Parental burnout increases the risk of deleterious consequences on parents’, couples’, and children's physical and mental health.
MethodsThe current study (N = 134) aimed to assess the effectiveness of a Cognitive Behavioural Stress Management (CBSM) group programme in terms of parental burnout reduction. In total 67 parents attended the 8-week CBSM intervention groups, and another 67 parents were assigned to the waiting-list control group. We compared the effectiveness of the CBSM intervention with a waiting-list control group directly after the end of the programme and at three-months follow-up.
ResultsThe results showed that compared to the control group the CBSM programme contributed to the reduction of parental burnout symptoms with statistically significant and small effect size. Moreover, the contrast analyses showed that the reduction in parental burnout severity was maintained at 3 month-follow-up. The reduction in parental burnout scores was mediated by the decrease in stress and the increase in unconditional self-kindness.
ConclusionsThese results highlight the potential benefits of the CBSM programme for parental burnout prevention and reduction.
Being a parent presents both challenging and rewarding experiences (Deater-Deckard, 1998). In that sense, all parents are exposed to parenting stress to a different degree and with various consequences on family functioning and well-being (Crnic & Greenberg, 1990). Parenting stress is a dynamic process involving an interaction between parent, child, and environment (Berry & Jones, 1995). The experience of parenting strain relates to the multiple demands, constraints, and opportunity costs entailed by parental role (e.g., mental load, limited time for oneself, sense of responsibility) which can be balanced by the rewards of parenting, such as the sense of fulfilment and personal growth (Sheldon et al., 2021), and an individual's ability to cope with stress (Lazarus, 1993). Yet, chronic imbalance between parenting stress and rewards increases the risk of parental burnout (Mikolajczak & Roskam, 2018).
Parental burnout is a context specific syndrome characterised by emotional and physical exhaustion, decreased sense of accomplishment in parental role, emotional distancing from a child, and a contrast in parental self, that is, an impression of not being a good parent anymore (Roskam et al., 2018). In the general population, the prevalence of parental burnout varies across countries from 0% in Cuba, 3.3% in United Kingdom, 6.2% in France, 8.9% in USA and up to 9.8% in Belgium (Roskam et al., 2021). However, the prevalence of parental burnout can reach even 36% among the parents of children with chronic diseases (Lindström et al., 2010). The consequences of parental burnout can lead to multiple impacts on parents’ physical and mental health, couple functioning, and the child's development (Mikolajczak et al., 2018). More specifically, at the parental level, burnout severity increases the incidence of suicidal ideation, sleep disorders, and addictive behaviours. Moreover, the emotional distancing symptoms of parental burnout are likely to contribute to couple conflicts, and neglectful and violent behaviours toward the child. Given that parental burnout could “constitute direct threat to children's psychological and physical safety” as well as parents’ health (Mikolajczak et al., 2018, p. 143), it appears crucial to prevent and treat parental burnout in order to limit its negative consequences on parents’ and children's well-being.
A recent meta-analysis identified currently used interventions for parental burnout among the parents of chronically ill children and parents from the general population (Urbanowicz et al., under review). The results of this meta-analysis suggested that psychological group interventions significantly contributed to the reduction of parental burnout symptoms compared to a control group. Among the interventions which showed their effectiveness were mindfulness, cognitive-behavioural therapy (CBT), acceptance and commitment therapy (ACT), psychoeducation, active-listening, and interventions targeting the development of parenting resources and the reduction of stress. Although these findings are very promising, existing evidence is still limited: the meta-analysis only identified 8 studies evaluating 11 interventions for parental burnout treatment. In addition, all identified studies focused on the parents presenting severe parental burnout symptoms: there is no evidence of these programmes playing a preventative role among the parents at risk. Therefore, there is a need to further evaluate these types of interventions both for parental burnout prevention and treatment.
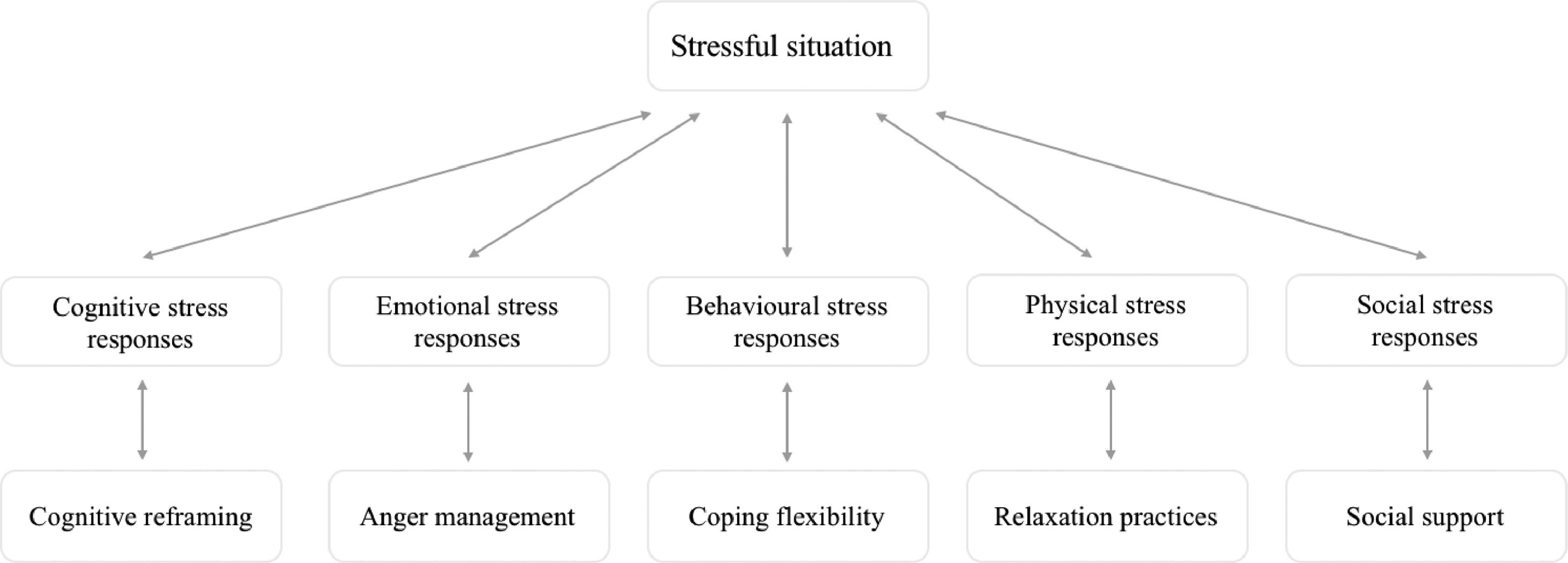
The present study assessed the effectiveness of an 8-session Cognitive Behavioural Stress Management (CBSM) programme among parents from general population. The CBSM is a group intervention based on cognitive-behavioural therapy (CBT) and relaxation techniques aiming to develop appropriate stress management skills for affective, behavioural, cognitive, physiological, and social stress responses (see Fig. 1; Antoni et al., 2000; Gauchet et al., 2012). CBT interventions are considered as a gold standard in the field of psychotherapy and use empirically supported techniques and standardised treatment protocols for specific disorders (David et al., 2018).
Cognitive Behavioural Stress Management (CBSM) Model (adapted from Antoni et al., 2007).
During the CBSM programme participants learn to identify different sources of stress in their daily life and to increase their self-awareness of stress responses. The CBSM programme uses cognitive and behavioural techniques aiming to modify maladaptive cognitive and emotional regulation strategies (e.g., cognitive reframing, anger management, coping strategies, assertiveness techniques), as well as relaxation and meditation techniques to reduce physical stress and enhance self-awareness and psychological flexibility. In addition, a group format of the intervention favours social ties between participants which in turn may contribute to well-being and health (Kemp et al., 2017). Moreover, during the sessions participants learn to distinguish controllable and uncontrollable aspects of their difficulties, how to mobilise coping resources and social support, and how to identify, express, understand, regulate, and use overwhelming difficult emotions in a constructive way. Both during sessions and in between the sessions, participants practice self-monitoring of their responses to stress, relaxations, and cognitive reframing exercises based on their daily life situations. All these practices aim to develop stress management resources and help to choose the behaviour rather than responding automatically.
The CBSM programme has been widely assessed and has shown its effectiveness in many stress-related disorders, including among patients suffering from chronic illnesses, in the reduction of depressive, anxious, and stress-related symptoms (Antoni et al., 2000; Phillips et al., 2011). Given the stress-related nature of parental burnout the CBSM programme could be effective in terms of parental burnout prevention and treatment. Yet, in the context of parenting, the efficacy of CBSM intervention has been evaluated in only one study among Iranian mothers (Karamoozian et al., 2015). The study measured the efficacy of a CBSM programme on anxiety and depression levels during pregnancy (N = 30). Compared to the control group, the results suggested the effectiveness of CBSM both in terms of mothers’ anxiety and depression reduction during pregnancy, as well as on the new-born babies’ physical health. However, the study design lacked a follow-up evaluation, and did not evaluate the mothers’ burnout, or depressive and anxiety symptoms following childbirth. Despite the promising results of this study, we cannot conclude on the effectiveness of the CBSM programme in terms of parental burnout reduction. To our knowledge no other study adapted the content of the CBSM programme to the context of parental burnout and evaluated its effectiveness. Given the high prevalence of parental burnout and its deleterious consequences it seems crucial to assess to what extent already existing programmes based on empirically supported techniques contribute the prevention and treatment of parental burnout, and through which mechanisms of action. This would help to determine the need for creating new programmes specific for parental burnout and/or to continue the validation and dissemination of the CBSM programme to the population of parents at risk of burnout by already trained psychologists.
Present studyThe aim of the present study was to assess the effectiveness of the CBSM parenting programme in terms of parental burnout severity following an 8-week programme at three-months follow-up compared to a waiting-list control group. The 8-sessions design and the follow-up at three-months was chosen based on the previous interventional studies in the context of parental burnout (Anclair et al., 2018; Bayot et al., 2021; Brianda et al., 2020; Lindström et al., 2016). Based on these previous studies, the duration of 8-sessions seemed adequate to observe the change in parental burnout severity and to maintain the involvement of participants: shorter programmes could not be enough to develop the stress management competencies, and longer programmes could increase the drop-out rate. Moreover, the choice of similar duration of the programme and of the follow-up enables the comparison of effectiveness across the studies. We hypothesised that compared to the control group, the programme would contribute to a reduction in parental burnout scores. Our second hypothesis was that the decrease in parental burnout would be maintained up to three-months post-intervention. We further hypothesised that the reduction in parental burnout would be associated with the decrease in stress and abstract ruminations as well as the increase in unconditional self-kindness and intra-personal emotion regulation competences.
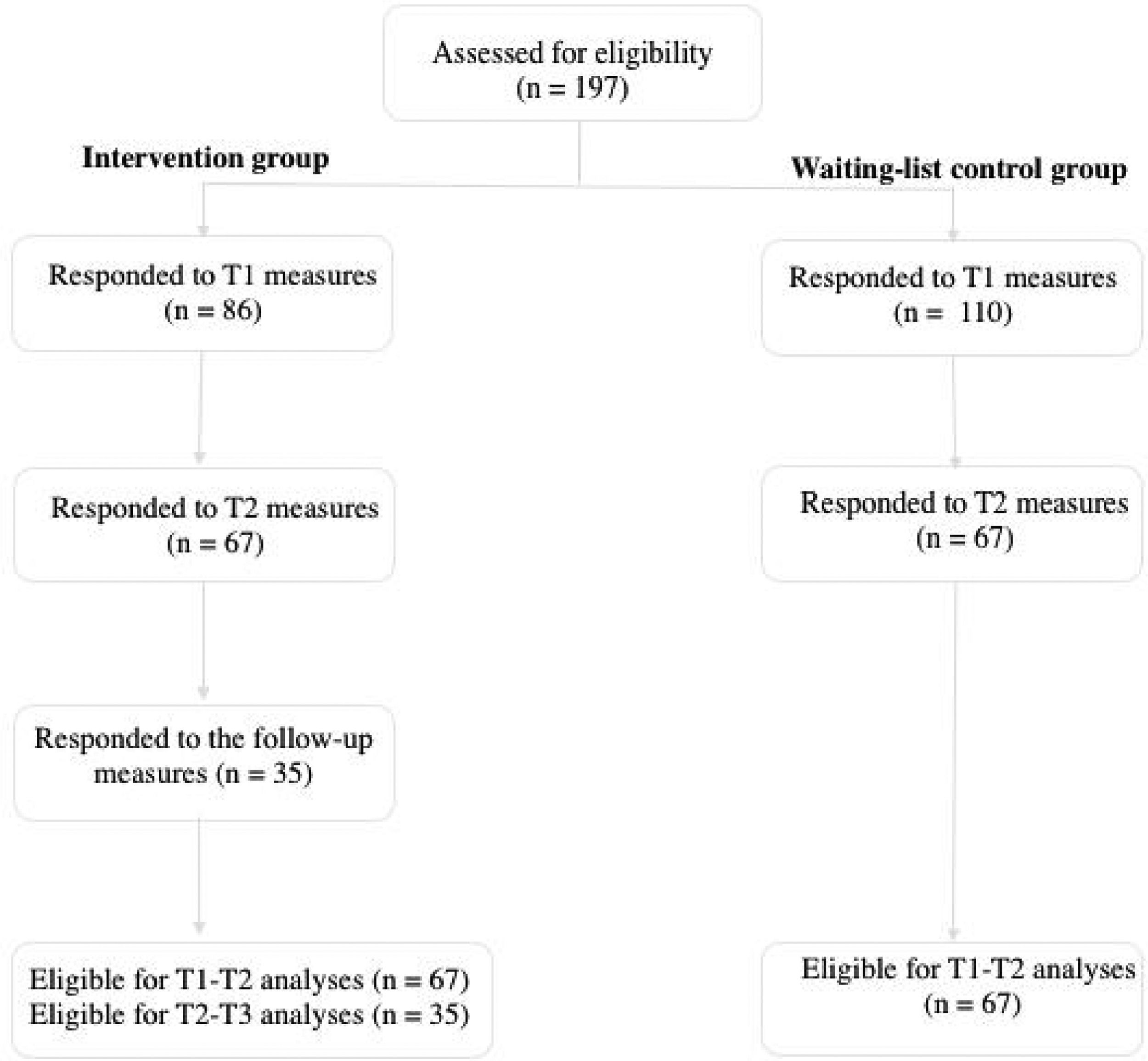
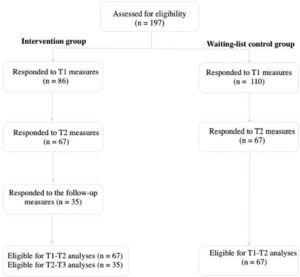
Materials and methodsParticipantsBased on a power analysis calculated with G* Power software the required sample size was of 158 participants (i.e., 79 participants for both CBSM and control groups). We have determined a medium effect size (f = 0.25) with 80% power for ANCOVA based on previous interventional studies for parental burnout (Bayot et al., under review; Brianda et al., 2020). In total, 196 parents participated in the study, out of which 134 (130 females and 4 males) were included in the analyses as they responded to at least T1 and T2 measures. The mean age of participants was 37.3 years (SD = 5.23), and the median number of children living in the same household was 2 (M = 1.88, SD = 0.876). The inclusion criteria for participating in the study were: (a) to be a parent of at least one child living in the same household, (b) being over 18 years old, and (c) having accepted an informed consent for participation in the study. Participants did not receive any financial reward for their participation in the study and they participated in the CBSM group for free. Flowchart diagram of participation rate at pre-, post-, and follow-up measures is presented in Fig. 2.
The study received approval from the national ethical committee board (No.: 19.02.06.44810) and was preregistered on the Open Science Framework: https://osf.io/f5c7b/?view_only=22472fb65a344e7cb52e948d2b39e0ff.
Regarding the allocation procedure, we did not implement a randomised controlled trial procedure because of the ethical implications related to the risks associated with parental burnout (i.e., increased risk of suicide, child abuse and neglect; Brianda et al., 2020; Mikolajczak et al., 2018). Consequently, parents willing to participate in the intervention could immediately attend to the intervention group. Participants were recruited in ecological context through the community-based organisations: they were not followed by doctors and had no other treatment proposed. The control group comprised parents who could not participate in a group at a given time (waiting-list), and who expressed their interest to participate in subsequent intervention groups. New CBSM groups were proposed every 8-weeks. Therefore, participants from the waiting-list control group were invited to participate in the intervention group after T2 measures. We decided not to randomly assign participants to the CBSM and control groups as this might have resulted in increased risk of drop-out from the study. Parents from the waiting-list control group were those who could not attend the intervention immediately: they would therefore have been excluded from the study before the beginning of the intervention if they had been assigned to the experimental group. Similarly, it is possible that parents who were available to attend the intervention at the moment of signing in for the study but would have been assigned to the control group would not be available to attend the intervention 8 weeks later. Thus, from a clinical and ethical perspective fewer parents would have received the intervention if the study had been randomised.
Prior to the assignment to an intervention group, participants were informed about the purpose and protocol of the study during an information meeting. All participants received a written information sheet and signed the informed consent. Participants were informed about their right to withdraw from the study at any moment. Participants signed-up to an intervention group depending on their availabilities: different time slots were proposed every 10 weeks. Participants who could not participate in the intervention were assigned to the waiting-list control group and invited sign up to one of the newly proposed groups.
The CBSM parenting intervention groups consisted of eight sessions delivered by two trained psychologists once a week over an 8-week period. The duration of each session was 2 h and 30 min. The psychologists delivering the intervention had previous experience in group therapy and completed a three-day CBSM training course, they also had previous experience of working with parents. Participants from the intervention group were asked to respond to an online questionnaire via a Qualtrics™ online software before (T1) and after (T2) the intervention as well as at three-month follow-up (T3). Participants from the control group responded only to the T1 and T2 questionnaires and were invited to participate in the CBSM intervention directly after the T2 measure.
The intervention sessions were video recorded to enable fidelity checks conducted by the developer of the French intervention, focusing on adherence to the treatment manual. Any deviations were discussed and corrected in subsequent sessions.
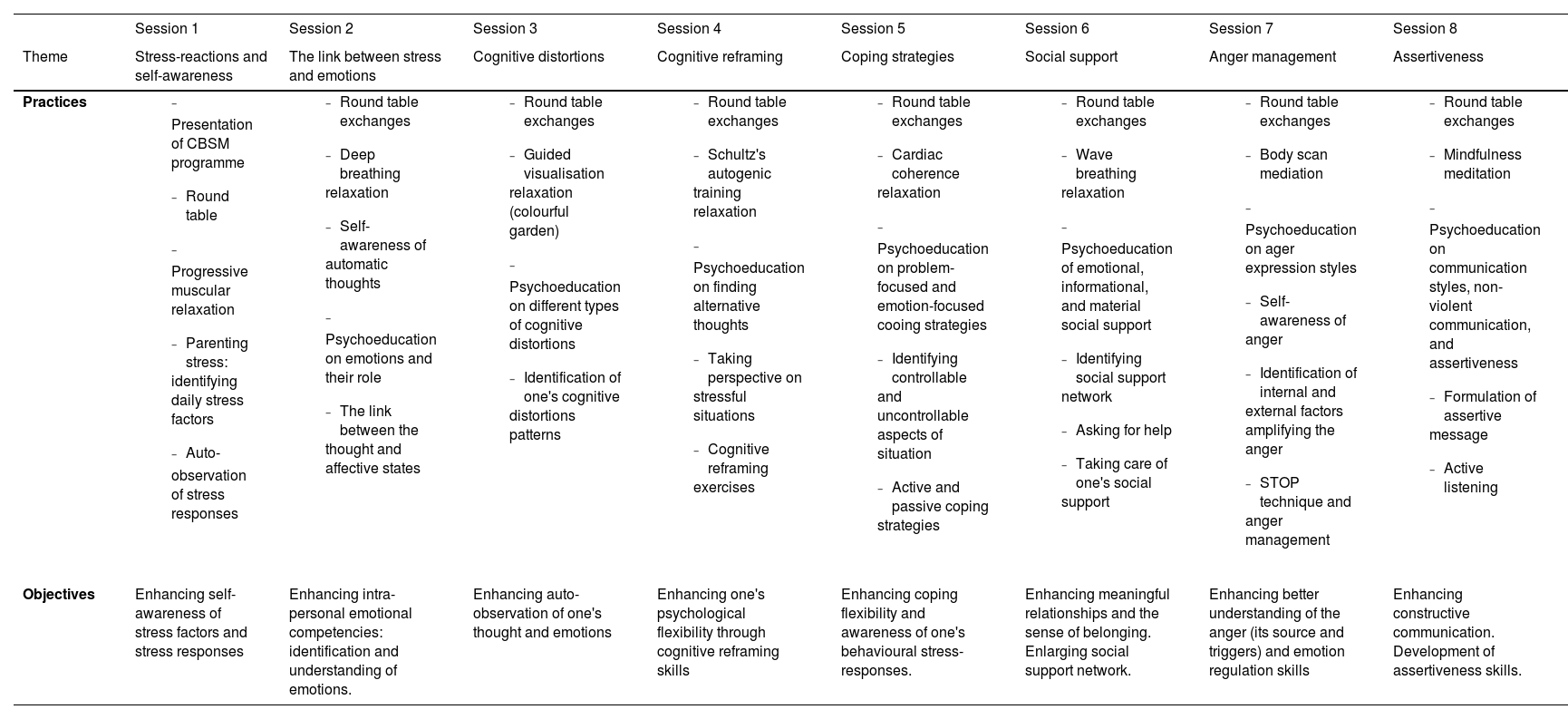
InterventionWe translated the CBSM protocol (Antoni et al., 2007) to the French language and adapted the psycho-educative content of each session and proposed practices to the context of parenting stress and parental burnout based on recommendations of Roskam and Mikolajczak (2018). The final intervention protocol consisted of eight weekly sessions, see Table 1. Each session focused on a different stress management competency and followed a structured plan starting with a roundtable exchange between participants and therapist about participants’ experiences during the week, as well as their achievements and difficulties in the application of relaxation and other newly learned skills in the family context. Following this, participants were invited to a guided relaxation exercise and to share their experience of whether the practice was perceived as enjoyable or difficult. The third part of each session consisted of a psycho-education training during which participants were introduced to a series of stress management skills (e.g., cognitive distortions, cognitive reframing, coping strategies, anger management, assertiveness). The psycho-education part consisted also of structured exercises based on participants’ individual experiences to put the theory into practice using real life situations. The last part of each weekly meeting was the summary of the session's content and planning self-monitoring and relaxation exercises to practice at home in between the sessions. Each session ended with a roundtable exchange about the experience that each person had during the session. The additional two follow-up sessions were proposed: one month and three months after the end of the intervention. The follow-up sessions consisted of round table exchanges between participants and the therapist and the guided relaxation.
Overview of the CBSM programme protocol.
To assess the intervention's effectiveness, we used self-administrated questionnaires measuring severity of parental burnout and stress symptoms, abstract ruminations, self-kindness, and emotion regulation before, after, and at 3-month follow up. We also measured socio-demographic characteristics (i.e., age, gender, number and age of children, family and professional situation, level of education) and the motivation to participate in the programme.
Parental burnoutThe severity of parental burnout was measured using the Parental Burnout Assessment (PBA, Roskam et al., 2018). PBA is 23- item scale measuring four dimensions of parental burnout: (a) physical and emotional exhaustion (e.g., Item 3: “I feel completely run down by my role as a parent”), (b) emotional distancing from the child (e.g., Item 20: “I'm no longer able to show my children how much I love them”), (c) the loss of fulfilment and pleasure in parental role (e.g., Item 11: “I don't enjoy being with my children”), and (d) contrast in the perception of parental self (e.g., Item 17: “I'm ashamed of the parent that I've become”). The responses are assessed on a 7-point Likert scale: never (0), a few times per year or less (1), a few times per month (2), once per month or less (3), once per week (4), a few times per week (5), every day (6). The scale enables the assessment of the risk and severity of parental burnout using five cut-off scores (Roskam et al., 2018). The total score below 30 is considered as no risk of parental burnout. Scores between 30 and 45 are considered as a low risk to parental burnout, those between 46 and 60 are considered as a moderate risk to the parental burnout, those between 61 and 75- the high risk of parental burnout, and scores above 75 are considered to indicate severe parental burnout. In the present study, the total scale had an excellent internal consistency with a Cronbach's 2at T1, α = 0.98 at T2, and α = 0.97 at T3.
StressThe severity of stress symptoms was measured with one dimension of Depression, Anxiety, Stress Scale (DASS-21; Lovibond & Lovibond, 1995). The DASS-21 contains three 7-items subscales measuring the emotional states of depression, anxiety, and stress over the past week. The items are rated on 4-point Likert scale from 0 (“Did not apply to me at all”) to 3 (“Applied to me very much or most of the time”). The stress subscale assesses the difficulty to relax (e.g., Item 12: “I found it difficult to relax”), agitation and over-reactivity (e.g., Item 14: “I was intolerant to anything that kept me from getting on with what I was doing”). In the present study, the stress sub-scale showed a good internal consistency with a Cronbach's α = 0.86 at T1 and α = 0.89 at T2.
Abstract ruminationsThe frequency of abstract ruminations was evaluated with 8-items subscale of Mini-Cambridge Exeter Repetitive Thought Scale (Mini-CERTS; Douillez et al., 2014). Mini-CERTS is 16-item questionnaire measuring abstract and concrete ruminations with 8 items for each dimension. The responses are rated on 4-point Likert scale from (1) almost never to (4) always. Abstract ruminations are unconstructive repetitive thoughts which are often overgeneralised to many different topics. Whereas concrete ruminations are considered as constructive repetitive thoughts as they are focused on a specific problem and can enhance the problem solving strategies. In this study, the subscale showed satisfying internal consistency with Cronbach's α = 0.66 at T1 and α = 0.72 at T2.
Self-KindnessSelf-kindness was measured with the Unconditional Self-Kindness scale (USK; Smith et al., 2018). The USK is a 6-item scale assessed using a series of 7-point Likert items, with scores ranging from 0 (not at all) to 6 (a great deal) measuring the ability to be kind to oneself in challenging situations e.g., in the context of rejection, failure or mistake, awareness of personal flaws and imperfections. The examples of items are: Item 1: “How much are you patient and tolerant with yourself when you are criticized or rejected by another person”? Item 6: “How much are you loving and kind to yourself when you fail or make a mistake”? The higher scores show the higher levels of unconditional self-kindness. The scale showed excellent internal consistency with a Cronbach's α = 0.92 at T1, α = 0.94 at T2.
Emotion regulationEmotion regulation was measured with intrapersonal emotion regulation dimension of The Profile of Emotional Competence scale (PEC, Brasseur et al., 2013). The PEC scale measures five dimensions of emotional competencies, i.e., identification, expression, comprehension, regulation, and utilisation of emotions both on intrapersonal and interpersonal levels. The intrapersonal emotion regulation subscale consisted of 5 items assessed on a five-point Likert scale from 1 (the statement does not describe me at all) to 5 (the statement describes me very well). The examples of items are, Item 12: “I easily manage to calm myself down after a difficult experience”; Item 15: “When I am sad, I find it easy to cheer myself up”; Item 37: “I find it difficult to handle my emotions”. In this study, the scale showed a suboptimal internal consistency at time 2 with a Cronbach's α = 0.69 at T1 and α = 0.65 at T2.
Data analysesAll collected data were processed using the Jamovi statistical software (The jamovi project, 2020). We applied one-way ANOVA to examine the differences in age between participants from the intervention and the control groups. We also applied χ² tests for independence on categorical and discrete variables: gender, family situation, professional occupation, education level, and number of children. The prevalence of parental burnout in intervention and control groups was calculated using five cut-off scores following Roskam et al. (2018) recommendation.
To test our main hypothesis comparing the effects of the control group with the CBSM intervention on parental burnout at T2 we applied ANCOVA with the PBA score at T1 as covariate to statistically control for the effect of the pre-test differences between the groups. To test our second hypothesis that the results of the intervention were maintained within CBSM group at 3 months follow-up we applied one sample t-tests applying Helmert contrasts within the intervention group. The first contrast compared unilaterally the baseline measure (T1) with the post-intervention (T2) and 3-months follow-up measures (T3). The second contrast compared unilaterally the 3 months follow-up (T3) with the post-intervention measure (T2). The choice of the analyses was guided by the fact that we could not apply repeated measures ANOVA with three measurement times as we assessed the follow-up measures only in the CBSM group: participants from the control group could assign to the intervention group directly after the T2 measure. To test our third hypothesis that within the intervention group the decrease of parental burnout between T1 and T2 would be associated to the increase of unconditional self-kindness and emotion regulation as well as the decrease of stress and abstract ruminations we conducted correlation analyses on centred variables representing the difference of scores between T2 and T1 (ΔT2-T1) in: (1) parental burnout, (2) stress, (3) abstract ruminations, (4) unconditional self-kindness, and (5) emotion regulation.
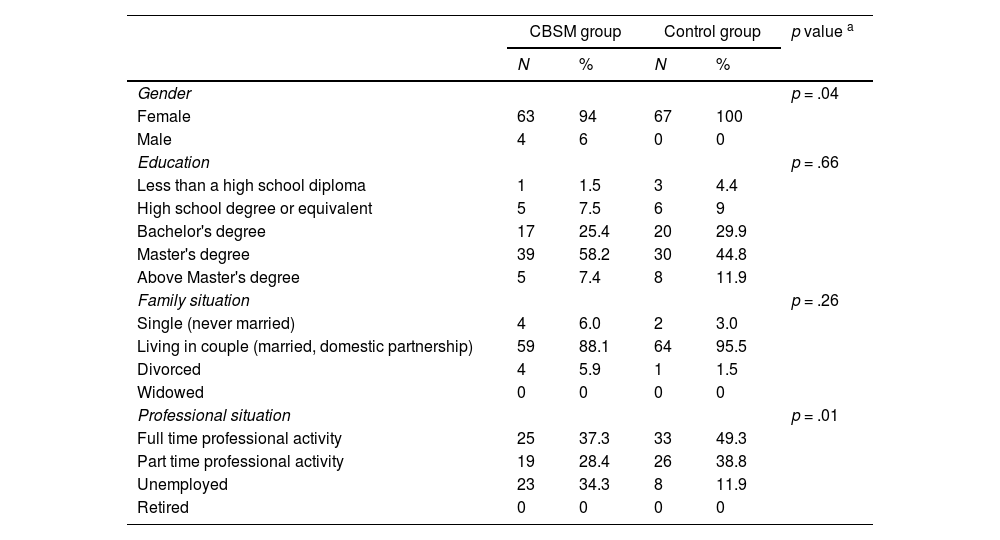
ResultsDescriptive analysesThe socio-demographic characteristics of the participants are presented in Table 2. The results of one-way ANOVA - F(1, 131) = 6.93, p = .01, η2p = 0.05 - showed that participants from the intervention group (M = 38.45, SD = 5.35) were on average older then participants from the control group (M = 36.12, SD = 4.89). There was also a statistically significant difference between the groups in gender - χ²(1) = 4.12, p = .04, V = 0.18, and professional occupation - χ²(2) = 9.45, p = .01, V = 0.27. There was no statistically significant difference between the groups in terms of family situation - χ²(2) = 2.67, p = .26, V = 0.14, education level - χ²(5) = 3.32, p = .66, V = 0.16, and number of children - χ²(5) = 4.40, p = .49, V = 0.18. A total of 35.8% of the participants had one child under 18 years old (N = 48), 46.3% of the participants had two children (N = 62), 14.2% had three children (N = 19), 3.62% had more than three children (N = 5). In addition, 15.7% of the participants reported a current diagnosis of a child's chronic illness or developmental problems, while 3.7% of the parents reported a past problem.
Demographic characteristics of participants.
| CBSM group | Control group | p value a | |||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Gender | p = .04 | ||||
| Female | 63 | 94 | 67 | 100 | |
| Male | 4 | 6 | 0 | 0 | |
| Education | p = .66 | ||||
| Less than a high school diploma | 1 | 1.5 | 3 | 4.4 | |
| High school degree or equivalent | 5 | 7.5 | 6 | 9 | |
| Bachelor's degree | 17 | 25.4 | 20 | 29.9 | |
| Master's degree | 39 | 58.2 | 30 | 44.8 | |
| Above Master's degree | 5 | 7.4 | 8 | 11.9 | |
| Family situation | p = .26 | ||||
| Single (never married) | 4 | 6.0 | 2 | 3.0 | |
| Living in couple (married, domestic partnership) | 59 | 88.1 | 64 | 95.5 | |
| Divorced | 4 | 5.9 | 1 | 1.5 | |
| Widowed | 0 | 0 | 0 | 0 | |
| Professional situation | p = .01 | ||||
| Full time professional activity | 25 | 37.3 | 33 | 49.3 | |
| Part time professional activity | 19 | 28.4 | 26 | 38.8 | |
| Unemployed | 23 | 34.3 | 8 | 11.9 | |
| Retired | 0 | 0 | 0 | 0 | |
Note.
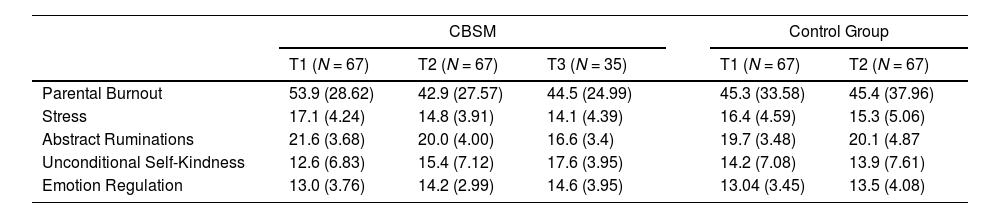
Regarding the prevalence of parental burnout in the experimental (CBSM) group, 22.4% of the participants did not present symptoms of parental burnout (total BPA score below 30), 22.4% were at low risk of parental burnout (total PBA score between 30 and 45), 19.4% of parents were at moderate risk of burnout (total PBA score between 46 and 60), and 35.8% of participants presented severe symptoms of parental burnout (total PBA score above 61). In the control group, 47.8% of participants did not present the symptoms of parental burnout (total BPA score below 30), a total of 13.4% were at low risk of parental burnout (total PBA score between 30 and 45), 11.9% of parents were at moderate risk of burnout (total PBA score between 46 and 60), and 26.9% of participants presented severe symptoms of parental burnout (total PBA score above 61). Parents from the intervention group (M = 53.9, SD = 28.6) presented on average a higher score of parental burnout at T1 then participants from the control group (M = 45.3, SD = 33.6). However, this difference was not statistically significant - F(1, 129) = 2.53, p = .11, η2p = 0.02. Table 3 presents the mean scores, standard deviations of the studied variables in the intervention and control groups.
Means, standard deviations of studied variables.
Note. Standard deviations are presented in brackets. T1, T2, and T3 correspond to pre-, post-, and follow-up measures.
To test our first hypothesis that compared to the control group CBSM intervention reduced the severity of parental burnout symptoms, we performed ANCOVA with PBA scores at T1 as a covariate to control for the difference of PBA scores at pre-test. Results indicated that when controlling for differences between pre-test scores, the CBSM group scored significantly lower on parental burnout severity (M = 42.90, SD = 27.60) than the control group (M = 45.40, SD = 38.00), with (F(2, 131) = 77.30, p < .00, and d = 0.41. These findings supported our first hypothesis.
To test our second hypothesis that the reduction in parental burnout scores was maintained within the intervention group at 3-month follow-up, we applied a one-sample t-test with Helmert contrast. The first contrast, testing our hypothesis, compared unilaterally the baseline measure (T1) with the post intervention (T2) and 3-month follow-up measures (C1 = 2*T1-T2-T3). The second contrast, supposed to be non-significant, compared (therefore bilaterally) the 3 month-follow up with the post intervention measure (C2 = T3-T2). The analysis showed a significant mean difference in PBA scores between T1 and T2, and T3 (Mdiff = 15.66, t(34) = 1.89, d = 0.32, 95%CI [−0.02, 0.66], p = .03), and statistically non-significant mean difference between T2 and T3 measures (Mdiff = −1.83, t(34) = 0.76, d = - 0.13, 95%CI [−0.45, 0.206], p = .23) which confirmed our second hypothesis.
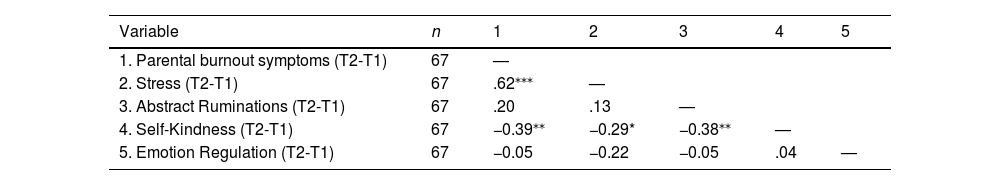
To test our third hypothesis that within the intervention group the decrease in parental burnout between T1 and T2 would be associated to the decrease in stress and ruminations, as well as the increase in unconditional self-kindness and emotion regulation we conducted correlations with centred variables (see Table 4). The findings suggested that the difference in parental burnout between T2 and T1 was significantly associated to the decrease in stress (r = 0.62, p < .001), and the increase in self-kindness (r = −0.39, p = .001). In addition, the increase in self-kindness was significantly associated with the decrease in stress (r = −0.29, p = .02). and abstract ruminations (r = −0.38, p = .002).
Correlations between the differences of scores (T2 -T1) in study variables amongst the CBSM group.
| Variable | n | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|
| 1. Parental burnout symptoms (T2-T1) | 67 | — | ||||
| 2. Stress (T2-T1) | 67 | .62⁎⁎⁎ | — | |||
| 3. Abstract Ruminations (T2-T1) | 67 | .20 | .13 | — | ||
| 4. Self-Kindness (T2-T1) | 67 | −0.39⁎⁎ | −0.29* | −0.38⁎⁎ | — | |
| 5. Emotion Regulation (T2-T1) | 67 | −0.05 | −0.22 | −0.05 | .04 | — |
Note.
This study aimed to evaluate the effectiveness of CBSM intervention for parental burnout reduction compared to a waiting-list control group. We evaluated the evolution of parental burnout symptoms before and after 8 weeks of the intervention. In addition, we compared the mean scores in parental burnout between T2 and the 3-month follow-up within the CBSM group. We also assessed the variables potentially implied in the reduction of parental burnout: the decrease in stress and abstract ruminations between T1 and T2, as well as the increase in unconditional self-kindness and emotion regulation between T1 and T2. The results of our study showed that CBSM intervention contributed to the reduction in parental burnout and that the decrease in parental burnout was associated with the decrease in stress and the increase in unconditional self-kindness.
Regarding the effectiveness of the CBSM intervention in terms of parental burnout severity reduction, we observed that after controlling for the pre-test differences between the intervention and control groups the scores of PBA were significantly lower in the CBSM group following the intervention. The comparison with a waiting-list control group showed that the decrease in parental burnout with a small effect size was due to the intervention's effects and not the spontaneous remission over time. Indeed, the CBSM intervention provides a complex range of tools for the management of cognitive, emotional, behavioural, physical, and social stress responses (see Table 1 and Fig. 1) which seem to contribute to the reduction of parental burnout and stress symptoms. Parental burnout is considered as a consequence of a chronic imbalance between stress factors and parental resources (Mikolajczak & Roskam, 2018) and the CBSM intervention significantly reduced parental burnout severity. These findings are also in line with previous research showing that CBSM intervention reduces stress symptoms across different populations including patients suffering from chronic illnesses (Antoni et al., 2000; Phillips et al., 2011) and pregnant women (Karamoozian et al., 2015). Beyond the previous research, the present study revealed the beneficial effects of the CBSM intervention also in terms of parental burnout severity reduction in parents from the general population. These findings give empirical evidence for the application of CBSM for parental burnout reduction and prevention. Although, the effect size of the intervention is small, the significative reduction of parental burnout severity among the parents at risk is an important implication. It remains fundamental to assess the effect size of the intervention depending on the severity of parental burnout. To our knowledge it is the first study evaluating the intervention for parental burnout prevention among the parents form the general population and not solely among the parents identified with severe burnout. It is possible that the effect size of the programme would be larger among participants with more severe parental burnout.
Moreover, the contrast analyses within the intervention group showed that whilst the parental burnout severity before the intervention at T1 significantly differed from post intervention (T2) and 3-month follow- (T3), there was no statistically significant difference between T3 and T2. This confirmed our second hypothesis that the effects of the intervention maintained at 3-month follow up. These findings can be explained by the fact that parents may continue to develop their stress management skills after the end of the intervention (Walton, 2014). This can be possible when the intervention targets psychological processes underlying parental burnout symptoms. The CBSM programme may have acted on numerous mechanisms of action such as negativity bias, repetitive negative thinking, self-critical thinking, perfectionism, or avoidance of expressing one's emotions and/or needs. In addition, during the 8 weeks of the intervention, parents developed their self-awareness skills, emotional competencies, and social support network which can also contribute to better stress management over time. It is possible that a person who found it difficult to express their needs or ask for help, for example, may find it easier with every positive experience (i.e., positive reinforcement). Therefore, the person's stress management skills may continue to increase following the intervention. This observation is in line with the results of the meta-analysis on parental burnout psychological interventions which showed that parental burnout severity continued to decrease even after the end of the interventions (Urbanowicz et al., under review).
Regarding our third hypothesis that the decrease of parental burnout at T2 would associated to with the decrease in stress and abstract ruminations, as well as by the increase in unconditional self-kindness and emotion regulation, the correlation analyses revealed significant associations of parental burnout reduction with stress reduction and the increase in self-kindness. Moreover, the increase in self-kindness was significantly associated with the reduction of abstract ruminations and stress. These findings are in line with previous research suggesting that self-compassion plays a protective role in parental burnout development (Paucsik et al., 2021). Indeed, self-compassion is likely to buffer against perfectionism (Mehr & Adams, 2016) which was identified in the literature as a risk factor for parental burnout (Kawamoto et al., 2018; Lin et al., 2021; Sorkkila & Aunola, 2020). Similarly, self-compassion has been shown to contribute to parental well-being (Neff & Faso, 2015), lower levels of parental burnout (Paucsik et al., 2021), and self-efficacy (Liao et al., 2021). Unconditional self-kindness is likely to play a similar protective role as self-compassion, as it reflects the capacity to be kind to oneself in challenging situations (e.g., in the context of rejection, failure, awareness of personal imperfections; Smith et al., 2018).
In contrast to previous findings on the protective role of emotional competencies and emotional intelligence in the context of parental burnout (Bayot et al., 2021; Lin et al., 2021; Mikolajczak et al., 2018), the findings of our study did not confirm our last hypothesis that reduction of parental burnout would be mediated by increases in emotion regulation competencies. There are two possible explanations for the discrepancy between the findings of our study and previous research. First, emotion regulation as a trait is one's ability to apply an adaptive emotion regulation strategy in emotional demanding situations (Brasseur et al., 2013). The 8-week period of time may not be long enough to achieve a significant change in participants’ emotion regulation capacity. Second, in our study we focused on intrapersonal emotion regulation traits which constitute only one dimension of emotional competencies (Brasseur et al., 2013). This may suggest that other emotional competencies (i.e., emotion identification, expression, comprehension, and utilisation) could be involved in parental burnout to a larger extent than intrapersonal emotion regulation skill alone. Indeed, emotional competencies describe a wide range of intra- and inter-personal skills which may buffer against or predict parental burnout on different levels (Lin et al., 2021). According to Lin et al. (2021) research should evaluate the independent effects of each dimension of emotional competencies while systematically controlling for the effects of others. Further studies are necessary to identify which emotional competencies should be targeted by psychological interventions.
In addition, the results of our study are not consistent with previous findings regarding the role of abstract ruminations in the development and maintain of parental burnout. Indeed, (Paucsik et al., 2021) identified abstract ruminations as a risk factor for parental burnout. Whereas in our study the decrease in parental burnout did not seem to be directly associated with the decrease in parental burnout. This discrepancy can be potentially explained by the fact that the decrease in abstract ruminations between T1 and T2 within the intervention group was not sufficiently important to significantly contribute to the reduction of parental burnout. As illustrated in Table 3 the scores of abstract ruminations continued to decrease at T3 (at three-month follow up). Therefore, the role of abstract ruminations can be potentially more important in the long-term perspective. In addition, the decrease in abstract ruminations was associated with the increase of self-kindness (see Table 4) which in can indirectly explain the reduction in parental burnout severity in the CBSM group.
The findings of this study should be interpreted with caution, as the study presents several limitations. First, the sample comprised mostly mothers (97%). A similar issue was identified in other studies on parental burnout, in which the participation of mothers was significantly higher compared to fathers (Brianda et al., 2020; Paucsik et al., 2021; Sorkkila & Aunola, 2020). Future research should assess to what extent the findings of this study can be generalised to the population of fathers.
Second, regarding the design of this study, we did not implement a randomised controlled trial procedure because of the ethical implications related to the risks associated with parental burnout (i.e., increased risk of suicide, child abuse and neglect; Brianda et al., 2020; Mikolajczak et al., 2018). Parents willing to participate in the intervention could immediately attend the group of their choice according to their availabilities (i.e., multiple schedules were proposed) and those who could not were assigned to the waiting-list control group. In our study, we aimed to assess the effectiveness of the CBSM intervention controlling for a potential natural remission over time in a control group. Based on previous evidence, randomly assigning participants to control and experimental groups was not necessary to meet this objective (Kowalski & Mrdjenovich, 2013). Indeed, assigning parents willing to immediately participate in the intervention group to the passive control group would rise both ethical and methodological problems (i.e., delaying the treatment and possibly losing the participants). However, given that in our sample participants were not randomly assigned to the intervention and control groups, there is a risk of a self-selection bias which can explain the significant difference in parental burnout severity levels at T1 between the CBSM and control group (Higgins et al., 2008). Indeed, the participants from the CBSM group presented significantly higher scores for parental burnout before the intervention compared to the parents from the control group. From the clinical perspective it means that parents who assigned to the intervention groups were these who needed parental support the most and those who benefited from the intervention in the first place: the distress related to the higher levels of parental burnout could underlie the motivation to seek help and participate in the intervention group. Parents with lower scores of parental burnout possibly felt less urgency to attend to the intervention group although they expressed their interest in the participation in the study. Future research should investigate the factors underlying the motivation to participate in the intervention and different profiles of parents participating in the programmes. Indeed, in interventional studies the person-centred approach may provide information about inter-personal characteristics which underlie the degree of adherence to the programme and its effectiveness (Bergman & Trost, 2006; Suárez et al., 2022).
In addition, we observed a significant drop-out in the number of responses to the online questionnaire at the end of the intervention at 3-month follow up. The response rates dropped from 86 to 67 at T2 and from 67 to 35 at T3. Drop out in post- intervention measurements has also been observed in other interventional studies on parental burnout (e.g., Anclair et al., 2018; Brianda et al., 2020; Masoumi et al., 2020). The loss of participants in the post-intervention measures can be explained by the fact that participants had already responded to the same online survey at T1 and it could be monotonous for them to respond for the second and third time. Moreover, participants did not receive any financial reward for their participation in the study. Potentially a financial compensation could increase the response rate as participants would receive a reward for investing their time. However, a financial reward could possibly bias the results of the study by increasing the self-selection bias (Hsieh & Kocielnik, 2016) and the external motivation to participate in the study (Sharp et al., 2006).
In conclusion, compared to the control group the CBSM intervention contributed to the significant reduction of parental burnout symptoms which was maintained at 3-moth follow-up. The findings of our study suggested that the decrease in parental burnout following the intervention was mediated by the decrease in stress and the increase in unconditional self-kindness.