We aimed to investigate whether distress tolerance mediated the effects of mindfulness-based intervention (MBI) on anxiety and depression with two randomized controlled studies.
MethodIn Study 1, 374 participants with at least moderate emotional distress were randomized to an intervention group (N = 174) and a waitlist control group (N = 173). Mindfulness, distress tolerance, anxiety, and depression were measured at the pre-test, week 3, week 5, and post-test. In Study 2, 170 participants with emotional disorders were randomized to an intervention group (N = 86) and a control group (N = 84). The same variables were assessed at pre-test, weekly during the intervention, and post-test.
ResultsIn both studies, linear mixed effect models showed that compared to the control group, mindfulness, distress tolerance, anxiety, and depression significantly improved in the intervention group. Parallel process latent growth curve models showed that changes in distress tolerance mediated the effects of the MBI on changes in anxiety and depression. Random-intercept cross-lagged panel models found that distress tolerance temporally preceded depression, but not anxiety.
ConclusionsDistress tolerance is a potential mechanism underlying MBIs. Interventions targeting distress tolerance could be embedded in MBIs to enhance the intervention effects for emotional distress.
Anxiety and depression are common mental health disorders that affect millions of people worldwide (World Health Organization, 2021). Despite differences in symptoms, anxiety and depression are highly comorbid and share many etiological similarities (Barlow et al., 2010). In the past few decades, an abundance of studies has found that mindfulness-based interventions (MBIs) can effectively alleviate anxiety and depression symptoms (e.g., Creswell, 2016; Ju et al., 2022; Li et al., 2023a; Segal et al., 2020), with the effect on anxiety symptoms being comparable to that of anti-anxiety medications, but with fewer side effects (Hoge et al., 2023). Given the stable beneficial effects, an increasing number of researchers have delved into the mechanisms of change in MBIs for anxiety and depression (Maddock & Blair, 2021).
Distress tolerance (DT) is an important transdiagnostic factor underlying emotional disorders (e.g., Lass & Winer, 2020; Michel et al., 2016). It refers to an individual's ability to tolerate negative emotional states (Simons & Gaher, 2005). A recent study found that DT mediated the relationship between mindfulness and anxiety/depression at both between- and within-person levels (Li et al., 2023b). In addition, the mediation effects also existed in the time-lagged models. These findings suggests that DT could be a potential mechanism of change in MBIs for anxiety and depression. However, till now no study has directly examined this question. Therefore, it is important to determine the specific role of DT in the effects of MBIs for anxiety and depression.
According to Kazdin (2007), establishing a mediator of change in the underlying mechanism requires meeting several criteria. These include providing an explanation of how a mediator operates and integrating findings with the broader scientific knowledge base to contribute to the inferences (plausibility criterion), demonstrating strong associations between the intervention, mediator, and outcome (strong association criterion), with the mediator temporally preceding the outcome (temporal precedence criterion). Moreover, supporting evidence should derive from randomized controlled trials (RCT) that manipulate either the cause or the mediator (experimental manipulation criterion).
DT as the mechanism probably meets the plausibility criterion. Theoretically, individuals with low distress tolerance tend to perceive negative emotions as intolerable and resort to avoidance and suppression strategies, hindering habituation and self-efficacy development, ultimately leading to heightened anxiety and depression (Barlow et al., 2010; Ellard et al., 2010). MBIs may enhance distress tolerance by promoting present-focused attention, awareness, and acceptance of internal experience, including aversive sensations, cognitive appraisals (e.g., the distress is intolerable), and habitual response tendencies (e.g., thoughts, actions, sensations, and urges) to experiential distress (Lotan et al., 2013; Lynch & Mizon, 2011), ultimately leading to decreased anxiety and depression.
There is also experimental evidence contributing to the inferences of DT as the mechanism (e.g., Carpenter et al., 2019; Li et al., 2023b). DT is negatively correlated with anxiety and depression across diagnostic boundaries (Leyro et al., 2010; Yoon et al., 2018). Interventions targeting DT have shown potential in reducing depressive symptoms (Bornovalova et al., 2012), and an increase in DT after cognitive-behavioral therapies was associated with decreased anxiety and depression symptoms (McHugh et al., 2014). Regarding the relationship between MBIs and DT, a meta-analysis of 22 RCTs on mindfulness and acceptance-based interventions for affect intolerance/sensitivity found a small but significant effect on affect intolerance (including DT, Hedges' g = -0.37; Kraemer et al., 2020).
As for other criteria, there is a lack of evidence, especially regarding the temporal precedence criteria. This is a common challenge in the study of mechanisms underlying MBIs (Maddock & Blair, 2021). Previous mediation studies of MBIs often lack measures during the intervention, making it challenging to establish temporal precedence (Johannsen et al., 2022; Maddock & Blair, 2021). For example, in a review of 11 RCTs (Maddock & Blair, 2021), mindfulness, self-compassion, cognitive flexibility, and affect empathy (Kuyken et al., 2015; Morrison et al., 2019) were found to satisfy some of the criteria for mediation. However, these variables were only measured at pretest, posttest, and follow-up. While this sheds some light on the potential mediators of sustained treatment effects, it only provides partial support for the mediation tests. Therefore, to establish temporal precedence, we need to measure potential mediators and outcomes more frequently during the intervention and use these numerous assessment points in the data analysis (Kazdin, 2007; Kendall et al., 2017). To investigate whether DT is an important mechanism underlying MBIs, a more rigorous study design is needed, which combines RCT with multiple time-point measurements.
In summary, the current study aimed to examine whether DT satisfied the experimental manipulation, strong association, and temporal precedence criteria as a treatment mediator of MBI for anxiety and depression systematically. To accomplish this aim, 2 RCT studies were conducted. Study 1 was conducted in a sample of participants with emotional distress, using a 2 (Group: intervention vs. control) × 4 (Time: pre, week 3, week 5, post) study design mainly to examine the experimental manipulation and strong association criterion. Study 2 was conducted in a sample of clinical participants with anxiety and/or depression disorders, using a 2 (Group: intervention vs. control) × 8 (Time: pre, weekly, post) study design to mainly examine the temporal precedence criterion. We hypothesized that (H1) the intervention group would significantly improve compared to the control group in terms of mindfulness, DT, anxiety, and depression (experimental manipulation criterion); (H2) change of distress tolerance would mediate the association between an MBI, called Mindfulness Intervention for Emotional Distress (MIED; Li et al., 2023b; Liu, 2024) intervention (vs. control group) and improvements in anxiety/depression (strong association criteria); (H3) change of DT temporarily preceded the change of anxiety and depression (temporal precedence criterion).
Study 1MethodsParticipantsParticipants with high levels of self-reported anxiety and depression were recruited through social networks. The inclusion criteria included: (1) aged 18 to 65, and (2) with at least moderate anxiety and depression (score of the 10-item Kessler Psychological Distress Scale ≥ 22; K10; Kessler et al., 2002). The exclusion criteria included: (1) having previously participated in mindfulness-based programs longer than 8 weeks and/or currently meditating more than once a week; (2) having schizophrenia or psychotic affective disorders, current organic mental disorders, substance abuse disorders, and pervasive developmental disorders; (3) having a high risk of suicide.
Considering the power of 80 % and a significance level of 5 % on a two-sided test, a sample of at least 64 participants was needed per group (a total of 128) to estimate a medium between-group effect size of 0.5 (Cohen's d; Ju et al., 2022). Based on previous studies with a similar design, it was determined that a sample size of at least 150 was necessary for the more complex models (Cheong, 2011; Sunnhed et al., 2022).
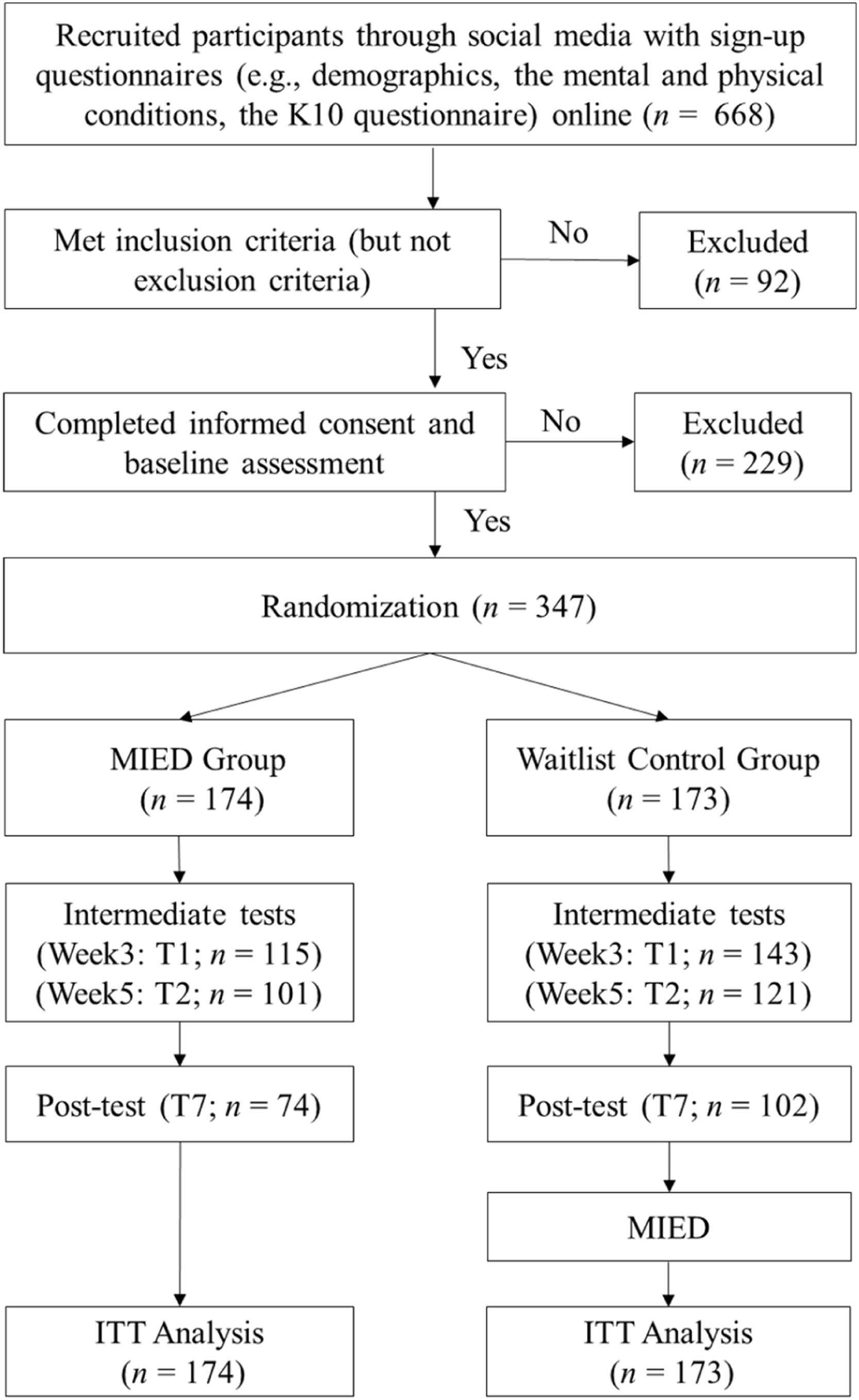
In total, 668 participants completed the sign-up questionnaires, of whom 92 were excluded for not meeting the study criteria or meeting the exclusion criteria, and 229 did not respond and/or finish baseline measures, leaving 347 participants included in the randomization (See Fig. 1).
ProceduresThe current study was a prospective, pre-registered, repeated-measure, RCT of comparing the MIED program against a Waitlist control. It was pre-registered in Chinese Clinical Trial Registry (http://www.chictr.org.cn/, Registration number: ChiCTR2200057398). Data were collected between March and May of 2022. The Association for Ethics and Human and Animal Protection of the School of Psychological and Cognitive Sciences of Peking Universit approved the study. As shown in Fig. 1, participants were invited to complete a sign-up questionnaire. Subsequently, they underwent screening based on the aforementioned inclusion and exclusion criteria. Participants who were eligible to participate then received an informed consent form, and upon signing, completed baseline measurements of mindfulness, DT, anxiety, and depression.
After completing the baseline questionnaire (T0), participants were randomly assigned to either a waitlist control group or the MIED group. A randomization list was created using a computer-generated random number sequence in Excel. The randomization was stratified by gender and age to ensure a balance of participants across the groups.
After randomization, the MIED group participated in the MIED program (Liu, 2024), while the waitlist control group did not receive any intervention during this period. At the end of the third week (T1) and fifth week (T2) of the intervention, and after the intervention (T3), both groups completed intermediate and post-intervention measurements, which included the same measures as the baseline assessment. Following the post-test, the waitlist control group received the MIED course. Participants did not receive any form of compensation or remuneration apart from the free course.
InterventionThe MBI used in the current study is the Mindfulness Intervention for Emotional Distress (MIED; Li et al., 2023a; Liu, 2024). The MIED targets the transdiagnostic factors underlying emotional distress (i.e., anxiety and depression), combining practices and rationales from traditional MBIs and the Unified Protocol for Transdiagnostic Treatment of Emotional Disorders (UP; Barlow et al., 2010). The MIED program can be delivered in a group (group-based MIED program) with guidance from a qualified teacher or delivered over the internet in a self-help version, which is effective in alleviating anxiety and depression for sub-clinical participants with emotional distress (Ju et al., 2022) and clinical participants with depression and/or anxiety disorders (Li et al., 2023a).
The eight-week MIED course comprised of eight sessions, each lasting 1.5–2.5 h. Each class consisted of 25–30 participants. The courses were led by 6 master students who majored in clinical psychology under the supervision of an expert in MIED teaching (Xinghua Liu, the corresponding author). All the teachers were MIED intern teachers, receiving training for at least one year. Homework was assigned using the internet-based MIED delivered via a mini app (Li et al., 2023a).
MeasurementsMindfulness The Chinese version of the Five Facet Mindfulness Questionnaire (FFMQ; Deng et al., 2011) was used to measure mindfulness. The FFMQ consists of 39 items, and each item is rated on a 5-point Likert scale (1 = never or very rarely true, 5 = very often or always true). Higher scores on the FFMQ indicate higher levels of mindfulness. In Study 1, the Cronbach's alpha of the FFMQ in the pretest was 0.85.
Distress tolerance The Chinese version of the Distress Tolerance Scale (DTS; You and Leung, 2011) was used to measure distress tolerance. The DTS contains 15 items, using a 5-point Likert scale (1 = strongly agree, 5 = strongly disagree). Higher scores on the DTS indicate a greater ability to tolerate distress. In Study 1, the Cronbach's α of DTS in the pretest was 0.91.
Anxiety The Chinese version of the Overall Anxiety Severity and Impairment Scale (OASIS; Liu et al., 2023) was used to measure anxiety levels and their interference. OASIS consists of 5 items that assess the frequency and severity of anxiety symptoms, functional impairment associated with these symptoms (i.e., impairment in school, work, home, and social life), and behavioral avoidance. In Study 1, the Cronbach's alpha of OASIS in the pretest was 0.85.
Depression The Overall Depression Severity and Impairment Scale (ODSIS; Liu et al., 2023) was used to measure depression levels and their interference. ODSIS consists of 5 items that assess the severity of depressive symptoms and the level of related functional impairment using a 5-point scale. In this study, the Cronbach's α of ODSIS was 0.94.
Statistical analysisAll the data were analyzed and reported following the CONSORT guidelines (Schulz et al., 2010). For all analyses, we conducted intent-to-treat (ITT) analyses (Tripepi et al., 2020), with all randomized participants included.
Experimental manipulation criterion of mediation: 2 (Group: MIED versus Waitlist) × 4 (Time: T0-T3) Linear mixed-effects model (LMM) in SPSS 26.0 was used to investigate the effects of the MIED program, with maximum likelihood as the method of estimation. Since analyses with raw data and imputed data yield similar results, here we only reported results with imputed data. Little's MCAR (Missing Completely at Random) tests showed that data were missed at random (all p-values > 0.05). Therefore, we used the expectation maximization (EM) imputation method (Newgard & Lewis, 2015) to deal with missing data. The fixed effect interaction terms between Group and Time were the primary parameters of interest, as they described whether the participants had differential changes from pre-to-post-treatment between groups. The model included random intercepts and identity covariance structure. For significant interaction effects, post-hoc analyses with Bonferroni correction were conducted (Bland & Altman, 1995). We report effect sizes as Cohen's d (Cohen, 1988), including between-group effect sizes at post-test and within-group pre-post effect sizes. Effect sizes are usually defined as small when d ≤ 0.2; medium when d ≥ 0.5; and large when d ≥ 0.8 (Cohen, 1988).
Strong association criterion of mediation: Parallel process latent growth curve model (PP-LGCM; Zhu et al., 2021) was used to examine whether the change of DT mediated the effects of the MIED program on anxiety/depression. Both latent intercepts and latent slopes were included in the model. The intercept factor loading was specified as 1, representing the value of the initial time point. The slope factor loadings followed an unspecified shape model (i.e., 0, *, 1), such that factor loadings were freely estimated. The latent slopes of distress tolerance and anxiety/depression were regressed on the Group (1 = MIED; 0 = waitlist) to establish a mediation model. Bootstrapping (n = 2000) was implemented in these analyses to obtain 95 % bias-corrected confidence intervals for the indirect effect estimates. If the values between the upper and lower confidence limits do not include zero, this indicates a statistically significant indirect effect (Preacher & Hayes, 2008).
Temporal precedence criterion of mediation: Cross-lagged panel models with random intercepts (RI-CLPMs; Hamaker et al., 2015; Sunnhed et al., 2022) were employed to examine whether the change of DT temporally preceded anxiety/depression. These models accounted for temporal stability (autoregressive effects) and individual trait differences (random intercept). Contrary to a standard cross-lagged panel model that fails to differentiate effects within and between individuals, this modified panel model provides more precise conclusions regarding the mutual influence of variables and the causal dominance of each variable (Hamaker et al., 2015). A lag of one was specified, indicating that DT and anxiety/depression predicted subsequent changes in each other 2 to 3 weeks later. Autoregressive and cross-lagged effects remained consistent over time. Since the objective of these models was to investigate changes within individuals, only participants randomized to the intervention group were included (Sunnhed et al., 2022).
For PP-LGCMs and RI-CLPMs, the adequacy of model fit was assessed utilizing the comparative fit index (CFI) and root-mean-square error of approximation (RMSEA) for the primary models. Generally, a model fit was deemed acceptable if the CFI exceeded 0.90 and the RMSEA was below 0.10, following a common guideline (e.g., Bollen & Curran, 2006).
ResultsParticipant flow and characteristicsA total of 347 participants from the MIED (n = 174) and the Waitlist group (n = 173) were included in the study (see Fig 1 for a detailed description of the participant flow). The sample consisted of mostly women (n = 300, 86.50 %), with an average age of 32.78 years old (SD = 9.12). The average length of education was 16.63 (SD = 2.53) and the average per capita monthly income was 12,832.37 RMB (SD = 21,924.44). Among them, 24.50 % were full-time students, 14.70 % were teachers, 7.5 % were technical personnel, and 53.31 % were employees with other jobs. No significant differences in baseline characteristics and outcome measures were observed between groups (all p-values > 0.05).
Intervention effects of the MIED programThe average of days completing MIED daily tasks was 31.31 days out of 49 days (SD = 16.46). Results of the 2×4 linear mixed effect models demonstrated that for mindfulness (F = 77.15, p < .001), DT (F = 33.59, p < .001), anxiety (F = 19.80, p < .001), and depression (F = 9.12, p < .001), the Time×Group interactions were significant. These indicated that the intervention had differential effects compared to the waitlist group. Post-hoc pairwise comparisons showed that mindfulness, anxiety, and depression improved in both groups (all p-values < 0.05; Cohen's d = 1.29/-1.39/-0.68 for the MIED group, -0.13/0.52/-0.25 for the Waitlist group), while DT only improved in the MIED group (p < .001; Cohen's d = 0.80) but not in the Waitlist group (p = 1.000, Cohen's d = -0.10). As for the between-group differences, the MIED group had significantly higher levels of mindfulness and DT, and lower levels of anxiety and depression at T1 (week 3), T2 (week5), and T3 (post-test) compared to the waitlist group (all p-values < 0.05). The post-test between-group effect sizes for anxiety (Cohen's d =-0.41, 95 %CI = [-0.71. -0.10]) and depression (Cohen's d =-0.35, 95 %CI = [-0.65, -0.05]) were small. Details of descriptive statistics are presented in Table S1, and results of post-hoc analyses are presented in Table S2 and S3 in the Supplementary Material.
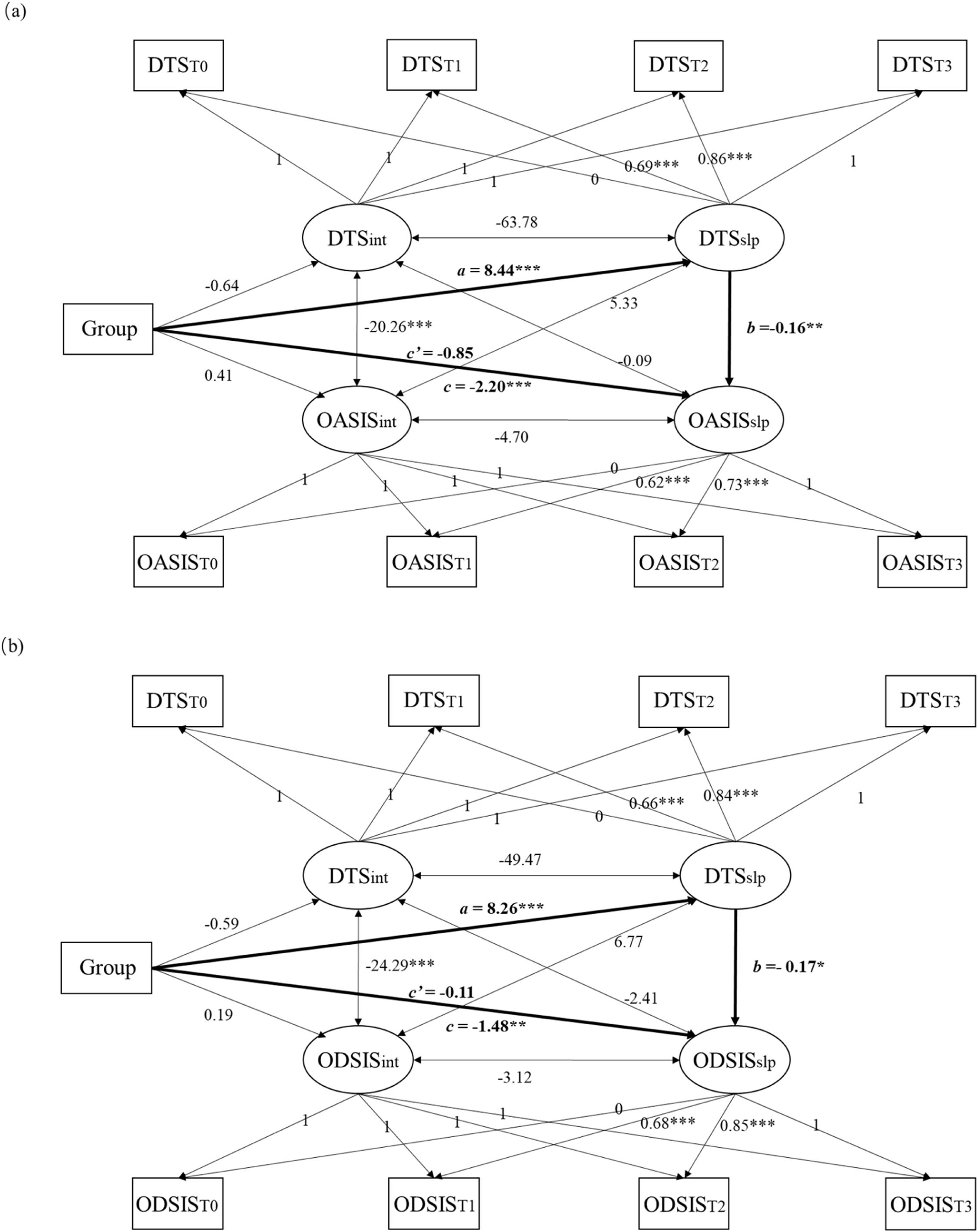
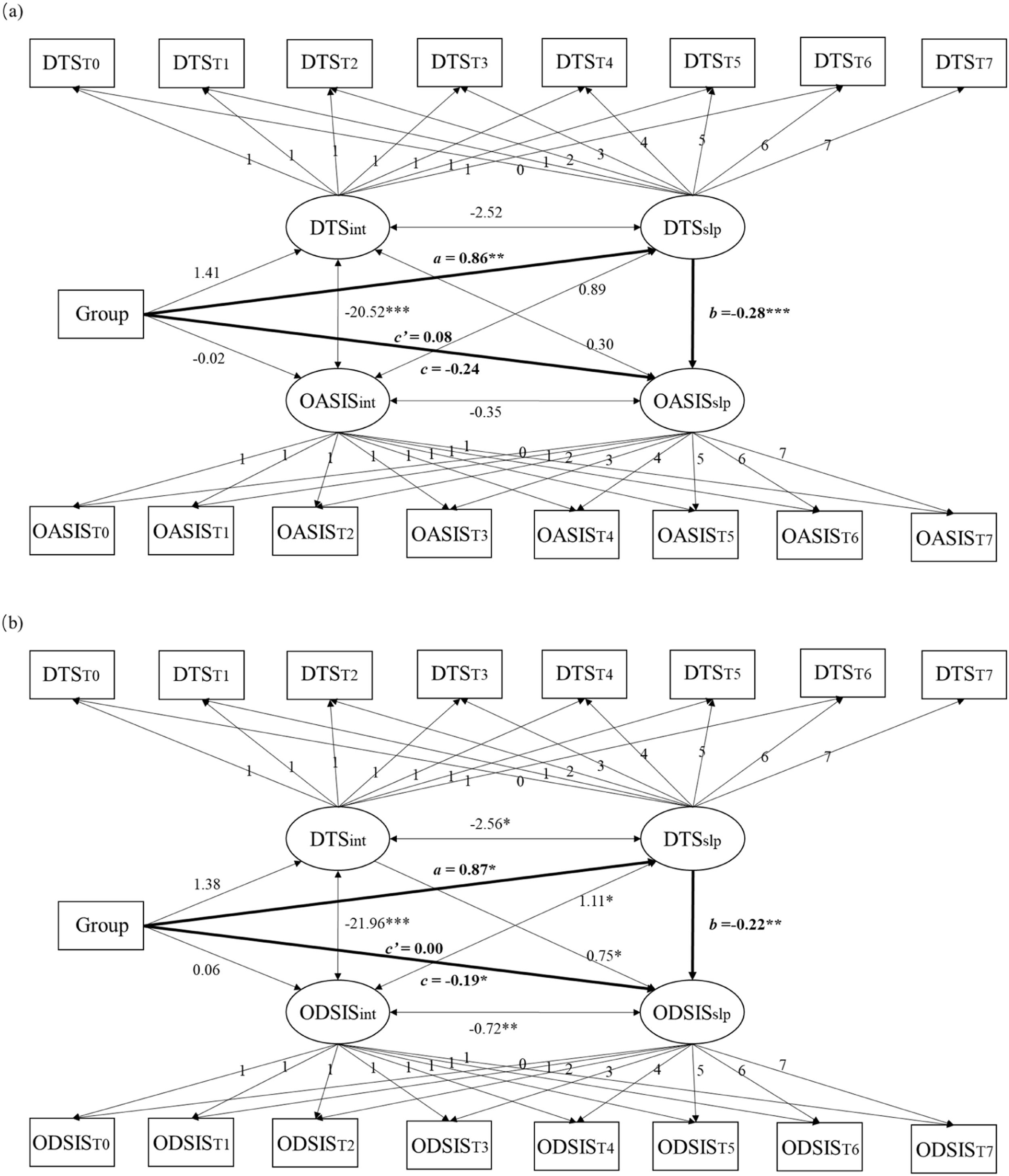
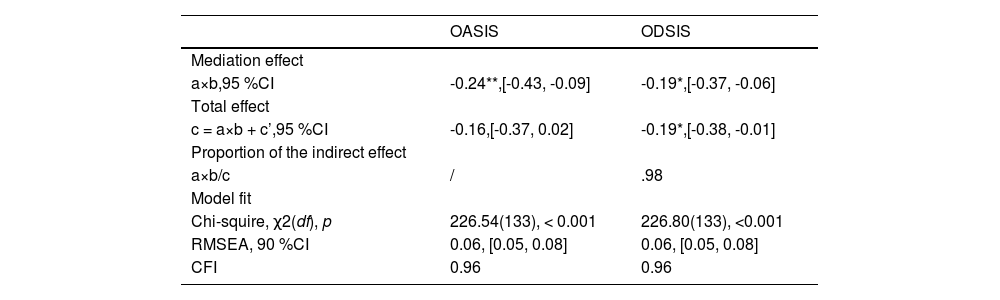
Effect of MIED on anxiety and depression via DTThe PP-LGCMs provided a good fit for the data (see Table 1). Results of the PP-LGCMs showed that increases in DT negatively predicted a decrease in anxiety and depression (See Table 1, Fig 2). In addition. the indirect effects of MIED on the slope of anxiety/depression via the slope of DT were significant, with an unstandardized estimate of -1.35/-1.37 (95 %CI did not contain zero). Both direct effects from the group to anxiety/depression were nonsignificant. Thus, the total effects of MIED on change in anxiety/depression were mostly explained by the impact of MIED in improving DT. The ratio of the indirect effect to the total effect from the group on anxiety/depression was 0.61/0.93.
Parallel process latent growth curve parameter estimates of Study 1.
Note. OASIS = Overall Anxiety Severity and Impairment Scale (anxiety); ODSIS = Overall Depression Severity and Impairment Scale (depression); CFI = Comparative Fit Index; CI = confidence interval; RMSEA = Root Mean-square error of approximation. * p < .05; ** p < .01; *** p < .001.
Parallel process latent growth curve model of Study 1. DTS = Distress Tolerance Scale (distress tolerance); OASIS = Overall Anxiety Severity and Impairment Scale (anxiety); ODSIS = Overall Depression Severity and Impairment Scale (depression). int = intercept; slp = slope. Group (0 = Waitlist, 1 = MIED). * p < .05; ** p < .01; *** p < .001.
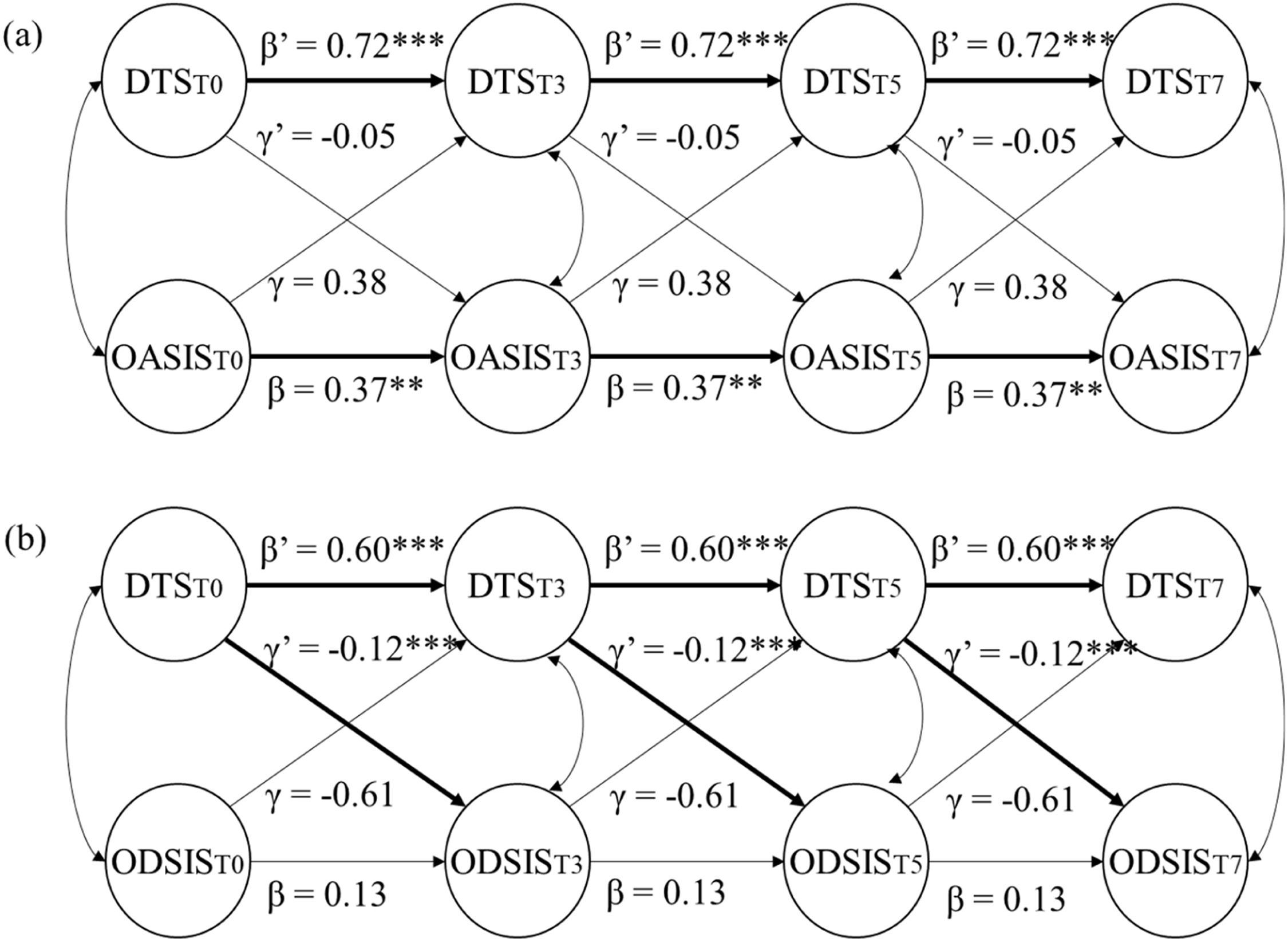
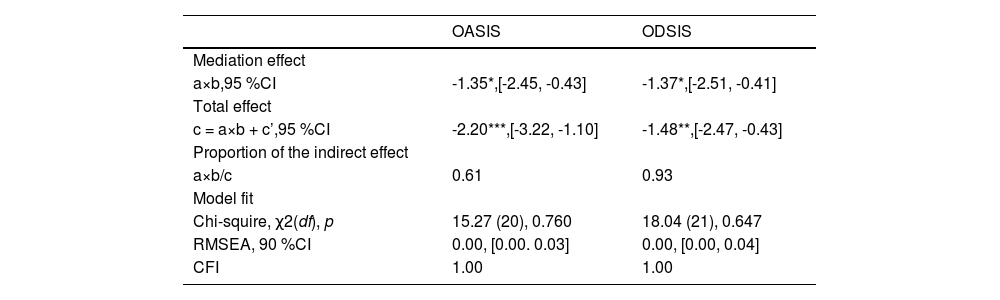
The models provided adequate model fit (for DT and anxiety: χ2(17) = 26.16, RMSEA = 0.06, 90 %CI = [0, 0.10], CFI = 0.98; for DT and depression: χ2(17) = 30.56, RMSEA = 0.07, 90 %CI = [0.03, 0.12], CFI = 0.97). Results of the RI-CLPMs indicated that DT could not significantly predict subsequent anxiety at distress tolerance one-lag (i.e., 2 to 3 weeks; γ’ = -0.05, p = .195), and vice versa (γ = 0.38, p = .254; See Fig. 3a). However, DT was a statistically significant predictor of depression at one lag (γ’ = -0.12, p < .001), whereas depression was not a statistically significant predictor of subsequent DT (γ = -0.61, p = .060; See Fig 3b). Therefore, during the intervention, DT was found to be temporally preceding depression, but not anxiety.
Bivariate Cross-lagged panel models of measures of distress tolerance, anxiety, and depression of Study 1. DTS = Distress Tolerance Scale (distress tolerance); OASIS = Overall Anxiety Severity and Impairment Scale (anxiety); ODSIS = Overall Depression Severity and Impairment Scale (depression). Correlated random intercepts were included in the models but are not shown. Unstandardized parameter estimates are shown within the model. ** p < .01, *** p < .001.
Study 1 aimed to investigate whether DT was a mechanism underlying the MIED, a recently developed MBI targeting transdiagnostic factors associated with anxiety and depression (Li et al., 2023a; Liu, 2024). Before examining the mediation models, examined the effects of the MIED program. The results showed that individuals who received the MIED intervention demonstrated higher levels of mindfulness, DT, and lower levels of anxiety and depression compared to those who only completed the assessments. These intervention effects of MIED were consistent with previous studies (e.g., He et al., 2023; Li et al., 2023a). Thus, DT as mechanism met the experimental manipulation criterion, which is consistent with Hypothesis 1.
In terms of the mechanism underlying MIED, the results support the idea that improvements in DT mediate the beneficial effects of the MIED program on anxiety and depression. This finding aligns with previous research that has shown DT mediating the relationship between mindfulness and depression/anxiety (Li et al., 2023b). Therefore, it is indicated that DT as a mechanism underlying the MIED for depression and anxiety also met the strong association criterion (Hypothesis 2). Regarding the temporal relationship between changes in DT, anxiety, and depression, the results from the RI-CLPMs indicated that changes in DT preceded depression but not anxiety. Therefore, the temporal precedence criterion was only met when the outcome was depression (Hypothesis 3).
Although provided some evidence for the mechanistic role of DT, Study 1 did not distinguish between clinical and nonclinical participants, making it harder to generalize the results to clinical samples. In addition, the insignificant path from DT to anxiety at t+1 may due to the fact that the time lag of two to three weeks was not sufficient to fully capture the temporal precedence of DT and anxiety. To address these issues and further validate the findings, Study 2 was conducted to replicate Study 1′s findings in a clinical sample. Weekly measurements would be taken during the intervention to examine whether DT fulfilled the temporal precedence criterion as a mediating factor (Kazdin, 2007).
Study 2MethodsParticipantsParticipants who received a diagnosis of an emotional disorder were recruited via social networks. The inclusion criteria were: (1) aged between 18 and 65 years old; (2) K10 score higher than 21 points; (3) providing diagnosis with emotional disorders, including anxiety disorders (such as panic disorder, social anxiety disorder, and generalized anxiety disorder) and unipolar depression, or assessed to have emotional disorders using the Mini-International Neuropsychiatric Interview (MINI; Sheehan et al., 1998; Si et al., 2009); (4) if taking medication, the medication dosage has remained stable for at least four weeks before intervention and was expected to remain stable during the intervention; and (5) voluntarily joined the study and signed an informed consent form. The exclusion criteria were the same as in Study 1. The sample size calculation was identical to Study 1; a minimum of 150 participants was required (Cheong, 2011; Sunnhed et al., 2022).
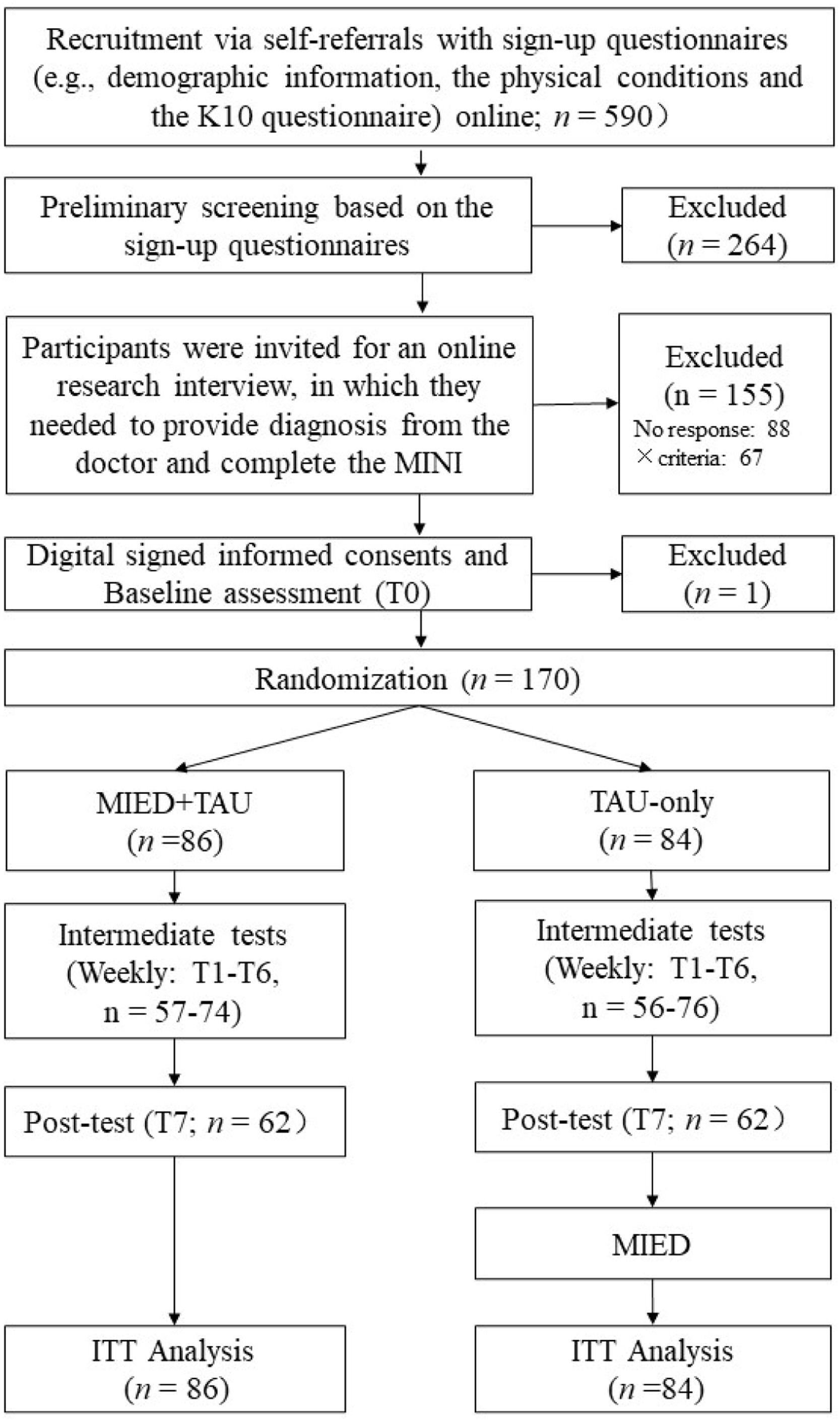
Data were collected in two waves. In total, 590 participants completed the sign-up questionnaires, of whom 264 were excluded for not meeting the inclusion criteria or meeting the exclusion criteria in preliminary screening, 155 were excluded based on results from interviews, and 1 did not finish baseline measures, leaving 170 participants included in randomization (See Fig. 4).
ProceduresThe current study was a prospective, pre-registered, repeated-measure RCT. It was pre-registered in Chinese Clinical Trial Registry (http://www.chictr.org.cn/, Registration number: ChiCTR2200059140). Data were collected in two waves: Wave 1 between May and July 2022 and Wave 2 between June and August 2023. Participants were recruited through social media, where they completed the sign-up questionnaire and informed consent form. Subsequently, they underwent preliminary screening based on the inclusion and exclusion criteria mentioned earlier. Participants who passed the initial screening were then invited to participate in an interview. These interviews were conducted by master's and doctoral students majoring in clinical psychology, all of whom had received training in clinical interviewing. The interview procedure involved participants presenting documentation of their existing diagnosis to the interviewer, completing the MINI, and ensuring that participants were informed about the study arrangements to guarantee their understanding. Patients who passed the interview screening received a baseline measurement questionnaire (T0).
After completing the questionnaire, patients were randomly assigned to the MIED+TAU (treatment as usual) group or the TAU-only group. A randomization list was created using a computer-generated random number sequence in Excel. The randomization was stratified by gender, age, and diagnosis to ensure a balance of participants across the groups.
After the randomization, patients in the MIED+TAU group continued with their usual psychological or medication treatment and received the MIED program. During this period, the TAU-only group received no intervention other than their usual treatment. Both groups completed measurements weekly during the intervention period (T1-T6) and after the intervention (T7). After the post-test, the TAU-only group received the MIED program (as shown in Fig. 4). Participants did not receive any form of compensation or remuneration. The intervention used in the current study was the MIED program described in Study 1.
MeasurementsMindfulness As in Study 1, we used the Five Facet Mindfulness Questionnaire-Short form (FFMQ-SF; Hou et al., 2014) to measure mindfulness. In this study, the FFMQ-SF in the pretest had a Cronbach's alpha of 0.81.
Distress tolerance The DTS (You and Leung, 2011) described in Study 1 was used to measure distress tolerance. In this study, the DTS in the pretest had a Cronbach's alpha of 0.91.
Anxiety The OASIS described in Study 1 (Liu et al., 2023) was used to measure anxiety. In this study, the OASIS in the pretest had a Cronbach's alpha of 0.90.
Depression The ODSIS described in Study 1 (Liu et al., 2023) was used to measure anxiety. In this study, the ODSIS in the pretest had a Cronbach's alpha of 0.94.
Statistical analysesAll data were analyzed using ITT analyses. Similar to Study 1, we used 2×8 LMMs to examine the intervention effects of the MIED program. We also used PP-LGCMs to examine the mediating effect of DT. Finally, we used RI-CLPM to examine the temporal precedence of DT, anxiety, and depression during the intervention.
ResultsParticipant flow and characteristicsA total of 170 participants from the MIED+TAU (n = 86) and the TAU-only group (n = 84) were included in the study (see Fig 4 for a detailed description of the participant flow). The final sample was primarily comprised of females (N = 127; 74.70 %), with a mean age of 31.65 years (SD = 9.64) and an average of 16.73 years of education (SD = 2.57). Among them, 31.76 % were full-time students; 10.00 % were teachers; 7.59 % were technical/research staff; 5.88 % were professionals (such as lawyers, and medical workers); and 44.77 % were employed in other occupations. As for participants’ diagnoses, 29.41 % were diagnosed with depression, 24.12 % with anxiety disorders, 38.24 % with comorbid anxiety and depression, and 8.23 % with other emotion-related disorders. With regard to treatment, 72.94 % were receiving medication, and 27.06 % were receiving psychotherapy.
Intervention effects of the MIED programThe average of days completing the MIED daily tasks was 32.38 days out of 49 days (SD = 16.88). Results of the linear mixed effect models demonstrated that for mindfulness (F = 10.65, p < .001), DT (F = 8.05, p < .001), anxiety (F = 2.62, p = .011), and depression (F = 2.53, p = .014), the Time×Group interactions were significant. Post-hoc pairwise comparisons showed that mindfulness, anxiety and depression improved in both groups (all p-values <0.05; Cohen's d = 0.97/-1.03/-0.84 for the MIED+TAU group, 0.33/-0.60/-0.46 for the Waitlist group), while DT only improved in the MIED+TAU group (all p-values < 0.001; Cohen's d = 0.91) but not in the TAU-only group (all p-values > 0.05, Cohen's d = 0.15). As for the between-group differences, the MIED+TAU group had significantly higher levels of mindfulness since T2 (Week2), and higher levels of DT since T1 (Week 1) compared to the TAU-only group (all p-values < 0.05); the MIED+TAU group had lower levels of anxiety and depression only at post-test compared to the TAU-only group (all p-values < 0.05). The post-test between-group effect sizes for anxiety (Cohen's d = -0.42) and depression (Cohen's d = -0.38) were small. Details of the descriptive statistics are presented in Table S4, and results of post-hoc analyses are presented in Table S5 and S6 in the Supplementary Material.
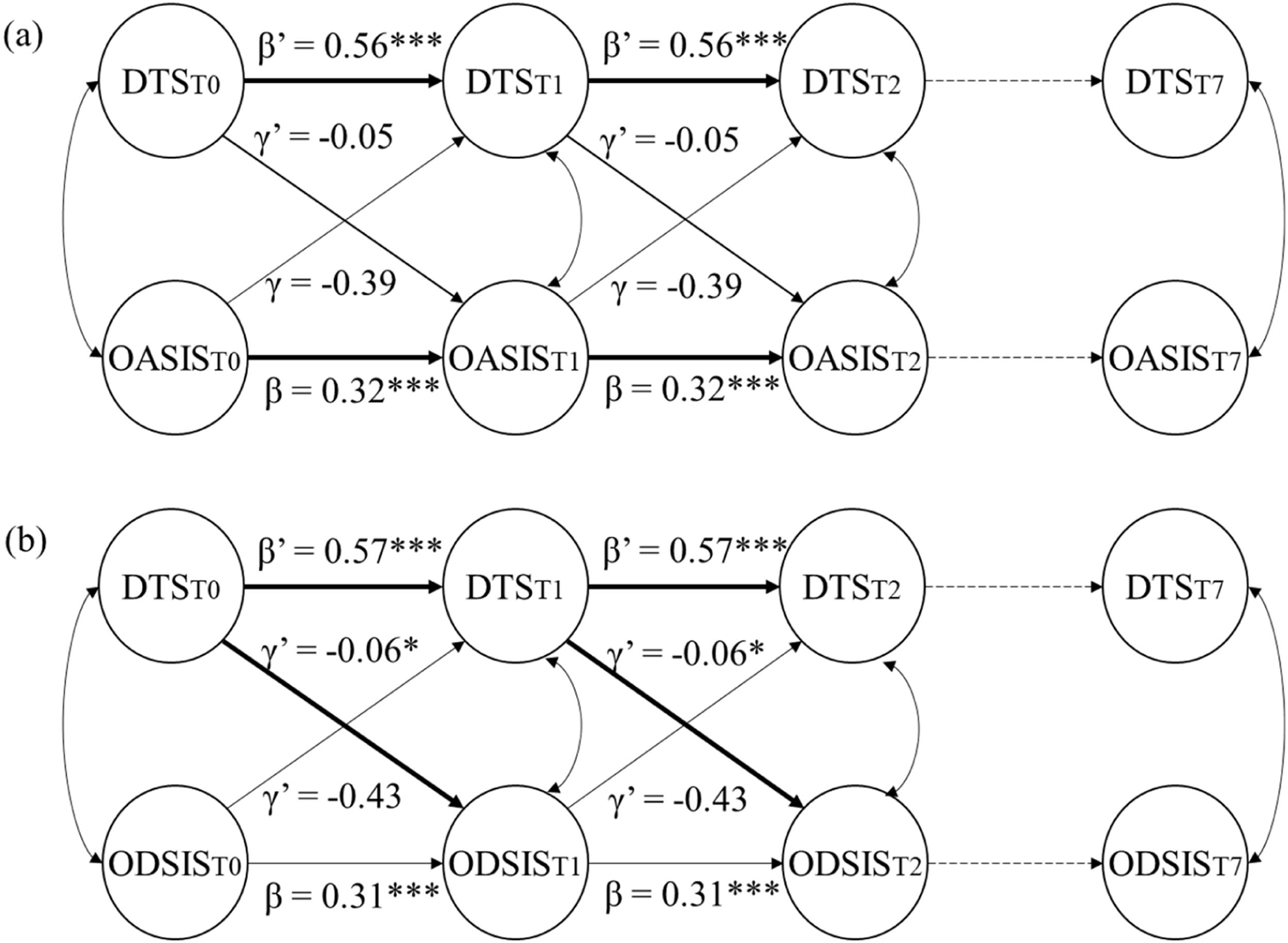
Effects of MIED on anxiety and depression via DTThe PP-LGCMs provided an adequate fit for the data (see Table 2). Results of the PP-LGCMs showed that increases in DT negatively predicted a decrease in anxiety and depression (See Table 2, Fig 5). In addition, the indirect effects of MIED on the slope of anxiety/depression via the slope of DT were significant (see Table 2). Both direct effects from the group to anxiety/depression were nonsignificant. Thus, the total effects of the intervention on change in anxiety/depression were mostly explained by the impact on change in DT. The ratio of the indirect effect to the total effect from group to depression was 0.98. However, for anxiety, the total effect was nonsignificant. Therefore, only indirect effect existed.
Parallel process latent growth curve parameter estimates of Study 2.
Note. OASIS = Overall Anxiety Severity and Impairment Scale (anxiety); ODSIS = Overall Depression Severity and Impairment Scale (depression). CFI = Comparative Fit Index; CI = confidence interval; RMSEA = Root Mean-square error of approximation. * p < .05, ** p < .01.
Parallel process latent growth curve model with distress tolerance and anxiety/depression of Study 2. DT = Distress Tolerance Scale (distress tolerance); OASIS = Overall Anxiety Severity and Impairment Scale (anxiety). int = intercept; slp = slope. Group (0 = TAU-only, 1 = MIED+TAU). * p < .05; ** p < .01; *** p < .001.
The models provided adequate model fit (for DT and anxiety: χ2(106) = 140.03, RMSEA = 0.06, 90 %CI = [0.03, 0.09], CFI = 0.96; for DT and depression: χ2(106) = 150.74, RMSEA = 0.07, 90 %CI = [0.04, 0.09], CFI = 0.95). Results of the RI-CLPMs indicated that DT did not significantly predict subsequent anxiety at distress tolerance one-lag (i.e., 1 week; γ’ = -0.05, p = .061), and vice versa (γ = -0.39, p = .087; See Fig. 6a). DT was a significant predictor of depression at one lag (γ’ = -0.06, p = .011). However, the reverse relationship was not significant (γ = -0.43, p = .062; See Fig. 6b). Thus, during the intervention, DT temporally preceded depression, but not anxiety.
Bivariate Cross-lagged panel models of measures of distress tolerance, anxiety, and depression of Study 2. DTS = Distress Tolerance Scale (distress tolerance); OASIS = Overall Anxiety Severity and Impairment Scale (anxiety); ODSIS = Overall Depression Severity and Impairment Scale (depression). Only the first three time points are shown but models were estimated with all measures (as indicated by the dashed lines). Correlated random intercepts were included in the models but are not shown. Unstandardized parameter estimates are shown within the model. * p < .05, *** p < .001.
Study 2 found significant beneficial effects of the MIED program in improving mindfulness and DT, alleviating anxiety and depression in the clinical samples with emotional or related disorders. Both Study 1 and study 2 supported the effects of the MIED program, suggesting that mindfulness-based interventions could yield significant effects in improving anxiety and depression, as found in previous studies (e.g., Ju et al., 2022; Li et al., 2023a). Hypothesis 1 was again supported in a clinical sample with emotional disorders.
In addition, Study 2 found that DT significantly mediated the effects of a MBI (i.e., the MIED program) on anxiety and depression, based on results from PP-LGCMs. This suggests that through practicing mindfulness and engaging in other exercises within the MIED program, individuals may become less likely to appraise uncomfortable emotions as unacceptable and better equipped to tolerate distressing experiences (e.g., Lotan et al., 2013), thereby reducing emotional distress in the long run (Leyro et al., 2010; Li et al., 2023b). The mediation effect of DT was replicated in a clinical sample. Therefore, hypothesis 2 was again supported in a clinical sample.
Finally, although DT was measured weekly, Study 2 observed that changes in DT temporally preceded changes in depression, but not anxiety. Thus, in line with Study 1, hypothesis 3 was only supported for depression, but not anxiety.
General discussionPrevious studies consistently found positive effects of MBIs on anxiety and depression (e.g., Creswell, 2016; Li et al., 2023a; Segal et al., 2020). However, little is known about the mediators of these treatments. Previous studies have pointed to distress tolerance as one of the key mediators (e.g., Carpenter et al., 2019; Li et al., 2023b). The current study builds on this prior research by examining DT as a treatment mediator of MBI for anxiety and depression, using two RCT studies with multiple time-point measurements. The MIED program was used as the intervention (Liu, 2024). Both studies revealed that the MIED program was effective in improving mindfulness and DT, alleviating anxiety and depression for individuals with at least a moderate level of emotional distress (Study 1) and with emotional disorders (Study 2). Furthermore, changes in DT mediated the effects of the MIED program on changes in anxiety and depression. These results suggest that improvements in DT may have contributed to the reductions in anxiety and depression symptoms. These findings suggest that DT meets the experimental manipulation and strong association criteria of mediation (Kazdin, 2007). The results of both studies supported hypotheses 1 and 2.
The current study provided evidence supporting the role of DT as a treatment mediator for reducing symptoms of anxiety and depression during MBIs. This finding aligns with previous studies that have identified DT, a skill that can be enhanced through MBIs (Kraemer et al., 2020), as a crucial transdiagnostic factor in anxiety and depression (e.g., Lass & Winer, 2020; Michel et al., 2016). Moreover, the current study utilized a RCT design, further replicating previous findings from cross-sectional and daily diary studies that have shown DT to mediate the relationship between mindfulness and depression/anxiety (Li et al., 2023b).
Furthermore, the results from the RI-CLPMs in both studies supported the observation that changes in distress tolerance (DT) preceded treatment changes in depression, but not in the case of anxiety. The absence of significant reversed relationships, where depression predicted DT in both studies, suggests that the temporal sequence is specific to the relationship between DT and depression. Hence, Hypothesis 3 was supported when the outcome was depression, but not anxiety.
It's important to note that establishing temporal precedence is crucial in discerning whether the mediator is a cause or an effect of changes in symptomatology, a consideration often overlooked in clinical studies (Kazdin, 2007; Kendall et al., 2017). This study was the first to investigate the temporal relationship between DT and anxiety/depression, emphasizing the significant finding that DT preceded depression. While the change in DT mediated the effects of the MIED program for both anxiety and depression, the absence of evidence for DT preceding anxiety during the intervention suggests that the mechanistic role of DT may vary for different outcomes. However, the p-value for the path from DT to anxiety at a one-week lag was 0.061. It is possible that this could reach significance with a larger sample size. Other possibilities include the one-week time lag not being sufficient to capture the temporal relationship between DT and anxiety or the DT-anxiety relationship during the intervention not being linear, which could not be investigated in RI-CLPMs. Future research could explore these differences more comprehensively, perhaps by adopting a larger sample size and more intensive tracking during interventions, such as employing intensive longitudinal study designs (Bolger & Laurenceau, 2013).
The findings of the current study need to be evaluated in light of some limitations that need to be addressed in future research to provide a more comprehensive understanding of DT as a treatment mediator of MBIs. First, self-report measures used in this study may have introduced biases, so future research should incorporate behavioral tasks and neuroscience indicators to objectively assess DT as a mediator of treatment change. Second, the study did not test the gradient and specificity criteria proposed by Kazdin (2007), future studies could manipulate the intervention dose of DT and include other mediators to test these criteria. Third, in Study 1, the attrition rate of the intervention group was higher than that of the control group. This aligns with findings from a previous meta-analysis, which reported that MBIs resulted in slightly higher attrition rates compared to control conditions in sensitivity analyses (Lam et al., 2022). In Study 2, we addressed this issue by putting more effort into contacting participants to complete the questionnaires. Future studies should aim to replicate the current study using innovative strategies. For example, personalized feedback or small incentives could potentially enhance study engagement and retention. Lastly, it is worth noting that, despite the relatively large total sample size and the models exhibiting adequate fit to the data, the comparatively smaller size of each group could have influenced the model fit measures and the stability of parameter estimates in the two complex models (i.e., PP-LGCMs and RI-CLPMs). Future studies should consider augmenting the sample size for the purpose of replicating the current study.
Despite these limitations, the current study offers valuable insights into the role of DT in MBIs by employing RCTs combined with multiple time-point measurements. Understanding the mechanisms of MBIs is crucial for elucidating the intervention's effects on diverse outcomes and optimizing therapeutic change by enhancing the intervention mechanisms (Kazdin, 2007). The results demonstrate that DT is a significant mediator underlying the effects of MBIs, specifically the MIED program in the current study. Clinicians can use this information to tailor MBIs for improving DT in patients with depression and/or anxiety disorders, leading to more effective interventions. Additionally, understanding DT's role as a treatment mediator can help clinicians identify which patients are likely to benefit the most from mindfulness interventions and make appropriate treatment recommendations. For instance, individuals with low DT levels may derive greater benefits from MBIs that specifically target and improve their DT skills. Besides instructing individuals to learn to stay with uncomfortable thoughts and feelings that arise during mindfulness meditation, practices from UP (Barlow et al., 2010), such as interoceptive exposure and exposure in vivo (i.e., challenging tasks in the MIED program), can be embedded in MBIs to enhance intervention effects.
ConclusionsOverall, the findings from the two RCTs conducted in samples of participants with at least moderate emotional distress and emotional disorders suggest that distress tolerance is a potential mechanism underlying the effectiveness of MBI, specifically the MIED program. Improvements in distress tolerance may contribute to reductions in depression. Additionally, the temporal precedence criterion was met for distress tolerance as a mechanism between the MIED program and depression, providing further evidence for the causal role of distress tolerance in reducing depression.
Ethical compliance statementCompliance with Ethical Standards: All procedures performed in the current study involving human participants were in accordance with the ethical standards of the School of Psychological and Cognitive Sciences of Peking University and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consentInformed consent was obtained from all participants included in the study.
Role of funding sourceThis work was supported by the National Natural Science Foundation of China (Project No. 31971016 and No. 32371138) and the National Clinical Research Center for Mental Disorders (Peking University Sixth Hospital; Project No. NCRC2021M01). The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Data availabilityThe current study (particularly Study 2) utilized clinical samples, and the data are not publicly available due to confidentiality concerns. Interested parties may contact the corresponding author to request access to the data.
CRediT authorship contribution statementYanjuan Li: Conceptualization, Methodology, Data curation, Formal analysis, Writing – original draft, Writing – review & editing. Mengyao He: Data curation, Validation. Zhenzhen Wang: Data curation. Stefan G. Hofmann: Writing – review & editing. Xinghua Liu: Conceptualization, Funding acquisition, Methodology, Writing – review & editing.
We thank all the participants who participated in this study. Special thanks to Kaerqika Shalihaer, Man Lu, You Chen, Yu Leng, Zitong Xin, and other master's students from Peking University for their invaluable assistance in collecting data and conducting clinical interviews for Study 2.