Unwanted mental intrusions (UMIs) are the normal variants of obsessions in Obsessive-Compulsive Disorder (OCD), preoccupations about defects in Body Dysmorphic Disorder (BDD), images about illness in Hypochondriasis (HYP), and thoughts about eating in Eating Disorders (EDs). The aim was to examine the similarities and differences in the functional links of four UMI contents, adopting a within-subject perspective. Method: 438 university students and community participants (Mage=29.84, SD=11.41; 70.54% women) completed the Questionnaire of Unpleasant Intrusive Thoughts (QUIT) to assess the functional links (emotions, appraisals, and neutralizing/control strategies) of the most upsetting UMIs with OCD, BDD, HYP and EDs-contents. Results: HYP-related intrusions caused the highest emotional impact, OCD-related intrusions were the most interfering, and EDs-related intrusions interfered the least. The four UMI were equally ego-dystonic. Women appraised OCD-related intrusions more dysfunctionally, but men appraised the four intrusive contents similarly. All UMI instigated the urge to “do something”, to keep them under control and/or neutralizing them. Conclusions: Similarities among the functional links of intrusions related to OCD, BDD, HYP and EDs contents support their transdiagnostic nature and they might contribute to understanding common factors in these disorders.
Las intrusiones mentales no deseadas (IM) son la variante normativa de obsesiones en el Trastorno Obsesivo-Compulsivo (TOC), preocupaciones por defectos en el Trastorno Dismórfico Corporal (TDC), imágenes sobre enfermedad en Hipocondría (TH) y pensamientos sobre alimentación en los Trastornos Alimentarios (TA). El objetivo fue examinar similitudes y diferencias en las relaciones funcionales de los cuatro contenidos de IM, adoptando una perspectiva intra-sujeto.
Método438 estudiantes universitarios y participantes de la comunidad (Medad=29,84; DT=11,41; 70,54% mujeres) completaron el Inventario de Pensamientos Intrusos Desagradables, que evalúa las relaciones funcionales (emociones, valoraciones y estrategias de neutralización/control) de las IM más molestas con contenidos TOC, TDC, TH y TA.
ResultadosLas IM-TH evocaron más emociones negativas, las IM-TOC fueron las que más interfirieron y las IM-TA las que menos. Todas fueron igualmente egodistónicas. Las IM-TOC fueron las más disfuncionalmente valoradas por las mujeres, pero los hombres valoraron los cuatro contenidos de forma similar. Todas las IM promovieron la necesidad de “hacer algo” para controlarla/neutralizarla.
ConclusionesLas similitudes en las relaciones funcionales de intrusiones relacionadas con contenidos del TOC, el TDC, el TH y los TA apoyan su naturaleza transdiagnóstica, pudiendo contribuir a la comprensión de los factores comunes entre esos trastornos.
Unwanted mental intrusions (UMIs) are discrete, untimely, and unexpected conscious cognitive products that can be experienced as thoughts, images, sensations, or impulses. Cognitive models consider UMIs to be the normal variants of clinically significant symptoms, such as obsessions in the Obsessive-Compulsive Disorder (OCD; Clark et al., 2014; Rachman & De Silva, 1978; Radomsky et al., 2014), dysmorphic preoccupations about appearance defects in Body Dysmorphic Disorder (BDD; Giraldo-O’Meara & Belloch, 2017a; Giraldo-O’Meara & Belloch, 2017b; Osman, Cooper, Hackmann, & Veale, 2004), images about illnesses and death in Hypochondriasis (HYP; Arnáez, García-Soriano, & Belloch, 2017; Muse, McManus, Hackmann, Williams, & Williams, 2010), and thoughts and impulses about eating and food in Eating Disorders (EDs; Blackburn, Thompson, & May, 2012; Dakanalis et al., 2015; García-Soriano, Roncero, Perpiñá, & Belloch, 2014).
These disorders also share other characteristics such as comorbidity, course, and age of onset, which support the current inclusion of BDD within the obsessive compulsive and related disorders (OCRD) section of the Diagnostic and Statistical Manual of mental disorders 5th Edition (American Psychiatric Association, 2013). The World Health Organization also currently proposing the inclusion of both BDD and HYP within the OCRD in the upcoming 11 edition of the International Classification of Diseases (i.e., Stein et al., 2016). Regarding EDs and OCD, the two disorders co-occur more frequently than what would be expected by chance (Speranza et al., 2001). This disorders also share high levels of personality traits such as rigidity and persistence (Lucena-Santos, Carvalho, da Silva Oliveira, & Pinto-Gouveia, 2017), a similar prevalence of personality disorders, and among the risk factors for EDs, some studies have identified OCD symptoms during childhood (for a revision, see Belloch, Roncero, & Perpiñá, 2016).
According to the cognitive-behavioral theories about OCD, BDD, HYP, and EDs, the escalation from normal UMIs to clinically significant symptoms lies, first, in the personal meaning that individuals attach to their contents and the emotional distress that the intrusions cause, and second, in the efforts made to neutralize and/or suppress them. Thus, it is assumed that a functional link exists between the experience of an UMI and the dysfunctional appraisals, distress, and behaviors that individuals display to manage the intrusion of an unexpected and/or unwanted thought in the flow of consciousness.
This assumption has been extensively supported by research in the case of OCD (Obsessive Compulsive Cognitions Working Group, OCCWG, 2003, 2005). Regarding BDD, research indicates that intrusive images elicit negative emotions and motivate maladaptive or regulatory behaviors (Giraldo-O’Meara & Belloch, 2017b; Osman et al., 2004). Experts in the area have proposed that dysmorphic “compulsions” (e.g., checking in reflective surfaces, concealing, or making comparisons with others) are triggered by dysmorphic preoccupations (Fang & Wilhelm, 2015; Phillips et al., 2010), and research has shown that dysmorphic concerns are associated with efforts to suppress recurrent intrusive images about appearance defects in non-clinical community individuals (Onden-Lim & Grisham, 2014). As for Hypochondriasis, patients who experience disturbing images about their health increased their estimations of the probability of becoming ill, and respond to these images by engaging in avoidance, checking, seeking reassurance, distraction, and rumination strategies (Muse et al., 2010). Finally, the presence of recurrent UMIs in the form of thoughts, images, and impulses about food, diet, physical exercise, and figure in individuals with EDs produce emotional discomfort, and these intrusive cognitions are usually followed by compensatory behaviors (checking weight, doing exercise, purging, or restricting intake) in an effort to obtain relief (e.g., Avargues-Navarro et al., 2017; Fairburn, Cooper, & Shafran, 2003; García-Soriano et al., 2014).
Taken together, all the above-mentioned studies pose the question of whether the functional consequences of experiencing UMIs might be a common factor among OCD, BDD, HYP, and EDs, and if so, to what extent they might operate transdiagnostically across these disorders (Belloch, 2012). This suggestion coincides with proposals emphasizing the phenomenological and functional similarities among these disorders (Abramowitz & Braddock, 2006; Abramowitz & Jacoby, 2015; Bartz & Hollander, 2006; Deacon & Abramowitz, 2008).
However, to the best of our knowledge, only one study has examined the hypothetical transdiagnostic nature of the functional links of UMIs with OCD and EDs-related contents, using a within-subject approach (Belloch et al., 2016). The results indicate that non-clinical participants with high-scores on OCD and EDs reported a greater frequency of OCD and EDs-related intrusions than individuals without a susceptibility to these disorders, suggesting that the experience of UMIs underlies both OCD and EDs. Moreover, within-subject comparisons showed that in the OCD-risk group, obsessional UMIs had more negative consequences (e.g., emotional distress, dysfunctional appraisals, and neutralizing strategies) than EDs-related intrusions, whereas in the EDs-risk group, both the obsessional and the EDs-related intrusions instigated similar negative functional consequences.
The main aim of the present study was to examine the similarities and differences in the functional links of four UMI contents (OCD, BDD, HYP, and EDs-related) in individuals who had experienced all of these mental intrusions recently. The use of analogue samples to study intrusive thoughts is common in the research about OC-related phenomena and their progression to clinically significant symptoms. Moreover, our study fits the requirements for using analogue samples to draw inferences about clinical participants, i.e., prevalence of symptoms in the sample, dimensionality of symptoms under study, qualitative similarities of symptoms, etiological continuity, and psychological variables relevant to the disorder (Abramowitz et al., 2014). From this perspective, the analyses were focused on the four UMIs that participants selected as the most disturbing, to obtain data closer to the clinical significance of the UMIs than what would be provided by examining the general frequency of these intrusions.
The specific objectives are twofold: first, to compare the emotional impact caused by the four UMIs, their interference in daily activities, the egodystonicity they cause, the dysfunctional appraisals individuals attach to the UMIs, and the thought control and/or neutralizing strategies to manage them; and second, to examine the relationships between the frequency and disturbance caused by the most upsetting OCD-related, BDD-related, HYP-related, and EDs-related intrusions experienced. We hypothesized that there would be no differences in the functional links of the four UMI contents, given the transdiagnostic nature of UMIs.
MethodParticipantsThe total sample consisted of 438 individuals; 290 were undergraduate university students (Mage=24.37, SD=6.90; range=18-26 years; 72.90% women) and 148 were community participants (Mage=40.86, SD=10.75; range=19-60 years; 65.8% women). University students and community participants did not differ on gender distribution, years of education, or socio-economic level, but differences were observed in marital status (χ2=119.03, p<.0001) because most of the students were single (81.7%), and most of the community individuals were married (51.35%). University students were younger than community participants (t=16.59, p<.0001), and women were younger than men in both groups (women: Mage=28.73, SD=11.04 years; men: Mage=32.50; SD=11.90 years; t=3.14, p=.002).
InstrumentsSocio-demographic data sheet. The data required were the following: age, gender, years of education, marital status, and socio-economic level. Two additional questions about the participants’ current mental-health status were also included.
Questionnaire of Unpleasant Intrusive Thoughts (QUIT; Pascual-Vera, Roncero, & Belloch, 2017) is a self-report questionnaire, based on the Revised Obsessional Intrusions Inventory (ROII; Purdon & Clark, 1993), to assess the frequency and discomfort of four sets of unwanted mental intrusions (obsessive, dysmorphic, hypochondriac, and eating disorders-related), and the functional links (emotions, appraisals, and control strategies) of each set of intrusions. Similar to the ROII, the QUIT includes a detailed definition of UMI and the different ways they can be experienced (i.e., as images, thoughts/doubts, impulses, or physical sensations). After the initial description, four separate sets of UMI are presented: OCD-related (12 items), BDD-related (9 items), HYP-related (10 items), and EDs-related (8 items). Respondents must evaluate each UMI on its frequency (from 0=never, to 6=always) and on the disturbance (from 0=not at all, to 4=extremely) the UMI produces when it occurs. In the current study, the Cronbach's alphas of the four UMI contents were satisfactory: OCD-UMIs: frequency α=.84; disturbance α=.82; BDD-UMIs: frequency α=.90; disturbance α=.87; HYP-UMIs: frequency α=.93; disturbance α=.95; EDs-UMIs: frequency α=.91; disturbance α=.93.
After completing each set of UMI, the respondent is asked to choose from the previous list the most upsetting UMI experienced in the past three months with a frequency ≥1. Then, the participant reports the modality/modalities in which s/he experienced the intrusion. Next, the functional consequences associated with the four most upsetting UMIs are evaluated throughout 12 items (from 0=never/not at all, to 4=always/frequently) assessing their emotional distress (anxiety, sadness), interference and egodystonicity, the dysfunctional appraisals the individual attaches to the UMI (thought importance, importance of thought control, and thought-action fusion), and the control and/or neutralizing strategies the subject uses to manage the UMI: do nothing, stop thinking/thought suppression, overt/covert behaviors, self-punishment, and reassurance. The intrusions from each set and its respective functional consequences were selected from validated self-report questionnaires assessing OCD-related intrusions (García-Soriano, Belloch, Morillo, & Clark, 2011), BDD-related intrusions (Giraldo-O’Meara & Belloch, 2017b), hypochondriac (HYP) or illness and death-related intrusions (Arnáez et al., 2017), and EDs-related intrusions (Perpiñá, Roncero, Belloch, & Sánchez-Reales, 2011). The current study focused in the functional consequences associated with the most upsetting OCD, BDD, HYP, and EDs-related intrusions.
ProcedureParticipants were recruited by the authors from the students who attended their lectures at the University of Valencia (Spain), as well as through advertisements on the university campus and on the web page of the research group (www.itoc.org.es) requesting voluntary participation in a study on values and beliefs about unpleasant thoughts. Potential participants were invited to contact one of the authors for an interview. In this interview, they were informed about the study's general purpose and assessment procedure, and asked for their explicit consent to participate. Once the informed consent was signed, participants were scheduled to attend an assessment session where they were provided with a booklet containing the socio-demographic data sheet and the QUIT. These sessions were conducted in groups of 25-35 individuals in the presence of one of the authors (B.P-V). Participants who reported having mental health problems in the past 6 months, who were undergoing psychological or pharmacological treatment, or were not in the 18-to-60-age range, were not included in data analyses. Participants did not receive any compensation for their participation. The study received the approval of the University Ethics committee.
Data analysesAn alpha level of .05 (two-tailed) was used for all statistical tests. Gender differences were calculated (unpaired t test, and Cohen's d). The consequences that each participant experienced due to his/her four most disturbing UMIs were examined using a repeated-measures within-subject design (MANOVA). Bonferroni adjustments for multiple-comparison post hoc analyses were also computed. Effect sizes (ηp2) were calculated. Pearson correlations among target variables were calculated. Separate analyses were performed in women and men given previous results indicating gender differences on frequency and disturbance caused by UMIs (Arnáez et al., 2017; García-Soriano et al., 2011; Giraldo-O’Meara & Belloch, 2017b; Pascual-Vera et al., 2017). Data were analyzed using IMB SPSS Statistics (version 22). G*Power (version 3) was used to calculate the sample size required (N=60) and the corresponding statistical power (η2p=.06; effect size f=.2526456) for repeated-measures within-subject design (MANOVA).
ResultsPreliminary dataUp to 49.1% of participants (185 women, 49 men) reported having experienced the four most upsetting intrusive contents with a frequency and discomfort ≥1 in the past three months. Consequently, only data from this sample will be considered for analyses.
In both women and men, the most disturbing intrusions were related to doubts about leaving something on (women: 25.4%; men: 18.4%), defects and defective bodily functions (women: 16.2%; men: 22.4%), and physical symptoms (women: 18.4%; men: 24.5%) for OCD, BDD, and HYP-related intrusions, respectively. The most disturbing EDs-related intrusions were related to physical appearance in women (42.2%) and to dieting in men (28.6%).
Regarding the modality, 62.35% of participants had experienced the most upsetting UMI in one modality, whereas 37.65% had experienced it in more than one form/modality. The four UMI appeared mainly as a thought-doubt, followed by an image, but they were scarcely experienced as an impulse or physical sensation.
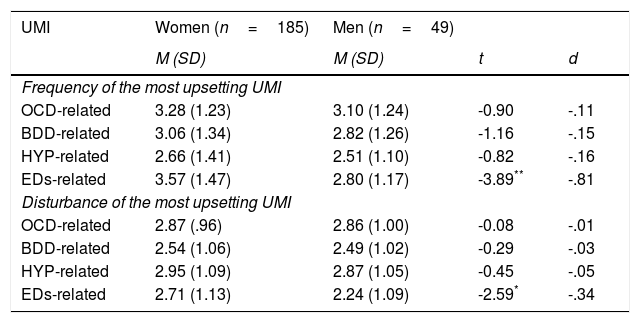
As Table 1 shows, the mean frequency and discomfort caused by the four most upsetting UMIs was moderate. Women and men experienced the OCD, BDD, and HYP-related intrusions with similar frequency and discomfort. The EDs-related UMIs were experienced more frequently and caused greater discomfort in women than in men. Age was related to the consequences of the UMI (e.g., emotions, appraisals, and control strategies) in women (range: r=-.23 to -.15) and in men (range: r=.35 to .36).
Gender differences in the frequency and disturbance of the four most upsetting unwanted mental intrusions (UMI).
| UMI | Women (n=185) | Men (n=49) | ||
|---|---|---|---|---|
| M (SD) | M (SD) | t | d | |
| Frequency of the most upsetting UMI | ||||
| OCD-related | 3.28 (1.23) | 3.10 (1.24) | -0.90 | -.11 |
| BDD-related | 3.06 (1.34) | 2.82 (1.26) | -1.16 | -.15 |
| HYP-related | 2.66 (1.41) | 2.51 (1.10) | -0.82 | -.16 |
| EDs-related | 3.57 (1.47) | 2.80 (1.17) | -3.89** | -.81 |
| Disturbance of the most upsetting UMI | ||||
| OCD-related | 2.87 (.96) | 2.86 (1.00) | -0.08 | -.01 |
| BDD-related | 2.54 (1.06) | 2.49 (1.02) | -0.29 | -.03 |
| HYP-related | 2.95 (1.09) | 2.87 (1.05) | -0.45 | -.05 |
| EDs-related | 2.71 (1.13) | 2.24 (1.09) | -2.59* | -.34 |
Note. OCD: Obsessive-Compulsive Disorder; BDD: Body Dysmorphic Disorder; HYP: Hypochondriasis; EDs: Eating Disorders.
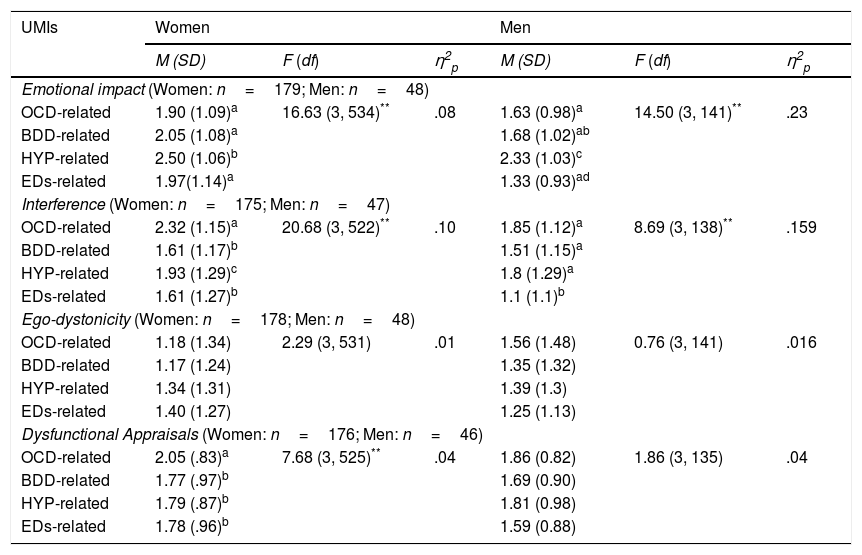
As Table 2 reveals, the F values were significant, indicating that the four sets of UMIs differed in the emotional impact they caused. The post-hoc analyses, in both women and men, indicated that the HYP-related intrusions were assessed as having a significantly higher emotional impact than the other three intrusive contents. The OCD and BDD-related intrusions caused similar emotional distress, whereas only in women the EDs-related intrusions instigated negative emotions comparable to those caused by the OCD and BDD-related intrusions. In the men's group, the EDs-related UMIs caused less emotional distress than the BDD intrusions.
Within-subject differences in emotional impact, interference, ego-dystonicity and dysfunctional appraisals associated with the four most upsetting unwanted mental intrusions (UMIs).
| UMIs | Women | Men | ||||
|---|---|---|---|---|---|---|
| M (SD) | F (df) | η2p | M (SD) | F (df) | η2p | |
| Emotional impact (Women: n=179; Men: n=48) | ||||||
| OCD-related | 1.90 (1.09)a | 16.63 (3, 534)** | .08 | 1.63 (0.98)a | 14.50 (3, 141)** | .23 |
| BDD-related | 2.05 (1.08)a | 1.68 (1.02)ab | ||||
| HYP-related | 2.50 (1.06)b | 2.33 (1.03)c | ||||
| EDs-related | 1.97(1.14)a | 1.33 (0.93)ad | ||||
| Interference (Women: n=175; Men: n=47) | ||||||
| OCD-related | 2.32 (1.15)a | 20.68 (3, 522)** | .10 | 1.85 (1.12)a | 8.69 (3, 138)** | .159 |
| BDD-related | 1.61 (1.17)b | 1.51 (1.15)a | ||||
| HYP-related | 1.93 (1.29)c | 1.8 (1.29)a | ||||
| EDs-related | 1.61 (1.27)b | 1.1 (1.1)b | ||||
| Ego-dystonicity (Women: n=178; Men: n=48) | ||||||
| OCD-related | 1.18 (1.34) | 2.29 (3, 531) | .01 | 1.56 (1.48) | 0.76 (3, 141) | .016 |
| BDD-related | 1.17 (1.24) | 1.35 (1.32) | ||||
| HYP-related | 1.34 (1.31) | 1.39 (1.3) | ||||
| EDs-related | 1.40 (1.27) | 1.25 (1.13) | ||||
| Dysfunctional Appraisals (Women: n=176; Men: n=46) | ||||||
| OCD-related | 2.05 (.83)a | 7.68 (3, 525)** | .04 | 1.86 (0.82) | 1.86 (3, 135) | .04 |
| BDD-related | 1.77 (.97)b | 1.69 (0.90) | ||||
| HYP-related | 1.79 (.87)b | 1.81 (0.98) | ||||
| EDs-related | 1.78 (.96)b | 1.59 (0.88) | ||||
Note, *p<.05. Superscripts a,b,c,d indicate post-hoc within-group differences (Bonferroni). Same superscript indicates no differences; different superscripts differ significantly at p≤.05. OCD: Obsessive-Compulsive Disorder; BDD: Body Dysmorphic Disorder; HYP: Hypochondriasis; EDs: Eating Disorders.
Regarding the interference caused by the four UMI contents, the F values were also significant, indicating that the different UMIs provoked different interference, in both women and men. The post-hoc analyses in the women's group indicated that OCD-related intrusions were the most interfering, whereas the BDD and EDs-related intrusions were the least interfering. In the men's group, OCD, BDD, and HYP-related intrusions were the most interfering, whereas the EDs-related intrusions interfered significantly less. In both women and men, OCD, BDD, HYP, and EDs-related intrusions were assessed as equally ego-dystonic, regardless of their content.
As for dysfunctional appraisals, the F values were significant in the women's group, indicating that the OCD-related intrusions were assessed as more dysfunctional than the other three sets of intrusions. By contrast, BDD, HYP, and EDs-related intrusions were similarly appraised. In the men's group, the four sets of intrusions were assessed equally in terms of dysfunctional appraisals.
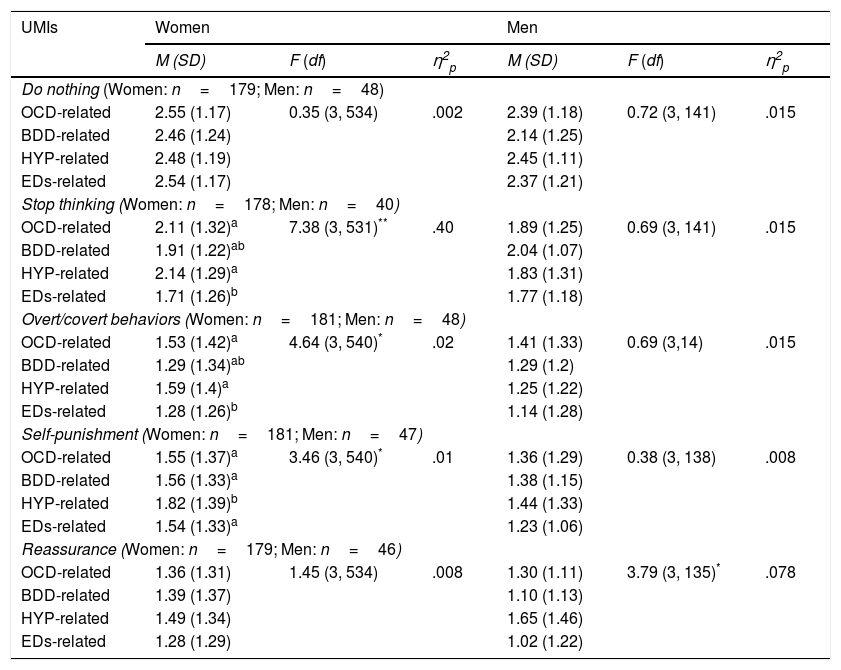
The results for the five thought-control strategies used to manage the four most upsetting UMIs appear in Table 3. The F values were not significant for the strategy do nothing with the UMI. In the women's group, the four modalities of intrusions differed in the use of stop-thinking. The post-hoc analyses indicate no differences in the use of this strategy to manage OCD, BDD, and HYP-related intrusions, but it was used significantly less to manage EDs-related intrusions. The main source of differences was between the low use of stop thinking to manage EDs intrusions compared to its high use to keep OCD and HYP intrusions under control. By contrast, in men, stop thinking was used similarly to manage the four UMIs.
Within-subject differences in the thought control strategies used to manage the four most upsetting unwanted mental intrusions (UMIs).
| UMIs | Women | Men | ||||
|---|---|---|---|---|---|---|
| M (SD) | F (df) | η2p | M (SD) | F (df) | η2p | |
| Do nothing (Women: n=179; Men: n=48) | ||||||
| OCD-related | 2.55 (1.17) | 0.35 (3, 534) | .002 | 2.39 (1.18) | 0.72 (3, 141) | .015 |
| BDD-related | 2.46 (1.24) | 2.14 (1.25) | ||||
| HYP-related | 2.48 (1.19) | 2.45 (1.11) | ||||
| EDs-related | 2.54 (1.17) | 2.37 (1.21) | ||||
| Stop thinking (Women: n=178; Men: n=40) | ||||||
| OCD-related | 2.11 (1.32)a | 7.38 (3, 531)** | .40 | 1.89 (1.25) | 0.69 (3, 141) | .015 |
| BDD-related | 1.91 (1.22)ab | 2.04 (1.07) | ||||
| HYP-related | 2.14 (1.29)a | 1.83 (1.31) | ||||
| EDs-related | 1.71 (1.26)b | 1.77 (1.18) | ||||
| Overt/covert behaviors (Women: n=181; Men: n=48) | ||||||
| OCD-related | 1.53 (1.42)a | 4.64 (3, 540)* | .02 | 1.41 (1.33) | 0.69 (3,14) | .015 |
| BDD-related | 1.29 (1.34)ab | 1.29 (1.2) | ||||
| HYP-related | 1.59 (1.4)a | 1.25 (1.22) | ||||
| EDs-related | 1.28 (1.26)b | 1.14 (1.28) | ||||
| Self-punishment (Women: n=181; Men: n=47) | ||||||
| OCD-related | 1.55 (1.37)a | 3.46 (3, 540)* | .01 | 1.36 (1.29) | 0.38 (3, 138) | .008 |
| BDD-related | 1.56 (1.33)a | 1.38 (1.15) | ||||
| HYP-related | 1.82 (1.39)b | 1.44 (1.33) | ||||
| EDs-related | 1.54 (1.33)a | 1.23 (1.06) | ||||
| Reassurance (Women: n=179; Men: n=46) | ||||||
| OCD-related | 1.36 (1.31) | 1.45 (3, 534) | .008 | 1.30 (1.11) | 3.79 (3, 135)* | .078 |
| BDD-related | 1.39 (1.37) | 1.10 (1.13) | ||||
| HYP-related | 1.49 (1.34) | 1.65 (1.46) | ||||
| EDs-related | 1.28 (1.29) | 1.02 (1.22) | ||||
Note. Superscripts a,b,c,d indicate post-hoc within-group differences (Bonferroni). Same superscript indicates no differences; different superscripts differ significantly at p≤.05. OCD: Obsessive-Compulsive Disorder; BDD: Body Dysmorphic Disorder; HYP: Hypochondriasis; EDs: Eating Disorders.
Furthermore, the F values were significant for the use of overt/covert behaviors in women. The main source of differences was between the highest use of these strategies to keep HYP intrusions under control, compared to their low use to control BDD and EDs-related intrusions. However, data showed that, in the men's group, overt/covert behaviors were used similarly to control all the UMIs, regardless of their specific contents. In the women's group, the four modalities of intrusions differed in the use of self-punishment, whereas no differences were found in men. Women punished themselves more when experiencing HYP intrusions than when they had the other modalities of intrusions.
Finally, F values were significant for the use of reassurance in men, whereas no differences were found in women. In men, post-hoc analyses indicate that reassurance was used more to manage HYP intrusions than EDs-related intrusions. No differences were found in the use of reassurance to manage HYP, OCD, and BDD-related intrusions.
Relationships between the frequency and distress provoked by the most upsetting OCD, BDD, HYP, and ED-related unwanted mental intrusionsIn the women's group, the four sets of UMIs were associated in terms of frequency (r range from .43 to .16; all p's≤.05) and disturbance (r range from .45 to .19; all p's≤.05), except for the association between the disturbance caused by EDs- and HYP-related intrusions (r=.13). For both frequency and disturbance, the largest coefficients were found between the most upsetting EDs and BDD intrusions (frequency r=.43; discomfort r=.45).
In the men's group, the frequency of BDD intrusions was related to the frequency of the EDs (r=.38, p≤.01), OCD (r=.31, p≤.05), and HYP intrusions (r=.29, p≤.05), but no other relationships were found. Regarding discomfort, the four most disturbing UMIs were significantly related, ranging from r=.49, p≤.01 (OCD and BDD) to r=.37, p≤.01 (BDD and EDs). However, there were no correlations between the disturbance caused by the most upsetting HYP and OCD UMIs (r=.28, p≥.05), or between the disturbance caused by the HYP and EDs-related UMIs (r=.26, p≥.05).
DiscussionThis is the first study to examine the hypothetical transdiagnostic nature of the functional links of UMIs with obsessive, dysmorphic, hypochondriac, and eating-disorders contents, using a within-subject approach. We focused on four specific disorders, OCD, BDD, HYP, and EDs, because of their phenomenological similarities, such as the experience of UMIs with contents related to the specific fear of each disorder.
Our findings showed that up to fifty percent of the total sample reported having experienced the four UMIs in the past three months. This is an important rate, that supports the putative transdiagnostic nature of UMIs (Belloch, 2012; Pascual-Vera et al., 2017). The fact that more than two-thirds of the participants who experienced the four UMI contents were women, posit the necessity to explore in depth the reasons and/or mechanisms that explain gender differences regarding the experience of UMIs and its consequences (Dakanalis et al., 2016).
The first objective was to compare the consequences of the four UMI contents. The results suggest that, for both women and men, the HYP-related intrusions caused the highest emotional distress, and the OCD-related intrusions were the most interfering, whereas EDs-related intrusions interfered less, which is consistent with previous research (Belloch et al., 2016). Furthermore, the four UMIs were equally ego-dystonic, which does not coincide with other studies where EDs intrusions were assessed as less egodystonic than OCD intrusions (Belloch, Roncero, & Perpiñá, 2012). The low scores and the fact that egodystonicity was assessed with a single item in this study might explain the discrepancy.
The OCD-related intrusions were appraised as the most dysfunctional by women, but men appraised the four intrusive contents similarly. These results support the role of faulty appraisals in OCD (Kyrios, Hordern, & Fassnacht, 2015; OCCWG, 2003, 2005), but they might indicate that dysfunctional appraisals also play an important role in the etiology and/or the maintenance of other disorders, such as EDs, HYP, and BDD. This notion has been extensively supported in the case of EDs (e.g., Fairburn et al., 2003; García-Soriano et al., 2014), and it has also been proposed in current cognitive models of hypochondriasis (Muse et al., 2010; Rachman, 2012) and BDD (Fang & Wilhelm, 2015).
The four UMIs instigated the urge to “do something”, supporting the functional link between an unwanted mental intrusion and behavior to alleviate the discomfort it causes, which has been largely supported by OCD research (e.g., Belloch, Carrió, Cabedo, & García-Soriano, 2015; Salkovskis, 1985). Nonetheless, some differences emerged in the use of specific strategies, taking into account the intrusive content and the gender. Women used less though-suppression and overt/covert behaviors when they experienced EDs-related intrusions, they punished themselves more when having HYP-related intrusions, and they sought reassurance equally to manage OCD, BDD, HYP, and EDs-related intrusions. Men used thought-suppression, overt/covert behaviors, and self-punishment in the same way to keep the four UMIs under control, but they sought reassurance less when experiencing EDs-related intrusions. Stop thinking or thought suppression has been largely investigated in OCD (e.g., Belloch, Morillo, & Giménez, 2004; Purdon & Clark, 2001). Our results showed that men used this strategy similarly to manage the four intrusive contents, but it was not used by women to manage the EDs-related intrusions. This result is consistent with studies reporting that patients with EDs often used strategies that were hardly used by OCD patients, such as doing what the intrusions says (e.g., burn calories, fast or vomit) or just doing nothing (e.g., “my thought reminds me that I’m doing the right thing”) (Belloch et al., 2016; Dakanalis et al., 2015).
The second objective was to examine the relationships between the frequency and disturbance caused by the four most upsetting intrusions experienced by participants. Data showed a stronger pattern of associations among the four most upsetting contents in women than in the men. In women, the highest association was between the frequency and disturbance of EDs and BDD intrusions, which agrees with the high comorbidity rates between EDs and BDD (Kollei, Schieber, de Zwaan, Svitak, & Martin, 2013). In the men's group, only the frequency of BDD-related intrusions correlated with the frequency of the other three intrusive contents. The associations between BDD and OCD-related intrusions support the phenomenological similarities between the two disorders (Osman et al., 2004; Phillips et al., 2010) and their high comorbidity rates (Bienvenu et al., 2012). The large correlation between BDD and HYP-related intrusions might support the inclusion of Hypochondriasis in the obsessive-compulsive spectrum disorders (Kogan et al., 2016; Stein et al., 2016).
Taken together, the results generally support our hypothesis about the similarities among the functional links of the intrusions related to four different clinical disorders, which might help to understand the common factors in these disorders, reflected by their comorbidity rates as well as by their similar response to treatments.
Several limitations of the study should be mentioned. First, the participants were mainly young healthy women. Consequently, the frequency with which they experience UMIs was generally low, which means that our data may have floor effects. Although the use of non-clinical samples is adequate to explore dimensional variables such as UMIs, it is necessary to support the results with clinical participants. Second, the study results rely exclusively on a self-report questionnaire. We have tried to overcome this limitation by designing the QUIT on the basis of previously validated self-reports, but future studies should include other data collection methods, such as structured interviews.
Further studies should test specifically the concurrent validity of the QUIT with symptom measures of OCD, BDD, HYP, and EDs, with both non-clinical and clinical participants, as well as to find out cutoff points on the QUIT scores to differentiate normalcy from psychopathology. Moreover, additional analyses under the item response theory framework should be conducted in order to explore in depth and to improve the psychometric properties of the QUIT.
FundingThis study was supported by the Spanish Ministerio de Economía y Competitividad, MINECO (Grant PSI2013-44733-R).