a background of trichophagia for 2 years without evidence of alopecia or psychiatric history. The physical examination revealed an epigastric mass motionless, stony, with poorly defined limits, painful on palpation and about 7cm diameter. Abdominal ultrasonography showed thickening of the gastric wall and antrum with gastric distension. The abdominal tomography scan and endoscopic examination revealed the presence of a bulky trichobezoar occupying almost the entire gastric lumen. It was decided to undergo gastrotomy and extraction of the bezoar. The postoperative period was uneventful.
Apresentamos o caso clínico de uma adolescente de 14 anos com emagrecimento, anorexia, epigastralgia e vómitos pós-prandiais com 5 meses de evolução. Apurou-se história de tricofagia com 2 anos de evolução mas sem áreas de alopécia ou antecedentes psiquiátricos. Apresentava massa epigástrica imóvel, pétrea, de limites mal definidos, dolorosa à palpação e com cerca de 7cm de diâmetro. A ecografia abdominal mostrou espessamento da parede gástrica e do antro com distensão gástrica. Realizou tomografia abdominal e endoscopia digestiva alta que revelaram a presença de volumoso tricobezoar ocupando quase a totalidade do lúmen gástrico. Foi decidido realizar gastrotomia e extração do bezoar. O pós-operatório decorreu sem incidentes.
Bezoars are concretions of undigested or partially digested foreign material in the gastrointestinal or genitourinary tract.1
They are classified according to their composition. The major types are phytobezoars (composed of vegetable matter), trichobezoars (composed of hair) and pharmacobezoars (composed of ingested medications).1–3 There are others composed of a variety of other substances as tissue paper, fungus, cement, vinyl gloves, milk curd.
Development of bezoars is usually associated with predisposing risk factors. They occur in patients with altered gastrointestinal motility and/or anatomy (previous gastric surgery, diabetes mellitus, neurological disorders). Psychiatric illness, suicidal tendencies and mental retardation are common associations with trichobezoar (hair bezoar).1,3 They begin as retained hairs between the gastric folds; the hair is then denatured by gastric acid, becomes black due to oxidation and combines with food to form an enmeshed mass. Trichobezoars subsequently become colonized by bacteria resulting in halitosis.
They are rare, with an estimated incidence of 0.3 percent on upper endoscopy.4 Trichobezoars are typically seen in women in their 20s and are often associated with psychiatric disorders.5
They cause nonspecific symptoms and are usually found incidentally in patients undergoing upper gastrointestinal endoscopy or imaging. The most common symptoms include abdominal pain, nausea, vomiting, early satiety, anorexia, and weight loss.3,5 They represent an uncommon cause of abdominal mass.
The bezoars although rare, when undiagnosed can lead to complications such as ulcers, gastric bleeding or perforation and obstruction.3,5 Although many bezoars become quite large, gastric outlet obstruction is an uncommon presentation.
2Clinical caseA 14-year old girl was admitted to the Department of Pediatrics with weight loss (5kg), anorexia, epigastric abdominal pain and postprandial vomiting with 5 months duration. She denied the presence of fever, altered bowel habits or visible blood loss. She had no distortion of body image or eating pattern changes.
Her history revealed significant trichophagia for 2 years without evidence of alopecia or psychiatric history.
On clinical examination she was pale and skinny. Her vital signs were within normal limits and the higher intellectual functions were normal. There was no dehydration, halitosis or lymphadenopathy. There was an epigastric mass of stony consistency, bulky, with poorly defined limits, painful on palpation and about 7cm diameter.
Laboratory investigation revealed anemia (hemoglobin – 7.6g/dL).
Abdomen radiograph showed marked gastric distension with gastric camera barely visible (Fig. 1).
On the abdominal ultrasonography there was thickening of the gastric wall and antrum with gastric distension.
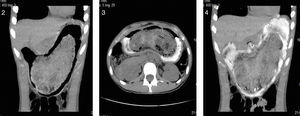
It was then performed an abdominal tomography scan to exclude other bezoars in the small intestine that revealed the presence of a bulky bezoar difficult to characterize, occupying almost the entire gastric lumen and causing compression of neighboring structures (Figs. 2–4).
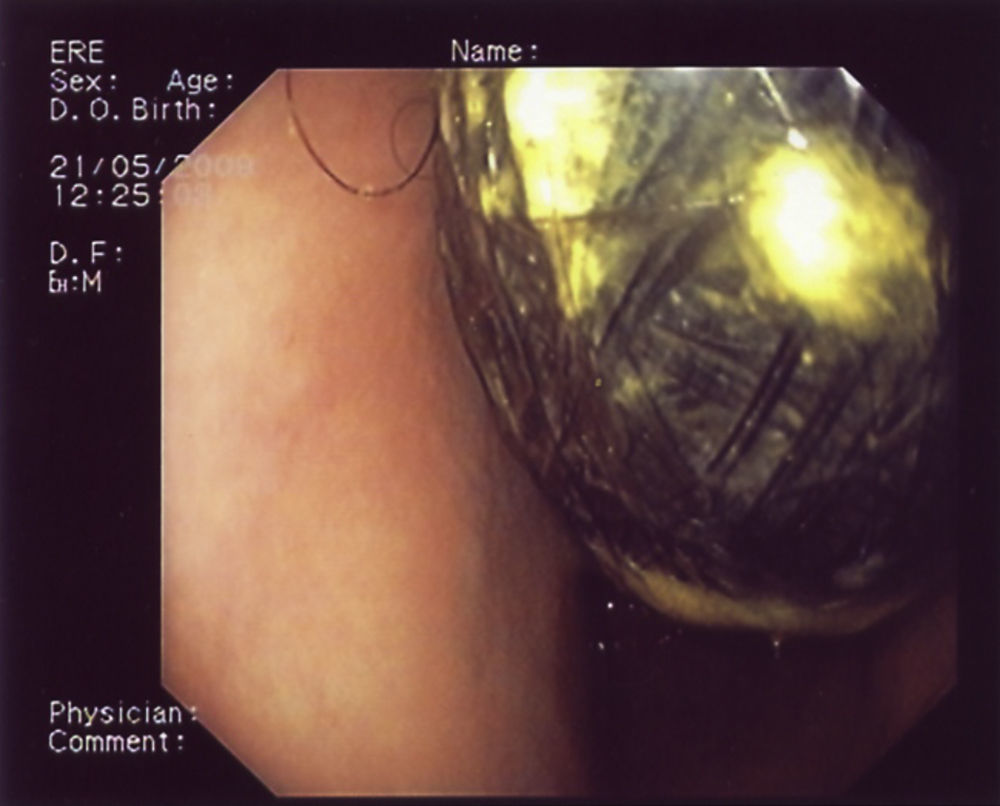
The endoscopy confirmed the diagnosis of a large volume trichobezoar not amenable for chemical dissolution or endoscopic fragmentation (Fig. 5).
Given the large mass causing gastric outlet obstruction and compression of neighboring structures it was decided to undergo laparotomy. Through the gastrotomy, a gastric trichobezoar 15-cm-long was removed (Fig. 6). The postoperative course was uneventful with resolution of the gastrointestinal symptoms.
She recovered well from the procedure without any complications, had a psychological evaluation and was symptom-free on discharge. She was started on an iron therapy and encouraged to seek psychiatric evaluation if needed. She is symptom-free at 6-year follow-up and had no recurrence of trichophagia.
3DiscussionBezoars are usually discovered as an incidental finding on imaging performed for evaluation of nonspecific symptoms. Abdominal radiograph with or without barium, abdominal ultrasound, or computed tomography scan may show the bezoar as a mass or a filling defect. Upper gastrointestinal endoscopy is required to establish the diagnosis and to obtain samples to determine the composition of the bezoar.3,6
Therapy for bezoars should be tailored to the composition of the concretion and to the underlying pathophysiologic process. The optimal strategy is controversial in the absence of studies comparing different modalities. For patients with mild symptoms due to gastric bezoars, it is suggested initial treatment with chemical dissolution. For patients with bezoars that fail to dissolve after two attempts at chemical dissolution or are resistant to chemical dissolution (trichobezoars) or moderate to severe symptoms due to large bezoars, it is suggested endoscopic therapy.7–9 Surgery should be reserved for selected patients with gastric bezoars if chemical dissolution and endoscopic fragmentation cannot be performed or fail and for patients with complications such as significant bleeding or obstruction as was the case in our patient. The standard surgery is a laparotomy with gastrotomy. If this is performed to remove bezoars, the remainder of the stomach and small bowel should be examined to exclude other retained bezoars. Other therapies include extracorporeal shock wave lithotripsy, NdYaG laser and laparoscopic removal.3
After trichobezoar removal, prognosis is good if there is prevention of recurrence.3 Up to 20 percent of patients have recurrent bezoars.10 In order to prevent recurrence, patients should be encouraged to increase water intake, modify their diet, chew their food carefully and seek psychiatric evaluation if needed. Patients should also be evaluated for an underlying motility disorder. Our patient had a history of trichophagia and psychological management to control her psychiatric disorder was successful and at 6-year follow-up she is symptom free and had no further recurrence of trichobezoar.
Conflicts of interestThe authors have no conflicts of interest to declare.