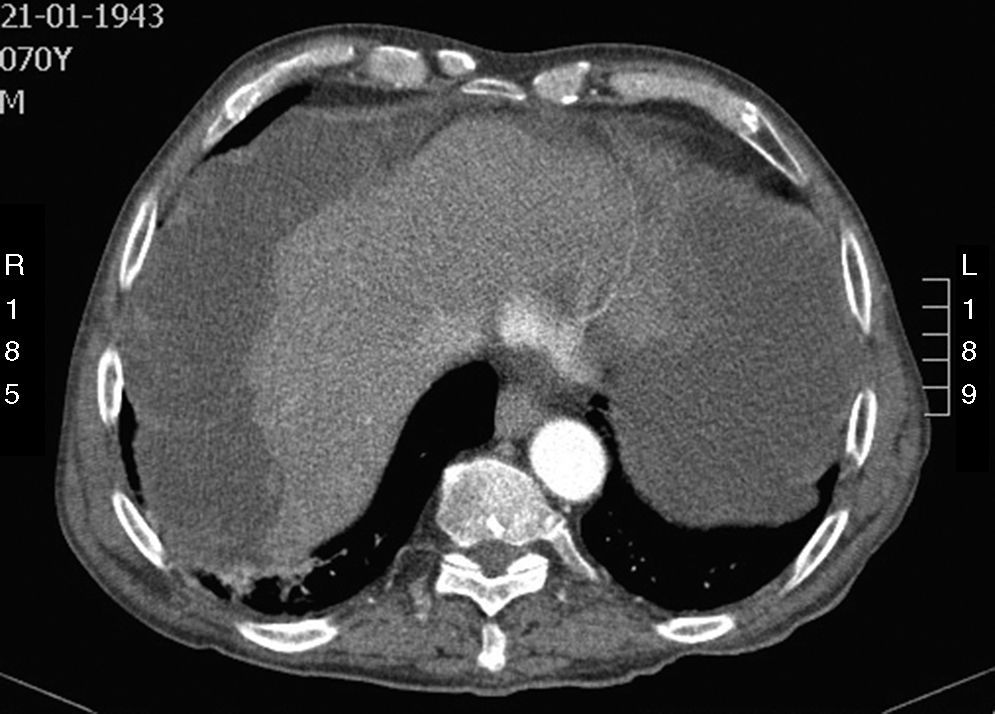
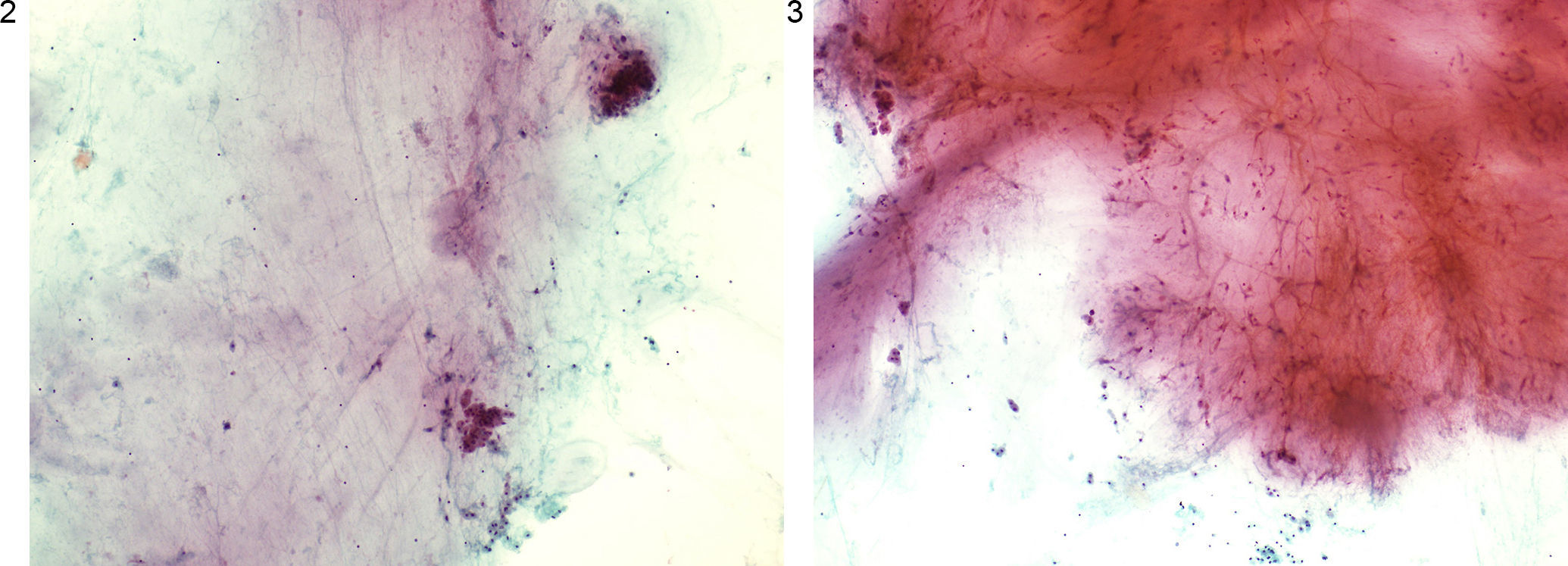
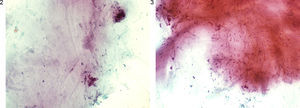
A 70-year-old man with significant past medical history of hypertension, atrial fibrillation and cerebral vascular disease was admitted for anorexia, weight loss (10kg) and increased abdominal girth for the past 3 months. On examination, a voluminous ascites was noted, with no signs of chronic liver disease. Laboratory studies showed an isolated elevation of serum inflammatory markers (C-reactive protein and erythrocyte sedimentation rate). Abdominal ultrasound (US) and computed tomography (CT) were performed and revealed CT low-attenuation heterogeneous ascites that scalloped the margins of the liver and spleen (Fig. 1). Diagnostic paracentesis revealed thick gelatinous ascitic fluid, rich in mucin on cytology examination (Figs. 2 and 3). Ascitic fluid cell count was not possible due to high viscosity and cultures were negative.
The radiologic and cytotogic findings were crucial to support the diagnosis of pseudomyxoma peritonei (PMP). Despite being proposed for surgery, there was a rapid clinical deterioration and the patient died 11 weeks after the diagnosis.
PMP is a rare and intractable clinical syndrome, with an estimated incidence of 1–2 per million per year. It is characterized by copious amounts of mucinous ascites and mucinous peritoneal implants, leading to progressive obliteration of the peritoneal cavity and intestinal obstruction. The most common sites of origin are tumors of the appendix and ovary and in up to 5% of the patients the origin remains unknown. Despite being a rare cause of ascites, with approximately one hundred cases reported worldwide, PMP must be considered in the differential diagnosis of ascites, particularly if gelatinous. Imaging is key to the initial diagnosis, revealing typical findings on US, CT and magnetic resonance imaging such as heterogeneous ascites scalloping the visceral surface of the liver and spleen. Diagnostic confirmation is made by ascitic fluid cytology showing abundant extracellular mucus. Treatment is controversial and the most satisfactory and effective approach is a combination modality of cytoreductive surgery and intraoperative chemotherapy.1–3
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Author contributionsSusana Marques did the writing of the manuscript. Joana Carmo, Miguel Bispo and Cristina Chagas were responsible for the revision of its contents.
Conflict of interestAll authors have approved the manuscript and agree with its submission to GE – Portuguese Journal of Gastroenterology. All authors have nothing to disclose.