A subset of recovered COVID-19 patients report persistent neurological symptoms. These include non-specific symptoms (e.g., headaches and fatigue) which were found to be affected by psychological processes in other disorders (e.g., post-concussion syndrome, PCS, after mild traumatic brain injury). The current study assessed the impact of diagnosis threat (i.e., information regarding the long-term neurological impact of COVID-19) and suggestibility on endorsed symptoms of both recovered patients and healthy controls. Method: Recovered patients (n = 90) and healthy controls (n = 210) described their cognitive functioning after being randomly assigned to: (a) Experimental group: These participants read an article that explored long-term neurological symptoms among COVID-19 survivors. (b) Control group: These participants read an article providing general information regarding the disease. Results: Recovered patients, but not healthy controls, endorsed more symptoms in the experimental condition compared to the control condition. Moreover, suggestibility was correlated with endorsement of symptoms. Conclusions: Post COVID-19 neurological symptoms may, at least partially, be affected by non-neurological factors such as diagnosis threat. Information regarding long-term effects of COVID-19 may skew reported symptoms with highly suggestible individuals particularly susceptible to these effects. Further research, however, is needed to validate and elaborate upon these initial findings.
Pacientes con COVID-19 recuperados informan síntomas neurológicos persistentes (e.g., dolor de cabeza y fatiga) que se vieron afectados por procesos psicológicos en otros trastornos (e.g., Síndrome postconmoción cerebral después de una lesión cerebral traumática leve). Se evaluó el impacto de la amenaza del diagnóstico (i.e., información sobre el impacto neurológico a largo plazo del COVID-19) y la sugestión sobre los síntomas respaldados tanto de pacientes recuperados como de controles sanos. Método: Pacientes recuperados (n = 90) y controles sanos (n = 210) informaron sobre su funcionamiento cognitivo después de haber sido asignados al azar a: (a) condición que exploró los síntomas neurológicos a largo plazo entre los sobrevivientes de COVID-19; (b) condición de control que proporciona información general sobre la enfermedad. Resultados: Pacientes recuperados, pero no los controles sanos, aprobaron más síntomas en la condición experimental que en la control. La sugestión se asoció con una mayor aprobación de síntomas. Conclusiones: Los síntomas neurológicos posteriores al COVID-19 pueden verse afectados, al menos parcialmente, por factores no neurológicos como la amenaza del diagnóstico. La información sobre los efectos a largo plazo de COVID-19 puede sesgar los síntomas informados en individuos altamente sugestionables. Se necesitan más investigaciones para validar y desarrollar estos hallazgos iniciales.
The Coronavirus Disease 2019 (COVID-19) outbreak constitutes a public health crisis at the international level (Lai, Shih, Ko, Tang, & Hsueh, 2020). Its symptoms include, among others, neurological deficits which may persist over time (Montalvan et al., 2020). For example, a subset of patients report symptoms such as dizziness, headaches, fatigue, and anosmia well after their initial recovery phase (Goërtz et al., 2020). This long-term cognitive dysfunction, a phenomenon termed Post COVID-19 Neurological Syndrome (PCNS), has drawn increased attention from researchers (Ritchie, Chan, & Watermeyer, 2020; Wijeratne & Crewther, 2020). As well as specific symptoms (e.g., anosmia), PCNS is associated with non-specific symptoms such as headaches, fatigue, and attentional impairment (Chen et al., 2021). These symptoms are common to many neuropsychiatric disorders and are also prevalent in the healthy population (Voormolen et al., 2019). Importantly, they are affected by non-neurological factors such as negative expectations regarding disease outcome and recovery. More specifically, 'diagnosis threat' refers to the impact of negative expectations on complaints regarding cognitive functioning and actual performance in neuropsychological tests (Suhr & Gunstad, 2002). For example, exposure to diagnosis threat significantly decreased memory performance of individuals with acquired brain injury (Fresson et al., 2019), a factor that was suggested to influence the persistence of symptoms in a minority of patients (i.e., post-concussion syndrome, PCS; Polinder et al., 2018).
We have limited understanding of PCNS at present and the factors that may contribute to its persistence. However, as diagnosis threat impacts the reporting of non-specific neurological symptoms in other disorders, there is value in assessing whether it may also impact such reports by recovered COVID-19 patients. Therefore, we randomized recovered COVID-19 patients and healthy controls to either diagnosis threat condition (i.e., participants received information regarding the neurological symptoms associated with PCNS) or control condition (i.e., participants received general information regarding COVID-19) as part of the current study. They then reported symptoms of cognitive dysfunction. As well as manipulating diagnosis threat, we also assessed the participants' suggestibility. The latter is defined as a communication process resulting in the acceptance of a proposition despite the absence of logically adequate grounds for its acceptance (Gudjonsson, 1987). Importantly, suggestibility may be a key factor in explaining the effect of diagnosis threat. For example, highly suggestible participants experienced a greater decrease in performance following instructions that likely activated diagnosis threat (Carter-Allison et al., 2016). Relatedly, these individuals may be especially prone to report higher levels of cognitive dysfunction, particularly in contexts that reinforce their beliefs in these impairments (Delis & Wetter, 2007). We hypothesized that: (a) Participants, particularly recovered COVID-19 patients, will report greater cognitive dysfunction in the diagnosis threat condition compared to the control condition. (b) Suggestibility will be significantly correlated with reported cognitive dysfunction. (c) Suggestibility will moderate the relationship between diagnosis threat and reported cognitive dysfunction.
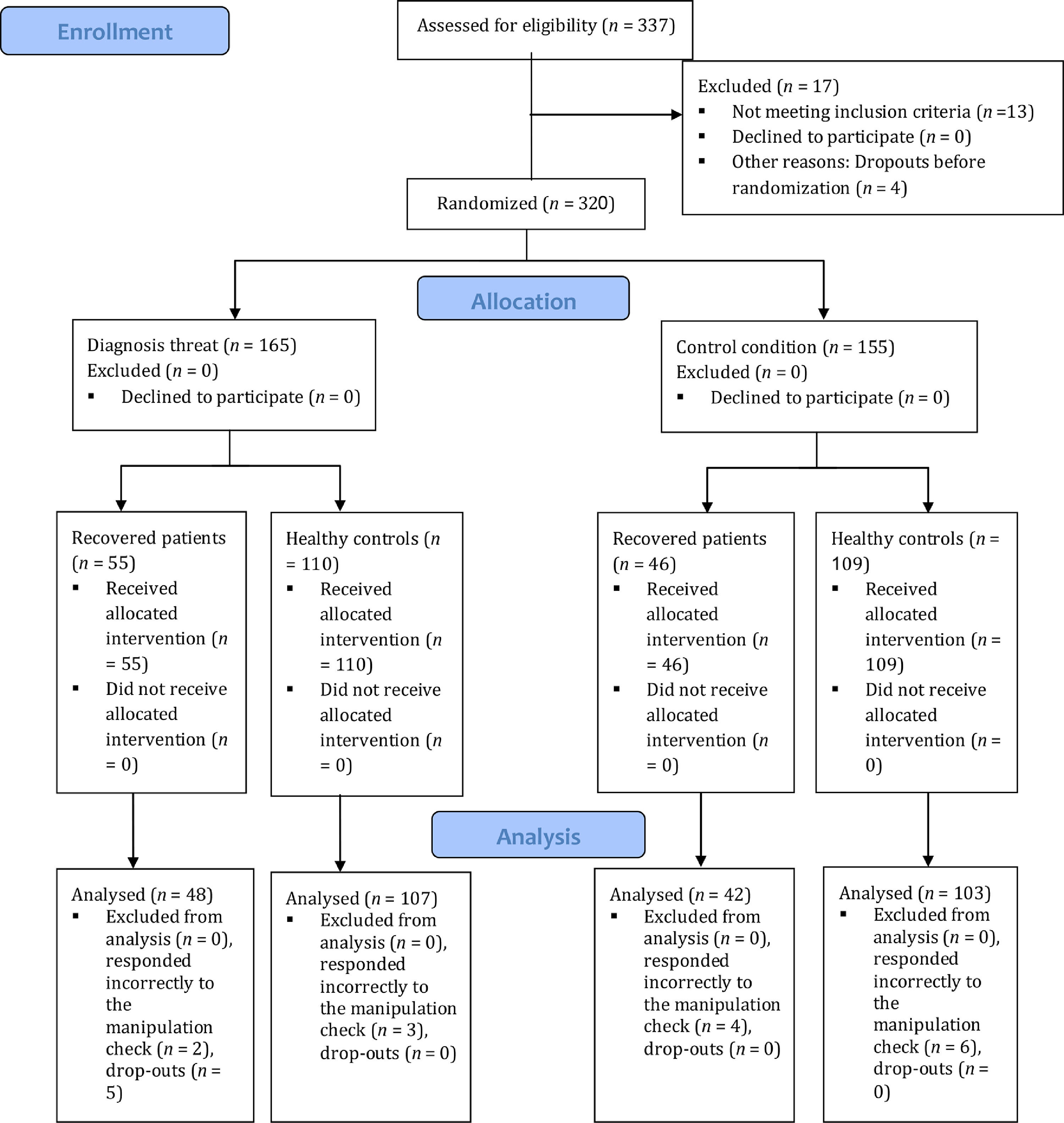
MethodParticipantsAdult (i.e., ≥ 18 years old) native Hebrew speakers participated in the study (N = 337). The participants were recruited via social media forums devoted to COVID-19 and through Ariel University's experimental bulletin board. The latter were undergraduate students who received course credit for participating in the study. Those who were still ill were excluded (n = 13) and data of 24 additional participants who did not complete the survey or responded incorrectly to the manipulation check (see procedure subsection) were not analyzed (final N = 300, n = 90 recovered patients, n = 210 healthy controls). See CONSORT diagram (Figure 1).
MaterialsCognitive failures questionnaire (CFQ). A self-report scale that ranks cognitive failures in daily life, such as attention lapses and memory problems (Broadbent et al., 1982; Wilhelm et al., 2010). It consists of 25 items which indicate how often the participant noted a certain problem, with scores ranging from 0 (never) to 4 (very often). Total score served as its outcome measure (0–100). The CFQ has good internal consistency (internal consistency coefficient, ICC = .89; Broadbent et al., 1982) and test-retest reliability (Bridger et al., 2013). Correspondingly, Cronbach's α in the current study was .92. Regarding validity, the CFQ is significantly correlated with other measures of subjective cognitive complaints (e.g., r = .62 with Reason's absent- mindedness questionnaire; Broadbent et al., 1982) and was described as a validated measure of real-world daily cognitive lapses which provides wider coverage than similar measures (Carrigan & Barkus, 2016).
Short suggestibility scale (SSS). A 21-item scale used to measure internalization and acceptance of messages. The SSS is a shorter version of the 95-item Multidimensional Iowa Suggestibility Scale (MISS; Kotov et al., 2004). Its items are related to consumer and psychological suggestibility, persuasiveness, peer conformity, and physiological reactivity (e.g., “I get a lot of good practical advice from magazines or TV”). Each item is rated from 1 (not at all or very slightly) to 5 (a lot). Total score served as the outcome measure (21–105). The scale had high internal reliability (rs = .86–.89) and was deemed reliable based on two different samples (n = 712 and n = 638; Kotov et al., 2004). Correspondingly, Cronbach's α in the current study was .91. The SSS is strongly correlated with the MISS (Kotov et al., 2004; Nitzan et al., 2015) and shows the expected associations with relevant variables among both healthy participants and clinical populations (e.g., overweight and obesity; Ray, Zachmann, Caudill, & Boggiano, 2020).
ProcedureThe study was conducted using the Qualtrics survey software (for a related study using the platform, see Nelson et al., 2020). Participants provided general demographic data. They were then requested to read an article and were notified that they will be later questioned regarding its content (i.e., a manipulation check). Afterwards, the participants were randomly assigned to one of two conditions, regardless of their current COVID-19 status (recovered patients vs. healthy controls): (a) Diagnosis threat: The article presented information regarding neurological symptoms following recovery from COVID-19. (b) Control: The article described factors that influence official policies regarding length of quarantines (see Appendix A). The articles were extracted from the online edition of “Israel Hayom”, a widely distributed Israeli daily newspaper. Both articles had the same headline and contained an identical number of words. The manipulation check consisted of two questions pertaining to the article. Participants were requested to read the article again if responding incorrectly. Any errors in the second administration of the manipulation check led to the exclusion of the participant's data. Participants then completed the CFQ, SSS, and medical questionnaires. The latter collected relevant medical data, including information related to COVID-19, and were based on recent publications (e.g., Menni et al., 2020). The study was approved by the Institutional Review Board (IRB) committee with all participants consenting to participate in the study.
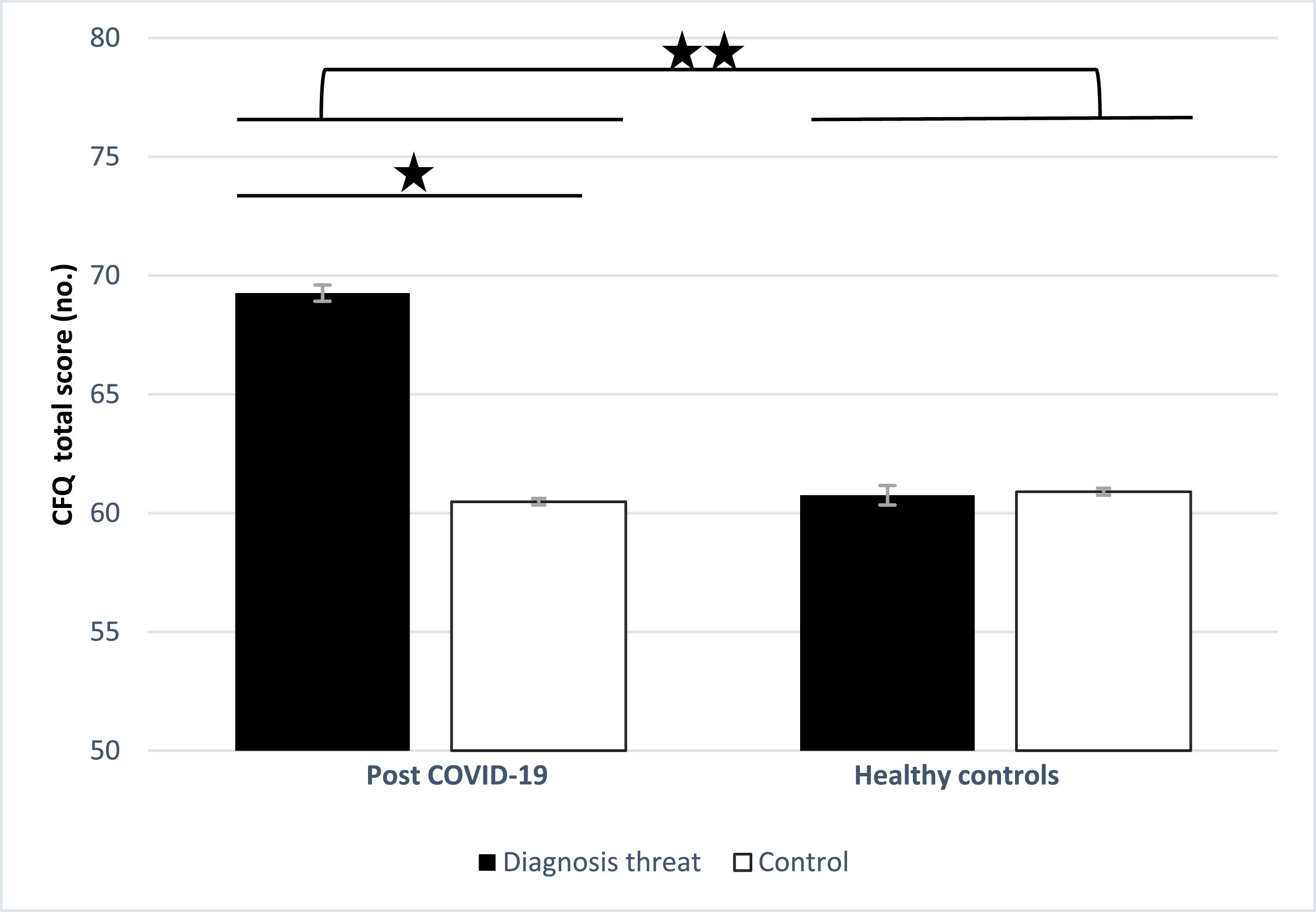
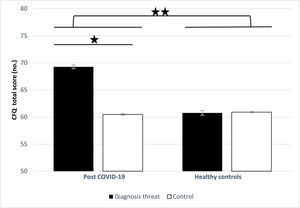
ResultsAnalyses of variance (ANOVAs) with a between-subjects factor of diagnosis threat (PCNS article or control article) and group (recovered COVID-19 patients or controls) was performed on cognitive complaints (CFQ total score). It indicated significant group and diagnosis threat main effects which were qualified by a significant group x diagnosis threat interaction [F(1, 296) = 4.68, p = .031, η2p = 0.16, 95% CI [0.80, 8.29]; F(1, 296) = 4.69, p = .031, η2p = 0.14, 95% CI [0.06, 7.55]; F(1, 296) = 4.93, p = .027, η2p = 0.17, 95% CI [60.93, 64.80]; respectively]. Among recovered COVID-19 patients, those in the diagnosis threat condition reported a larger cognitive impairment than those in the control condition, t(86) = -2.46, p = .016, d = 0.52, 95% CI [-16.40, -1.15]. In contrast, this difference was not significant among healthy controls, t(206) = 0.07, p = .939. See Figure 2. As the recovered COVID-19 patients and healthy controls differed in several variables (see Table 1), the analysis was repeated using these variables as covariates, either grouped together or in separate analyses. The findings of these analyses were like those of the original analyses and are therefore not presented.
Descriptive statistics and statistical analyses of demographic variables and suggestibility.
| Recovered COVID-19 patients | Healthy controls | Primary analyses | Post-hoc analyses | |||
|---|---|---|---|---|---|---|
| Diagnosis threat A | Control B | Diagnosis threat C | Control D | |||
| Parametric data | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Parametric analyses | |
| Age (years) | 38.60 ± 1.61 | 39.84 ± 1.76 | 27.54 ± 1.03 | 27.88 ± 1.05 | F(3, 296) = 23.22, p < .0001 | A / B > C / D |
| Education (years) | 15.26 ± 0.47 | 15.16 ± 0.53 | 13.26 ± 0.30 | 12.95 ± 0.31 | F(3, 291) = 10.03, p < .0001 | A / B > C/D |
| SSS total score (no.) | 43.15 ± 11.01 | 36.69 ± 9.23 | 47.54 ± 13.35 | 48.14 ± 12.41 | F(3, 296) = 9.94, p < .0001 | C / D > B Differences with A n.s. |
| Nonparametric data | Number | Number | Number | Number | Nonparametric analyses | |
| Gender (female / male) | 36/9 | 32/6 | 85/26 | 77/29 | χ2 (3) = 2.73, p = 0.43 | ________ |
| Birth country (Israel / other) | 34/11 | 33/5 | 102/9 | 97/9 | χ2(3) = 9.73, p < .021 | A / B > C / Da |
Note.
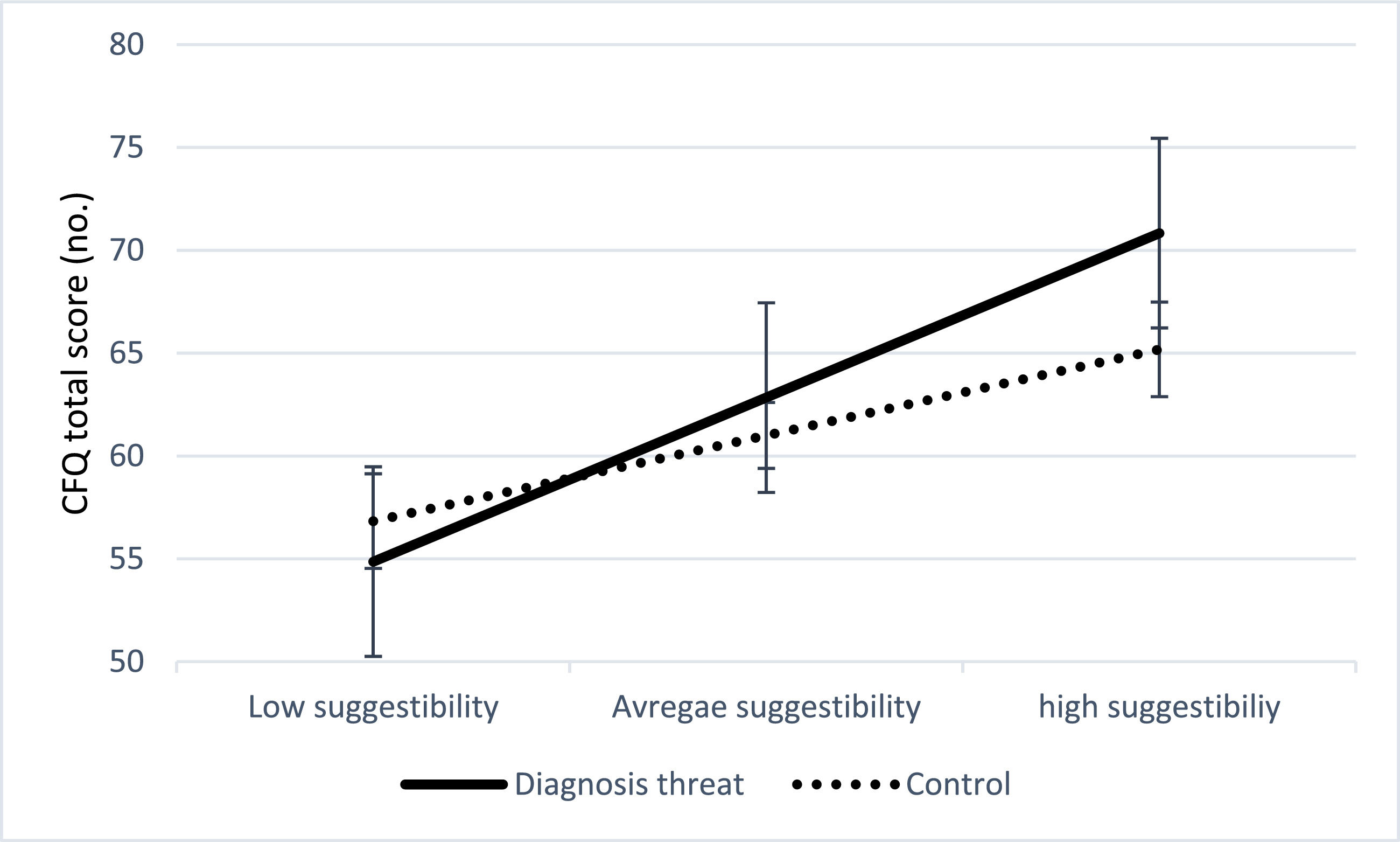
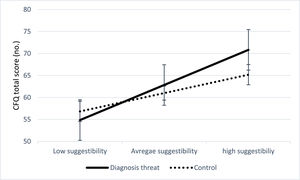
A Pearson product-moment correlation analysis between the extent of cognitive complaints (CFQ total score) and suggestibility (SSS total score) revealed a significant positive correlation, r = .40, p < .001. Hayes’ PROCESS module for SPSS (Hayes, 2018) was performed for each of 5000 bootstrapped samples. The combined effect of diagnosis threat and suggestibility on cognitive complaints (CFQ total score) was significant (R2 = .18, r = .42, F(3, 296) = 21.67, p < .001). Diagnosis threat in isolation from suggestibility was not a significant predictor (b = 1.83, t = 1.12, p = .261). Suggestibility, however, in isolation from diagnosis threat remained significantly correlated with cognitive complaints (b = 0.32, t = 3.52, p < .001, 95% CI [0.14, 0.50]). The interaction was also significant, indicating that suggestibility moderates the effect of diagnosis threat on the participants' cognitive complaints (R2 = .01, b = 0.29, t = 2.33, p = .02, 95% CI [0.04, 0.55]). Diagnosis threat was associated with the extent of cognitive complaints (i.e., CFQ total scores) among highly suggestible individuals (CFQ total score = 68.00 ± 0.13; b = 5.64, SE = 2.31, p = .015, 95% CI [1.08, 10.19]). In contrast, the effect was not significant among those with average (CFQ total score = 61.92 ± 0.09; b = 1.83, SE = 1.62, p = .261) or low suggestibility levels (CFQ total score = 55.84 ± 0.13; b = -1.97, SE = 2.30, p = .391). See figure 3.
Though not in the focus of the current study, we examined the contribution of the following demographic and disease-related variables: (a) Age: Pearson product-moment correlation analysis between suggestibility (SSS total score) and age revealed a significant inverse correlation, r = -.36, p < .001 (i.e., older participants tended to be less suggestible). However, entering age as a covariate in the analyses did not meaningfully alter the study's findings (not presented). (b) Gender: An independent-samples t-test revealed that women reported more cognitive impairment than men, t(298) = -3.27, p < .001, d = 0.41, 95% CI [-10.40, -2.42]. Note, however, that the groups did not differ significantly in gender distribution and entering gender as an independent variable in the analyses did not alter the study's findings (not presented). (c) Duration of COVID-19 disease: Suggestibility (SSS total score) and duration of COVID-19 disease were not significantly correlated (r = -.09, p = .401). Correspondingly, use of disease duration as a covariate did not alter the study's findings (not presented).
Finally, cognitive complaints (CFQ total score) were analyzed using analysis of variance (ANOVA) with between-subjects factors of gender, education level (≤12 years, 13-15 years, ≥16 years) and suggestibility (low, average, and high; i.e., the sample was divided according to participants' SSS total scores). The analysis revealed no significant gender, education level, or suggestibility main effects [F(1,298) = 1.66, p = .20; F(2, 297) = 0.94, p = .51; F(2, 297) = 1.16, p = .254; respectively]. Correspondingly, the suggestibility x gender, suggestibility x education level, and gender x education level interactions were not significant [F(2, 297) = 0.82, p = .66; F(4, 295) = 2.06, p = .81; F(2, 297) = 0.54, p = .82; respectively]. The gender x education x suggestibility interaction was also not significant [F(4, 295) = 1.60, p = .19].
General remarksAnalyses were conducted using the IBM Statistical Package for Social Sciences (SPSS) version 26.0 with a two-tailed p < .05 considered statistically significant in all analyses. Variables were assumed to be normally distributed after examining histograms (in accordance with Ghasemi & Zahediasl, 2012).
DiscussionThe current study contributes to the literature on diagnosis threat and suggestibility by focusing on the current COVID-19 pandemic. As expected, recovered COVID-19 patients reported more cognitive dysfunction than healthy controls, corresponding to recent studies (Goërtz et al., 2020). The study's key finding, however, was the effect of diagnosis threat; exposure to information regarding PCNS increased self-reported symptoms of cognitive dysfunction, but only among recovered COVID-19 patients. Diagnosis threat appears to be a specific manifestation of negative response expectancies (Kirsch, 1999), overlapping with the nocebo effect. The latter refers to the effects of negative expectations or anticipated future outcomes on state of health, with studies repeatedly indicating its widespread impact (Colloca & Barsky, 2020). Though speculative at present, the effect may stem from priming of memories related to everyday cognitive lapses, common in the general population (Voormolen et al., 2019). This possibility is in line with the expectation as etiology theory according to which PCS results from the linking of everyday complaints to a previous injury (i.e., a concussion) and thereby fueling expectations about recovery (Broshek et al., 2015). Furthermore, the current study implicates suggestibility in the susceptibility to the impact of diagnosis threat (Carter-Allison et al., 2016). More specifically, highly suggestible recovered COVID-19 patients were found to be particularly prone to the effects of diagnosis threat in their reporting of cognitive dysfunction. Self-reports of everyday cognitive functioning, a key element in the medical interview, may therefore be prone to the effect of diagnosis threat and related non-neurological factors (e.g., clinician driven iatrogenic processes; Niesten et al., 2020).
Limitations of the current study include: (a) COVID-19 patients were mostly recruited through social media forums devoted to the disease. Therefore, the sample may not be representative of the general COVID-19 recovering patient population (e.g., participants in the current study may be more anxious or experience more symptoms). (b) The study included undergraduate students which were mostly healthy, likely contributing to baseline differences between the recovered COVID-19 patients and healthy controls. Readers are therefore advised to focus on the comparisons between the patient groups (diagnosis threat vs. control condition) which represent a more rigorous research design (i.e., randomized controlled trial). (c) As noted by an anonymous reviewer, additional variables that may have impacted the findings were not assessed. For example, disease duration and its consequences, psychological variables (e.g., affective symptoms and patient resilience which was recently suggested as predictor of adaptive response to the COVID-19 pandemic and lockdown; Kocjan, Kavčič, & Avsec, 2021) and environmental factors (e.g., exposure to stress significantly increases suggestibility; Morgan III et al., 2020). Since the current study was constructed as a preliminary investigation, these variables – apart from disease duration which likely did not impact the findings – were not assessed. Consequently, it is advisable to include them in future studies.
The findings of the current study should be viewed as preliminary and await validation. Researchers are encouraged to include non-recovered patients and increase the sample size to enable more elaborate analyses and exploration of relevant variables. The effects of neuropathology on self-reported cognitive functioning, a link that was suggested in recent studies (Sun et al., 2021), is in this regard an important path that researchers can follow. This is in line with studies linking subjective cognitive complaints to neurological biomarkers (Cantero, Iglesias, Van Leemput, & Atienza, 2016; Liang et al., 2020; Llado-Saz et al., 2015). Researchers are also encouraged to assess whether cognitive complaints are manifested in objective tests and real-life functioning, as well as explore recovered COVID-19 patients' mental health during the disease and after recovery (Bueno-Notivol, 2021), including variables that predict resilience in unusual circumstances (e.g., positive mental health; Brailovskaia & Margraf, 2020). Relatedly, misinformation regarding COVID-19 has been the focus of increased concern (Merckelbach et al., 2018; Pennycook, McPhetres, Zhang, Lu, & Rand, 2020). Individuals may not accurately distinguish between scientific and pseudoscientific information, leading to serious medical complications (Pulido, Ruiz-Eugenio, Redondo-Sama, & Villarejo-Carballido, 2020), which stresses the need to further research. Exploration of demographic variables is also of importance. For example, age was correlated with suggestibility in the current study. Similarly, older adults show greater reduction in suggestibility when exposed to misleading information compared to younger adults (Huff & Umanath, 2018). Additionally, females reported more cognitive impairment than males in the current study, similar to earlier findings regarding general symptom endorsement in the context of COVID-19 (Fiorenzato et al., 2021). This likely did not confound the current study's conclusions, as the use of age as a covariate in the analyses did not alter the study's findings. Correspondingly, the groups did not differ significantly in gender distribution and gender did not alter the findings when entered as an independent variable. Nevertheless, this stresses the need for further research of these key demographic variables. Concepts related to suggestibility may also be the focus of research. For example, the 'being a patient effect' refers to the influence of group membership (i.e., knowledge that they are patients) on self-perception and cognitive functioning (Schwarz et al., 2018) and it would be of interest to investigate it with regard to COVID-19. Finally, strategies for using information in a beneficial manner should be investigated (e.g., offering psychoeducation on coping skills to manage patient expectations; Evers et al., 2021; Manai et al., 2019).
In summary, the current study demonstrates that information regarding COVID-19 may have clinical implications and, in certain cases, can increase subjective neurological complains due to the deleterious effects of diagnosis threat. Moreover, highly suggestible recovered COVID-19 patients may be particularly vulnerable to such an effect. It is advised that such factors be considered when assessing cognitive complaints of post COVID-19 patients (see, also, Evers et al., 2021). However, the current study's findings should be viewed as preliminary and await further research.
AcknowledgmentsThe research reported in this paper was completed as part of the first author's (D.W.) thesis (Rehabilitation Psychology, Ariel University, Ariel, Israel). We thank Mr. Tomer Elbaum for his aid in performing the statistical analyses.
Declarations of interestNone.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Note.aForeign countries are labeled green, yellow, or red by the Israeli Ministry of Health, based on the prevalence of COVID-19 in each country.The articles are composed of an identical number of words in their original Hebrew versions.