Background/Objetivo: According to the World Health Organization, one out of every four violent workplace acts takes place in the health setting. The aims of the study are to study the prevalence of workplace violence in primary healthcare (PHC) professionals by adapting the Healthcare-worker's Aggresive Behaviour Scale-Users (HABS-U), to establish the frequency of exposure to hostile indicators and to determine which professional group is most exposed. Method: Study through qualitative and quantitative methodology in PHC professionals of the Region of Murcia (Spain). In the qualitative phase in-depth interviews were conducted and during the quantitative phase the instrument was used to 574 professionals of 39 PHC centres. Results: The resulting scale shows excellent psychometric properties and correlates significantly with job satisfaction, burnout components, the factors of empathy and psychological well-being. There was a 90.2% prevalence of user violence, and non-medical personnel were found to be the professional group most exposed. Conclusion: The distribution of user violence is not homogeneous among the different professional groups of PHC. The adaptation of the scale may be useful for detection of user violence, as well as to evaluate the efficacy of intervention programs.
Antecedentes/Objetivo: Según la Organización Mundial de la Salud, en el ámbito sanitario se producen uno de cada cuatro incidentes laborales violentos. Los objetivos del estudio son examinar la prevalencia de violencia laboral en profesionales de Atención Primaria (AP) mediante la adaptación de la Healthcare-worker's Aggresive Behaviour Scale-Users (HABS-U), conocer la frecuencia de exposición a los indicadores hostiles y determinar el grupo profesional más expuesto. Método: Estudio realizado mediante metodología cualitativa y cuantitativa en profesionales de AP de la Región de Murcia (España). En la fase cualitativa se realizaron entrevistas en profundidad y en la fase cuantitativa se aplicó el instrumento a 574 profesionales de 39 centros de AP. Resultados: La escala resultante muestra excelentes propiedades psicométricas y sus medidas correlacionan de manera significativa con satisfacción laboral, los componentes del burnout, los factores de empatía y con el bienestar psicológico. La prevalencia de violencia de usuarios fue del 90,2% y el personal no sanitario resultó ser el grupo profesional más expuesto. Conclusión: La distribución de la violencia de usuarios no es homogénea entre los diferentes grupos profesionales de AP. La adaptación de la escala puede ser útil para la detección de la violencia de usuarios, así como para evaluar la eficacia de programas de intervención.
The International Labour Organization/International Council of Nurses/World Health Organization/Public Services International (ILO/ICN/WHO/PSI; 2002) defines workplace violence as “incidents in which workers suffers ill-treatment, threats or attacks in circumstances related to their work and which endanger, implicitly or explicitly, their safety, well-being or health” (p. 3). In this investigation, we focus on the study of low- and medium-intensity user violence aimed at Primary Healthcare (PHC) professionals because many studies consider that the authors of such aggressions towards healthcare workers are predominantly users, patients, or relatives (Alameddine, Mourad, & Dimassi, 2015; Alkorashy & Al Moalad, 2016; Park, Cho, & Hong, 2015; Spector, Zhou, & Che, 2014).
According to the forms of expression, workplace violence is classified as: (a) non-physical violence, referring to verbal abuse, threats, ironic language, disparaging looks, provocative or aggressive body language; and (b) physical violence, referring to physical intimidation and harm to people, properties or furniture (ILO, 2002ILO/ICN/WHO/PSI, 2002; Waschgler, Ruiz-Hernández, Llor-Esteban, & García-Izquierdo, 2013). The literature confirms the fact that non-physical violence predominates in the health sector, although we find that in certain services such as emergency wards and psychiatry, physical violence takes on relevant figures (Chapman, Styles, Perry, & Combs, 2010; Galián-Muñoz, Llor-Esteban, & Ruiz-Hernández, 2012; Llor-Esteban, García-Jiménez, Ruiz-Hernández, & Godoy-Fernández, 2016; Magnavita & Heponiemi, 2012). Among the PHC professionals, this phenomenon has received less attention, but some research confirms that whereas all the expressions of violence are present, non-physical or psychological types predominate, with a yearly prevalence range of 43.5–92.1% versus 7.9–18.3% for physical violence (El-Gilany, El-Wehady, & Amr, 2010; Fisekovic, Trajkovic, Bjegovic-Mikanovic, & Terzic-Supic, 2015; Gascón et al., 2013; Moreno-Jiménez et al., 2005).
Chappell and Di Martino's (2006) model of workplace violence, in its application to the health sector, notes the existence of diverse risk variables. In this sense, based on the existing literature, the risk factors of violence can be classified as follows: (a) patients: male, age, physical alterations and pathologies, mental state, psychopathology, patients’ perspective and attributions; or individual factors of health professionals, such as burnout or attitudes; (b) environmental factors or organizational factors: type of ward, such as emergency, psychiatry and intensive care units, long-term care, or geriatric centres; inadequate number of staff, assistential pressure, lack of privacy, climate of tension; (c) treatment-related factors, such as change of medication and restraint; and (d) interactional factors and societal factors (Ahmad, Al-Rimawi, Masadeh, & Atoum, 2015; Chapman et al., 2010; El-Gilany et al., 2010; Speroni, Fitch, Dawson, Dugan, & Atherton, 2014; Waschgler, Ruiz-Hernández, Llor-Esteban, & García-Izquierdo, 2013). In addition, the existence of diverse variables that modulate the impact of exposure to violence in the health sector has been proposed. Among the main variables identified are training in communication skills (Farrell, Shafiei, & Chan, 2014) and empathy (Bernaldo-de-Quirós, Labrador, Piccini, Gómez, & Cerdeira, 2014).
User violence perceived by PHC professionals negatively impacts on their health. Accordingly, exposure to workplace violence is associated with higher levels of burnout (Alameddine et al., 2015; Bernaldo-De-Quirós, Piccini, Gómez, & Cerdeira, 2015; Galián-Muñoz, Llor-Esteban, & Ruiz-Hernández, 2014; Gascón et al., 2013; Roldán, Salazar, Garrido, & Ramos, 2013), a decrease in psychological well-being, anxiety, depression (Bernaldo-De-Quirós et al., 2015; Da Silva et al., 2015; Magin, Joyce, Adams, Goode, & Cotter, 2009; Roldán et al., 2013) and job dissatisfaction (Aiken et al., 2001; Heponiemi, Kouvonen, Virtanen, Vänskä, & Elovainio, 2014).
On the basis of the hypothesis that the characteristics of the user-PHC professional relationship differs from that of the hospital sphere and considering that, after the review performed, no instrument was found that specifically assesses the phenomenon of user violence towards PHC professionals, the goals of this study are: to study the prevalence of workplace violence in PHC professionals through the adaptation of the “Healthcare-workers¿Aggresive Behaviour Scale-Users (HABS-U)” (Waschgler, Ruiz-Hernández, Llor-Esteban, Jiménez-Barbero, 2013), to establish the frequency of exposure to hostile indicators and to determine which professional group is the most exposed.
MethodAn instrumental investigation was performed with qualitative methodology to adapt the HABS-U to PHC professionals. An empirical study with quantitative, descriptive, and cross-sectional methodology was also performed (Montero & León, 2007) through the application of various instruments assessing occupational health.
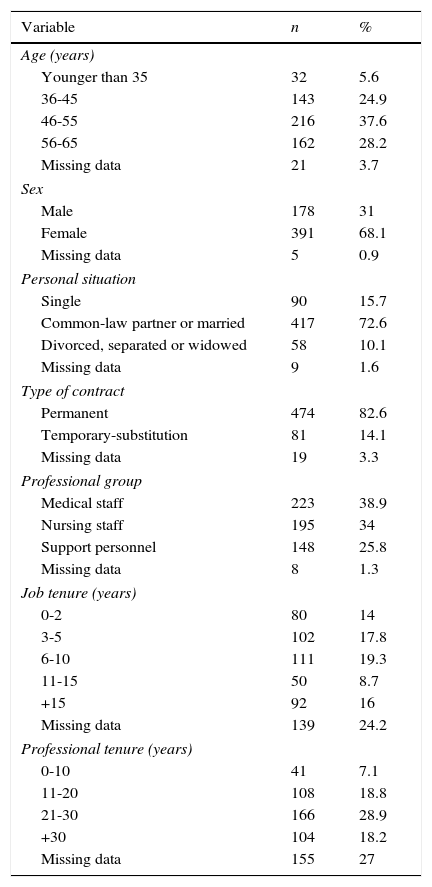
ParticipantsThe study population consisted of PHC professionals in different health areas depending on the Health Service of Murcia (Spain). Following the internal organisation of the PHC centres, the professionals were divided into three groups: medical staff, nursing staff and non-healthcare staff. A total of 13 in-depth interviews were conducted: 5 with medical staff, 5 with nurses and 3 with non-healthcare personnel. The sample's mean age was 48.8 years (SD=9.1), ranging between 32 and 60 years. The female gender predominated (61.5%) with mean job tenure of 11.3 years (SD=8.8). Subsequently, we applied the assessment instruments to a sample of 574 professionals in 39 PHC centres. Most of the professionals were women (68.1%), married or living with a partner (72.6%) and with a mean age of 49.6 years (SD=8.4). Table 1.
Socio-demographic and job characteristics of the sample.
| Variable | n | % |
|---|---|---|
| Age (years) | ||
| Younger than 35 | 32 | 5.6 |
| 36-45 | 143 | 24.9 |
| 46-55 | 216 | 37.6 |
| 56-65 | 162 | 28.2 |
| Missing data | 21 | 3.7 |
| Sex | ||
| Male | 178 | 31 |
| Female | 391 | 68.1 |
| Missing data | 5 | 0.9 |
| Personal situation | ||
| Single | 90 | 15.7 |
| Common-law partner or married | 417 | 72.6 |
| Divorced, separated or widowed | 58 | 10.1 |
| Missing data | 9 | 1.6 |
| Type of contract | ||
| Permanent | 474 | 82.6 |
| Temporary-substitution | 81 | 14.1 |
| Missing data | 19 | 3.3 |
| Professional group | ||
| Medical staff | 223 | 38.9 |
| Nursing staff | 195 | 34 |
| Support personnel | 148 | 25.8 |
| Missing data | 8 | 1.3 |
| Job tenure (years) | ||
| 0-2 | 80 | 14 |
| 3-5 | 102 | 17.8 |
| 6-10 | 111 | 19.3 |
| 11-15 | 50 | 8.7 |
| +15 | 92 | 16 |
| Missing data | 139 | 24.2 |
| Professional tenure (years) | ||
| 0-10 | 41 | 7.1 |
| 11-20 | 108 | 18.8 |
| 21-30 | 166 | 28.9 |
| +30 | 104 | 18.2 |
| Missing data | 155 | 27 |
The Healthcare-worker's Aggresive Behaviour Scale-Users (HABS-U). This is an adapted instrument that assesses user violence of low and medium intensity towards professionals in the specialized care area. The authors developed an initial pool of 166 items based on the information obtained from three discussion groups with 21 participants and 6 in-depth interviews with nursing professionals. The pool of items was applied to a sample of 1484 nursing professionals from 11 public hospitals. A sample of n=790 was employed for item construction and of n=694 for item validation. The resulting instrument has 10 Likert-type items ranging from 1 (never) to 6 (daily) during the past year, distributed in two factors: Non-physical violence (α=.85, explaining 36.4% of the variance) and Physical violence (α=.74, explaining 20.9% of the variance) (Waschgler, Ruiz-Hernández, Llor-Esteban, & García-Izquierdo, 2013).
To verify the criterion validity of the study, four validated occupational health scales were utilized:
- -
Overall Job Satisfaction (OJS) (Warr, Cook & Wall, 1979), adapted to Spanish by Pérez and Hidalgo (1995). This scale assesses job satisfaction and is made up of 15 items divided into two subscales: Intrinsic satisfaction, which addresses issues such as recognition for work, responsibility, promotion, etc. (α=.85); and Extrinsic satisfaction which explores aspects of the organization of work, such as work schedule, pay, physical conditions, etc. (α=.72). They are rated on a Likert-type response format, ranging from 0 (very dissatisfied) to 6 (very satisfied) (Berrios-Martos, Augusto-Landa & Aguilar-Luzón, 2006).
- -
The Jefferson Scale of Physician Empathy (JSPE) (Hojat et al., 2002). We used the adaptation of Alcorta-Garza, González-Guerrero, Tavitas-Herrera, Rodríguez-Lara and Hojat (2005). This scale assesses empathy and contains 20 items divided into three factors: Perspective taking (α=.90), Compassionate care (α=.72) and the Ability to put oneself in the patient's place (α=.66). The Likert-type items are rated from 1 (totally disagree) to 7 (totally agree).
- -
The Maslach Burnout Inventory-GS (MSI-GS) of Schaufeli, Leiter, Maslach and Jackson (1996), in the Spanish version of Salanova, Schaufeli, Llorens, Peiró and Grau (2000). It assesses levels of burnout through 16 items distributed in three dimensions: Emotional exhaustion which refers to the loss of the emotional resources because of the work (α=.90); Depersonalization, reflecting indifference and distant attitudes toward work (α=.81); and Professional efficiency, perceived effectiveness in one's work (α=.73). Respondents rate each Likert-type item from 0 (never) to 6 (every day) (García-Izquierdo, Llor-Esteban, García-Izquierdo, & Ruiz-Hernández, 2006).
- -
The General Health Questionnaire (GHQ-28; Goldberg & Hillier, 1979), in its 28-item version according to the Spanish adaptation of Lobo, Pérez-Echeverría and Artal (1986). It is divided into 4 subscales: Psychosomatic symptoms (feelings of tiredness, weakness and bodily discomfort), Anxiety/Insomnia, Social dysfunction (problems performing daily activities) and Depressive symptomatology (thoughts and feelings of personal worthlessness, sadness, hopelessness and suicide). This instrument obtained values of Cronbach's alpha for the subscales ranging from .80 to .91 (García-Izquierdo et al., 2006).
Qualitative phase: in-depth interviews were conducted to obtain new data and complement the indicators of the HABS-U. Based on the specialized bibliography, a guideline adapted to each of the three occupational groups was developed. We contacted with key informants, and the interviews were recorded for later transcription and qualitative analysis. They were continued until reaching the point of information saturation. With the information obtained, 15 new items, which were reviewed and validated by a group of experts (university professors, doctorate students and practising health professionals) were drafted by consensus and following previously established explicit criteria (Haladyna, Downing, & Rodríguez, 2002). After their revision, 7 items were removed because they presented drafting problems or content overlap.
Quantitative phase: Considering the total number of workers (2,575 professionals in 74 PHC centres), a confidence level of 95% and an assumed error of ±3%, a sample size of 510 professionals were estimated. Two-stage cluster sampling was used to select the sample. Firstly, the population was stratified by PHC centres (clusters) and 39 centres were selected through simple random sampling. Subsequently, using a fixed ratio pattern, we selected from the alphabetical listing of all the professionals from each centre those who were numbered with multiples of three, who were then invited to participate in the study. Meetings were held with the coordinators of the selected centres in which they were informed of the study, and the research protocol was distributed in printed form. 670 protocols were distributed, considering a 30% rate of non-response. Programmed visits to the centre were performed to clarify possible doubts and to collect the completed protocols. Participation was voluntary, ensuring strict confidentiality and anonymity of the data collected.
This study was approved by the Commission on Ethics of Research of the University of Murcia and by the managers of the health areas included. The authors declare no conflict of interest.
Data analysisTheme analysis methodology was used for the qualitative analysis of the interviews (Clarke & Braun, 2013). Following its phases, we identified the behaviour categories from the transcript of the interviews. We performed a theoretical triangulation, comparing the categories found with the results provided by investigations of this subject. Following the methodology described in similar studies (Waschgler, Ruiz-Hernández, Llor-Esteba, & García-Izquierdo, 2013; Waschgler, Ruiz-Hernández, Llor-Esteban, & Jimenez-Barbero, 2013), we conducted exploratory factor analysis (using SPSS® version 22) with maximum likelihood and varimax rotation and combining criteria were combined: (a) each factor should explain at least 5% of the total variance; (b) the factor loading of the items should be at least .50; (c) an item could not load on two factors with more than .40; and (d) the ítems contained in each factor should have adequate internal consistency (Nunnally & Berstein, 1994). We examined the distribution of the scale through the means, standard deviations, and skewness and kurtosis indexes. To verify the results obtained, we performed confirmatory factor analysis using the maximum likelihood estimation with the EQS program, version 6.1. Internal consistency and reliability of each factor were also analysed, and the performance of the adapted scale was confirmed with other external correlates, using the Pearson correlation coefficient. In addition, a descriptive analysis of the sample was conducted; we recorded the number and percentage of workers who reported each of the violence indicators that make up the scale, as a function of exposure frequency; ANOVA was carried out using the Brown-Forsythe robust test, after confirming that the assumption of homogeneity of variance was not met, with the Games-Howell post hoc test to establish the differences between the different professional groups.
ResultsQualitative phase: 8 new specific items about the characteristics of PHC work were created (e.g., ‘users hit the counter or the office door’, ‘users threaten me if their expectations are not met’, ‘users interrupt my work rudely’). Thus, the 10 items of the original scale were validated semantically (Waschgler, Ruiz-Hernández, Llor-Esteban, & García-Izquierdo, 2013). The scale adapted to PHC (Healthcare-worker's Aggresive Behaviour Scale-Users- Version Primary Healthcare [HABS-U-PHC]) consisted of 10 items of the HABS-U plus 8 new items relating to aggressive behaviours or challenging attitudes.
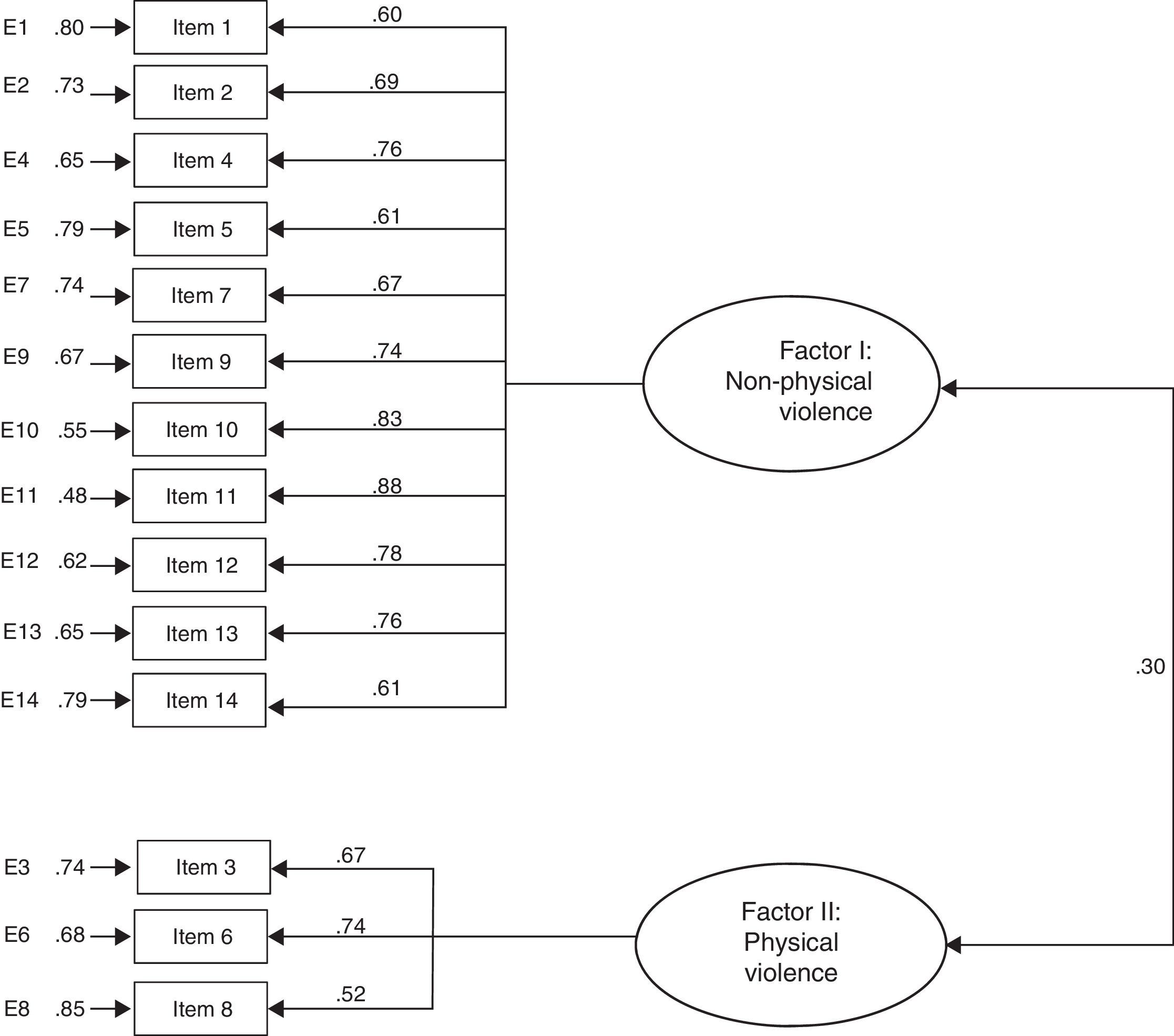
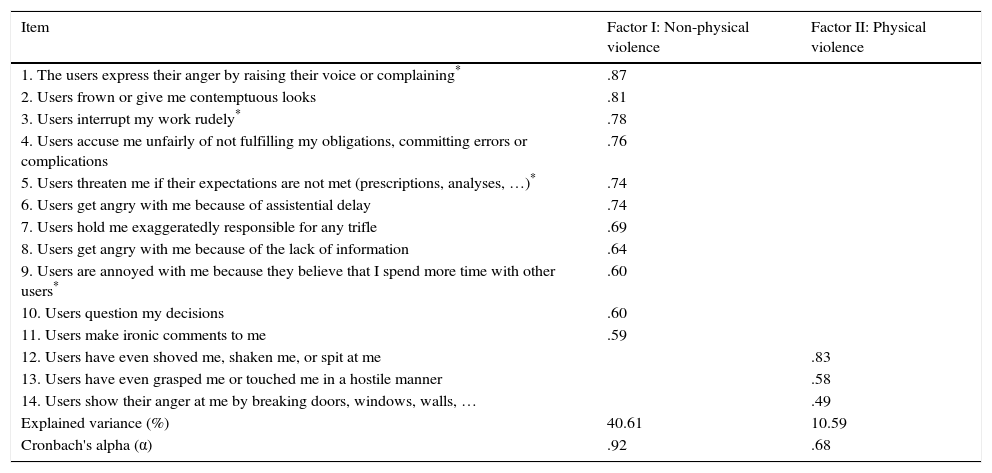
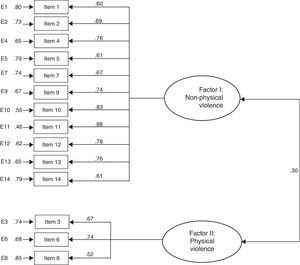
Quantitative phase: We performed exploratory factor analysis of the data, using the maximum likelihood method with Varimax rotation (KMO=.92; Bartlett sphericity test χ=3920.59, p<.001). Exploratory factor analysis (Table 2) yielded a scale consisting of 14 items (4 were eliminated for failing to meet the adove-mentioned criteria), explaining 58.1% of the variance (α= .91). Its items were grouped into two factors: Factor I (Non-physical violence) with 11 items about user violent verbal and nonverbal behaviours, explaining 40.6% of the variance (α=.92); and Factor II (Physical violence), consisting of 3 items that account for 10.6% of the variance (α= .68). Table 3 shows the results obtained after examining the distribution of the scale.The structure factor obtained was studied by means of confirmatory factor analysis (Figure 1) with appropriate goodness-of-fit indices (Bentler, 1990): Satorra-Bentler χ2=207.47 (df=76); p<.001; AGFI=.90, CFI=.91, NFI=.90 and TLI=.91, SRMR=.05 and, lastly, RMSEA=.05 (95% CI [.04 - .06]).
Matrix of rotated components, explained variance and Cronbach alpha (internal consistency).
| Item | Factor I: Non-physical violence | Factor II: Physical violence |
|---|---|---|
| 1. The users express their anger by raising their voice or complaining* | .87 | |
| 2. Users frown or give me contemptuous looks | .81 | |
| 3. Users interrupt my work rudely* | .78 | |
| 4. Users accuse me unfairly of not fulfilling my obligations, committing errors or complications | .76 | |
| 5. Users threaten me if their expectations are not met (prescriptions, analyses, …)* | .74 | |
| 6. Users get angry with me because of assistential delay | .74 | |
| 7. Users hold me exaggeratedly responsible for any trifle | .69 | |
| 8. Users get angry with me because of the lack of information | .64 | |
| 9. Users are annoyed with me because they believe that I spend more time with other users* | .60 | |
| 10. Users question my decisions | .60 | |
| 11. Users make ironic comments to me | .59 | |
| 12. Users have even shoved me, shaken me, or spit at me | .83 | |
| 13. Users have even grasped me or touched me in a hostile manner | .58 | |
| 14. Users show their anger at me by breaking doors, windows, walls, … | .49 | |
| Explained variance (%) | 40.61 | 10.59 |
| Cronbach's alpha (α) | .92 | .68 |
Note.
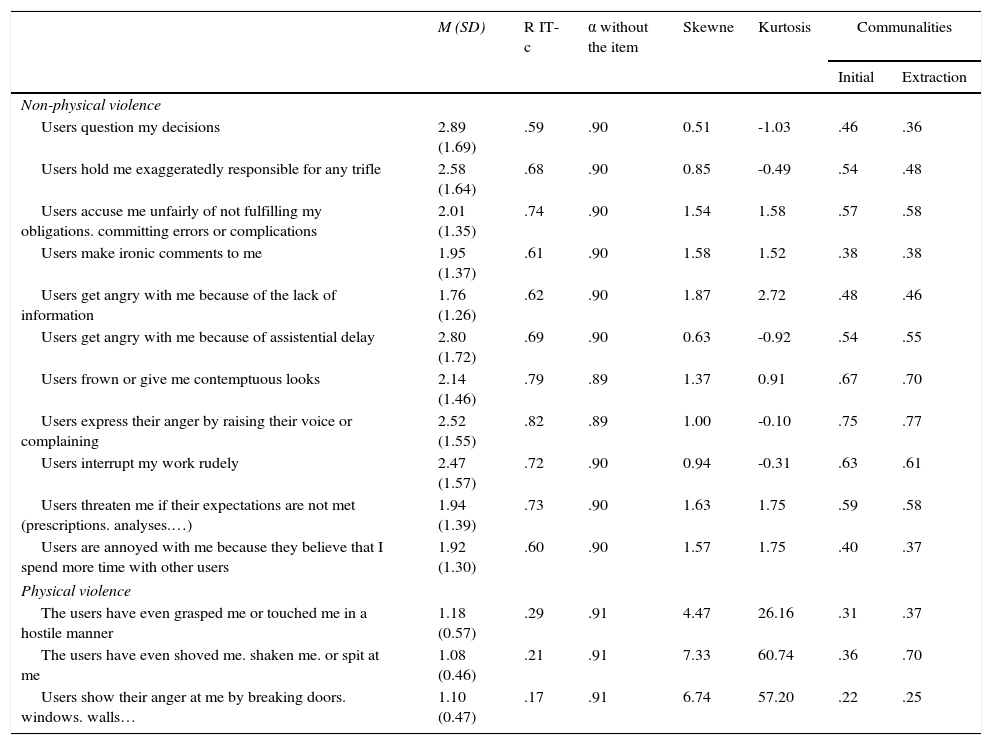
Descriptive statistics of the items.
| M (SD) | R IT-c | α without the item | Skewne | Kurtosis | Communalities | ||
|---|---|---|---|---|---|---|---|
| Initial | Extraction | ||||||
| Non-physical violence | |||||||
| Users question my decisions | 2.89 (1.69) | .59 | .90 | 0.51 | -1.03 | .46 | .36 |
| Users hold me exaggeratedly responsible for any trifle | 2.58 (1.64) | .68 | .90 | 0.85 | -0.49 | .54 | .48 |
| Users accuse me unfairly of not fulfilling my obligations. committing errors or complications | 2.01 (1.35) | .74 | .90 | 1.54 | 1.58 | .57 | .58 |
| Users make ironic comments to me | 1.95 (1.37) | .61 | .90 | 1.58 | 1.52 | .38 | .38 |
| Users get angry with me because of the lack of information | 1.76 (1.26) | .62 | .90 | 1.87 | 2.72 | .48 | .46 |
| Users get angry with me because of assistential delay | 2.80 (1.72) | .69 | .90 | 0.63 | -0.92 | .54 | .55 |
| Users frown or give me contemptuous looks | 2.14 (1.46) | .79 | .89 | 1.37 | 0.91 | .67 | .70 |
| Users express their anger by raising their voice or complaining | 2.52 (1.55) | .82 | .89 | 1.00 | -0.10 | .75 | .77 |
| Users interrupt my work rudely | 2.47 (1.57) | .72 | .90 | 0.94 | -0.31 | .63 | .61 |
| Users threaten me if their expectations are not met (prescriptions. analyses.…) | 1.94 (1.39) | .73 | .90 | 1.63 | 1.75 | .59 | .58 |
| Users are annoyed with me because they believe that I spend more time with other users | 1.92 (1.30) | .60 | .90 | 1.57 | 1.75 | .40 | .37 |
| Physical violence | |||||||
| The users have even grasped me or touched me in a hostile manner | 1.18 (0.57) | .29 | .91 | 4.47 | 26.16 | .31 | .37 |
| The users have even shoved me. shaken me. or spit at me | 1.08 (0.46) | .21 | .91 | 7.33 | 60.74 | .36 | .70 |
| Users show their anger at me by breaking doors. windows. walls… | 1.10 (0.47) | .17 | .91 | 6.74 | 57.20 | .22 | .25 |
Note. M=mean; SD= standard deviation; R IT-c: corrected item-total correlation; α without the item: Cronbach's α if the item is removed.
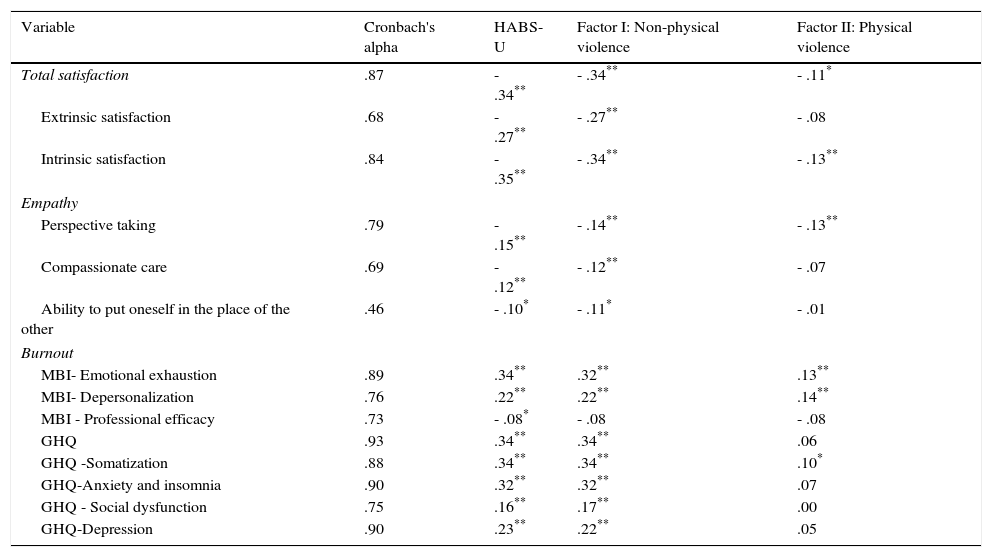
To analyze criterion validity, correlations between the adapted scale and the employed validation scales were calculated (Table 4). Factor I is significantly and negatively related to Job satisfaction (r=-.34, p<.01) and to factors of empathy; and positively to the rest of the validation scales. Factor II is very significantly and negatively related to the factors Intrinsic satisfaction (r=-.14, p<.01) and Perspective taking (r=-.13, p<.01) and positively to the burnout dimension Emotional exhaustion (r=.14, p<.01) and depersonalization (r= .14; p<.01).
Cronbach alpha obtained and correlations between factors and psychosocial variables.
| Variable | Cronbach's alpha | HABS-U | Factor I: Non-physical violence | Factor II: Physical violence |
|---|---|---|---|---|
| Total satisfaction | .87 | - .34** | - .34** | - .11* |
| Extrinsic satisfaction | .68 | - .27** | - .27** | - .08 |
| Intrinsic satisfaction | .84 | - .35** | - .34** | - .13** |
| Empathy | ||||
| Perspective taking | .79 | - .15** | - .14** | - .13** |
| Compassionate care | .69 | - .12** | - .12** | - .07 |
| Ability to put oneself in the place of the other | .46 | - .10* | - .11* | - .01 |
| Burnout | ||||
| MBI- Emotional exhaustion | .89 | .34** | .32** | .13** |
| MBI- Depersonalization | .76 | .22** | .22** | .14** |
| MBI - Professional efficacy | .73 | - .08* | - .08 | - .08 |
| GHQ | .93 | .34** | .34** | .06 |
| GHQ -Somatization | .88 | .34** | .34** | .10* |
| GHQ-Anxiety and insomnia | .90 | .32** | .32** | .07 |
| GHQ - Social dysfunction | .75 | .16** | .17** | .00 |
| GHQ-Depression | .90 | .23** | .22** | .05 |
Note.
Analyzing the annual prevalence of this phenomenon, 90.2% of the workers had suffered some kind of violence; 90.1% reported at least one of the indicators of non-physical violence of the scale, with a minimum annual frequency; and the prevalence of physical violence was 17.3%. The most frequent indicators of non-physical violence (at least monthly) were, firstly, ‘the patients question my decisions’ in 34.9% of the participants, and, secondly, ‘anger because of healthcare delay’ reported by 32.1%. Physical indicators such as ‘jostling and shaking’ and ‘breaking doors and windows’ (in the past year, 5.3% and 8.1%, respectively) were less frequent.
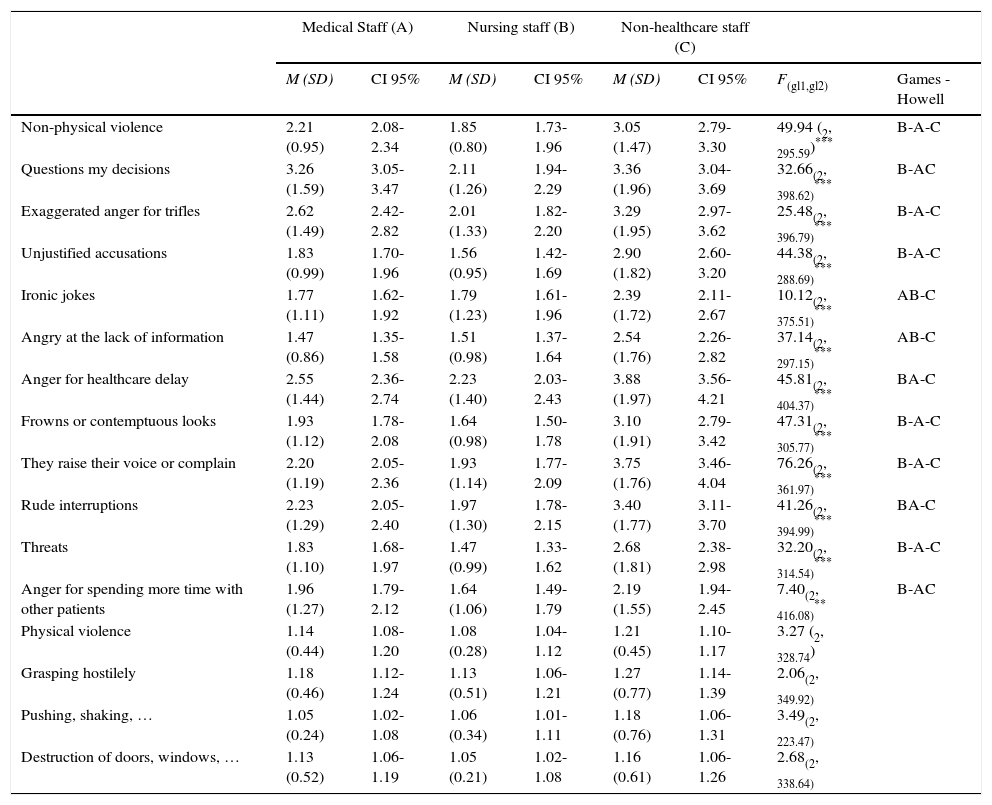
Finally, we determined whether the different occupational groups differed in exposure to user violence. In this sense, we found that, in the items related to ‘exaggerated anger for any trifle ‘(Brown-Forsythe F(2, 396.79)=25.48, p<.001), ‘unjustified accusations’ (Brown-Forsythe F(2, 288.69)=44.38, p<.001), ‘frowns or contemptuous looks’ (Brown-Forsythe F(2, 305.77)=47.31, p<.001), ‘they raise their voice or complain’ (Brown-Forsythe F(2, 361.97)=76.26, p<.001) and ‘threats’ (Brown-Forsythe F(2, 314.54)=32.20, p<.001), the three professional groups presented significant differences, with the nursing staff obtaining a lower mean in all these items. In the items related to ‘ironic jokes’ (Brown-Forsythe F(2, 375.51)=10.12, p<.001), ‘anger due to lack of information’ (Brown-Forsythe F(2, 297.15)=37.14, p<.001), ‘anger for health care delay’ (Brown-Forsythe F(2, 404.37)=45.81, p<.001) and ‘rude interruptions’ (Brown-Forsythe F(2, 404.37)=45.81, p<.001), the non-medical staff presents significant differences with the other professional groups, obtaining higher mean scores. In the items ‘questions my decisions’ (Brown-Forsythe F(2, 398.62)=32.66, p<.001) and ‘angry because I spend more time with other patients’ (Brown-Forsythe F(2, 416.08)=7.40, p<.01), doctors and non-medical staff obtain significantly higher scores than the nursing staff (Table 5).
Relationship between professional group and violence, robust Brown-Forsythe ANOVA.
| Medical Staff (A) | Nursing staff (B) | Non-healthcare staff (C) | ||||||
|---|---|---|---|---|---|---|---|---|
| M (SD) | CI 95% | M (SD) | CI 95% | M (SD) | CI 95% | F(gl1,gl2) | Games -Howell | |
| Non-physical violence | 2.21 (0.95) | 2.08-2.34 | 1.85 (0.80) | 1.73-1.96 | 3.05 (1.47) | 2.79-3.30 | 49.94 (2, 295.59)*** | B-A-C |
| Questions my decisions | 3.26 (1.59) | 3.05-3.47 | 2.11 (1.26) | 1.94-2.29 | 3.36 (1.96) | 3.04-3.69 | 32.66(2, 398.62)*** | B-AC |
| Exaggerated anger for trifles | 2.62 (1.49) | 2.42-2.82 | 2.01 (1.33) | 1.82-2.20 | 3.29 (1.95) | 2.97-3.62 | 25.48(2, 396.79)*** | B-A-C |
| Unjustified accusations | 1.83 (0.99) | 1.70-1.96 | 1.56 (0.95) | 1.42-1.69 | 2.90 (1.82) | 2.60-3.20 | 44.38(2, 288.69)*** | B-A-C |
| Ironic jokes | 1.77 (1.11) | 1.62-1.92 | 1.79 (1.23) | 1.61-1.96 | 2.39 (1.72) | 2.11-2.67 | 10.12(2, 375.51)*** | AB-C |
| Angry at the lack of information | 1.47 (0.86) | 1.35-1.58 | 1.51 (0.98) | 1.37-1.64 | 2.54 (1.76) | 2.26-2.82 | 37.14(2, 297.15)*** | AB-C |
| Anger for healthcare delay | 2.55 (1.44) | 2.36-2.74 | 2.23 (1.40) | 2.03-2.43 | 3.88 (1.97) | 3.56-4.21 | 45.81(2, 404.37)*** | BA-C |
| Frowns or contemptuous looks | 1.93 (1.12) | 1.78-2.08 | 1.64 (0.98) | 1.50-1.78 | 3.10 (1.91) | 2.79-3.42 | 47.31(2, 305.77)*** | B-A-C |
| They raise their voice or complain | 2.20 (1.19) | 2.05-2.36 | 1.93 (1.14) | 1.77-2.09 | 3.75 (1.76) | 3.46-4.04 | 76.26(2, 361.97)*** | B-A-C |
| Rude interruptions | 2.23 (1.29) | 2.05-2.40 | 1.97 (1.30) | 1.78-2.15 | 3.40 (1.77) | 3.11-3.70 | 41.26(2, 394.99)*** | BA-C |
| Threats | 1.83 (1.10) | 1.68-1.97 | 1.47 (0.99) | 1.33-1.62 | 2.68 (1.81) | 2.38-2.98 | 32.20(2, 314.54)*** | B-A-C |
| Anger for spending more time with other patients | 1.96 (1.27) | 1.79-2.12 | 1.64 (1.06) | 1.49-1.79 | 2.19 (1.55) | 1.94-2.45 | 7.40(2, 416.08)** | B-AC |
| Physical violence | 1.14 (0.44) | 1.08-1.20 | 1.08 (0.28) | 1.04-1.12 | 1.21 (0.45) | 1.10-1.17 | 3.27 (2, 328.74) | |
| Grasping hostilely | 1.18 (0.46) | 1.12-1.24 | 1.13 (0.51) | 1.06-1.21 | 1.27 (0.77) | 1.14-1.39 | 2.06(2, 349.92) | |
| Pushing, shaking, … | 1.05 (0.24) | 1.02-1.08 | 1.06 (0.34) | 1.01-1.11 | 1.18 (0.76) | 1.06-1.31 | 3.49(2, 223.47) | |
| Destruction of doors, windows, … | 1.13 (0.52) | 1.06-1.19 | 1.05 (0.21) | 1.02-1.08 | 1.16 (0.61) | 1.06-1.26 | 2.68(2, 338.64) | |
Note. M= medium; SD= standard desviation; CI= Confidence interval.
The development of this study has enabled the adaptation of the HABS-U to the PHC setting. The obtained scale consists of 14 items distributed in two factors. It is short, easy to apply and interpret and presents adequate psychometric properties and structure factor, so it can be concluded that is useful to assess user violence in PHC. The prevalence of workplace violence varies considerably due to the diversity of the physical and non-physical indicators and of scales used to study this phenomenon. Coinciding with the majority of the studies (El-Gilany et al., 2010; Fisekovic et al., 2015; Koritsas, Coles, Boyle, & Stanley, 2007; Skibeli-Joa & Morken, 2012), we found that the indicators of non-physical violence are more frequent than physical violence indicators among PHC professionals. Non-physical violence was experienced by 90.1% of the participants in the current study, compared to 92.1% of the participants in the study of El-Gilany et al. (2010), to 85% of PHC professionals in the study of Moreno-Jiménez et al. (2005) or 55.1% of participants who reported insults and 65.1% shouts in the study of Farias, Sánchez and Acevedo (2012). The annual prevalence of physical violence obtained was 17.3%. We found investigations where this type of violence takes similar figures (Fisekovic et al., 2015; Gascón et al., 2013), although in other studies (El-Gilany et al., 2010; Farias, Sanchez, & Acevedo, 2012) the prevalence of physical violence in PHC professional is lower (about 8%).
As in other publications (El-Gilany et al., 2010; Fisekovic et al., 2015; Magnavita & Heponiemi, 2012), we found differences in the different occupational groups of PHC professionals in their exposure to violent behaviour. In our study, the non-medical staff occupies a prominent place among the professions most exposed to user violence, followed by medical personnel and, finally, the nursing staff. The collective of non-healthcare professionals is acknowledged as being vulnerable to patients’ violent behaviours, given their position at the forefront of patient care and, therefore, they are the first to face users’ frustrations. Magin et al. (2009) carried out a qualitative research focused on this group which highlights that general practice receptionists are subject to considerably frequent workplace violence. However, different studies (El-Gilany et al., 2010; Fisekovic et al., 2015; Gascón et al., 2013; Magnavita & Heponiemi, 2012) found that doctors or nursing staff are the professionals most exposed to violence in PHC. This discrepancy with our results may be due to the different types of samples used in each study.
As to criterion validity, as in many studies, we obtained that exposure to violence can have numerous psychological consequences in the worker. In this sense, analyses have been conducted to predict the consequences of exposure to user violence, finding that professionals exposed to user violence score higher in job dissatisfaction, emotional exhaustion and depersonalization (Bernaldo-De-Quirós et al., 2015; Galián-Muñoz, Ruiz-Hernández, Llor-Esteban, & López-García, 2016; Gascón et al., 2013; Shahzad & Malik, 2014; Trépanier, Fernet, & Austin, 2013).
The present work presents the typical limitations of retrospective studies. We rely on participants’ recall, which may not be accurate when trying to remember events that occurred previously. Unlike other studies of user violence, in our study, all the professional categories present in the PHC centres participated proportionately. Factor II (Physical violence) had moderate internal consistency (α= .68), although it should be taken into account that this property is conditioned by the low number of items that make up this factor and the unusual behaviours described. Therefore, in future works, we will explore the inclusion of new items. The field methodology has generated a notable strength of the study, such as the high response rate (85.7%), unlike similar studies (Koritsas et al., 2007; Miedema et al., 2010). The non-response rate was not random, so it has no impact on the results. In addition, the randomization procedure employed prevented self-selection bias.
The application of this scale could be useful to identify professionals exposed to user violence in order to prioritise and select appropriate individual and collective preventive measures to reduce the possible associated psychological effects. The psychometric properties and use of the HABS-U-PHC would allow assessment of the effectiveness of intervention programmes designed to minimize this problem.
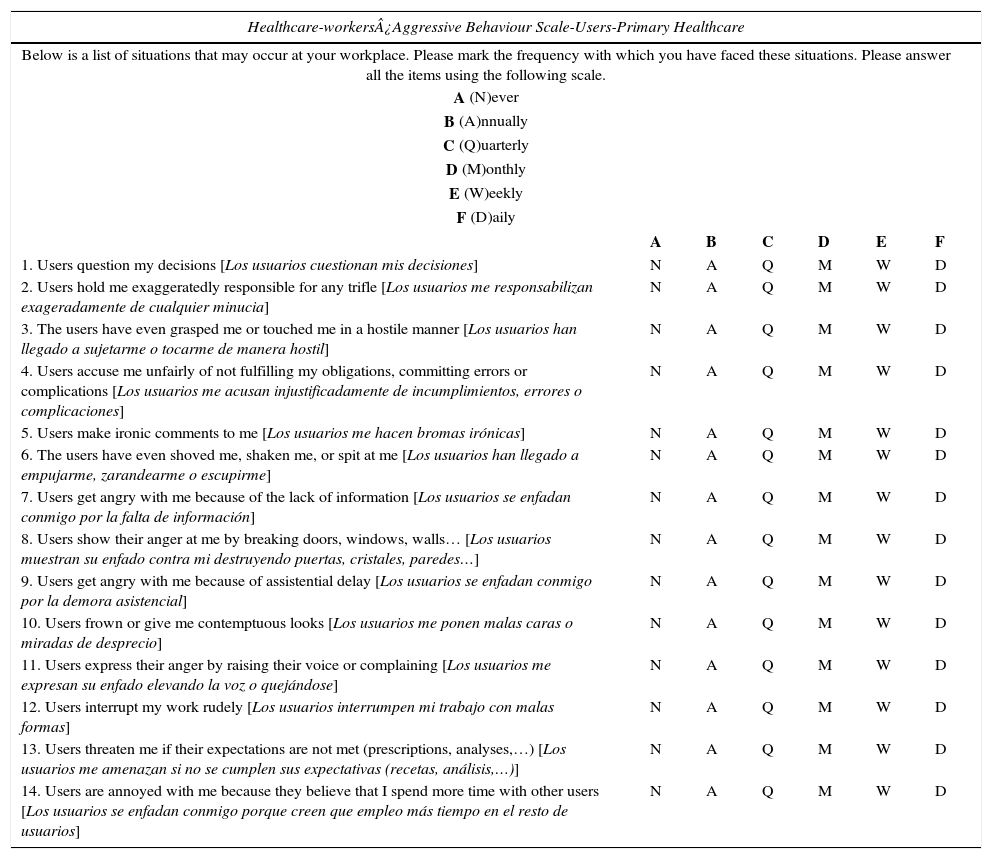
The HABS-U-PHC is included for its dissemination and use as an assessment instrument (Appendix 1), prior to obtaining the authors’ consent.
FundingThe study received an aid for research of the College of Nursing in the Region of Murcia (2013/1412).
We want to express our gratitude to all the professionals involved in the investigation, for their time and dedication, and to the all the PHC centre managers for their collaboration.
| Healthcare-workers¿Aggressive Behaviour Scale-Users-Primary Healthcare | ||||||
|---|---|---|---|---|---|---|
| Below is a list of situations that may occur at your workplace. Please mark the frequency with which you have faced these situations. Please answer all the items using the following scale. | ||||||
| A (N)ever | ||||||
| B (A)nnually | ||||||
| C (Q)uarterly | ||||||
| D (M)onthly | ||||||
| E (W)eekly | ||||||
| F (D)aily | ||||||
| A | B | C | D | E | F | |
| 1. Users question my decisions [Los usuarios cuestionan mis decisiones] | N | A | Q | M | W | D |
| 2. Users hold me exaggeratedly responsible for any trifle [Los usuarios me responsabilizan exageradamente de cualquier minucia] | N | A | Q | M | W | D |
| 3. The users have even grasped me or touched me in a hostile manner [Los usuarios han llegado a sujetarme o tocarme de manera hostil] | N | A | Q | M | W | D |
| 4. Users accuse me unfairly of not fulfilling my obligations, committing errors or complications [Los usuarios me acusan injustificadamente de incumplimientos, errores o complicaciones] | N | A | Q | M | W | D |
| 5. Users make ironic comments to me [Los usuarios me hacen bromas irónicas] | N | A | Q | M | W | D |
| 6. The users have even shoved me, shaken me, or spit at me [Los usuarios han llegado a empujarme, zarandearme o escupirme] | N | A | Q | M | W | D |
| 7. Users get angry with me because of the lack of information [Los usuarios se enfadan conmigo por la falta de información] | N | A | Q | M | W | D |
| 8. Users show their anger at me by breaking doors, windows, walls… [Los usuarios muestran su enfado contra mi destruyendo puertas, cristales, paredes…] | N | A | Q | M | W | D |
| 9. Users get angry with me because of assistential delay [Los usuarios se enfadan conmigo por la demora asistencial] | N | A | Q | M | W | D |
| 10. Users frown or give me contemptuous looks [Los usuarios me ponen malas caras o miradas de desprecio] | N | A | Q | M | W | D |
| 11. Users express their anger by raising their voice or complaining [Los usuarios me expresan su enfado elevando la voz o quejándose] | N | A | Q | M | W | D |
| 12. Users interrupt my work rudely [Los usuarios interrumpen mi trabajo con malas formas] | N | A | Q | M | W | D |
| 13. Users threaten me if their expectations are not met (prescriptions, analyses,…) [Los usuarios me amenazan si no se cumplen sus expectativas (recetas, análisis,…)] | N | A | Q | M | W | D |
| 14. Users are annoyed with me because they believe that I spend more time with other users [Los usuarios se enfadan conmigo porque creen que empleo más tiempo en el resto de usuarios] | N | A | Q | M | W | D |
Cronbach α=.91; Mean= 1.94; Standard Deviation=0.85
Factor I. Non-physical violence (items 1, 2, 4, 5, 7, 9, 10, 11, 12, 13, 14): Cronbach α=.92; Mean= 2.30; Standard deviation =1.16.
Factor II. Physical violence (items 3, 6, 8): Cronbach α=.68; Mean=1.14; Standard deviation =0.44.