Physical exercise may alleviate premature ejaculation symptoms, a prevalent male sexual dysfunction linked to a series of negative outcomes for men and their partners.
ObjectiveWe investigated the effectiveness of high-intensity interval training (HIIT) and slow breathing interventions on premature ejaculation symptoms and their relation to autonomic activity and attention regulation.
MethodChinese adult men (N = 76, M = 21.89, SD = 3.32) with premature ejaculation completed one of the two-week interventions in their homes or as participants in a normal breathing control group; they reported their age, height, weight, physical activity level, premature ejaculation symptoms, and attention regulation. In the HIIT group, 26 participants engaged in a 7-minute HIIT each day. In the slow breathing group, 25 participants performed 7-minute slow breathing exercises per day while the 25 participants in the normal breathing group similarly performed normal breathing exercises. All participants measured their heart rate once before and five times (with one-minute intervals) after the intervention. When participants had penile-vaginal sex with their partners, they measured their heart rate once after ejaculation.
ResultsTime × Intervention interaction was significant with lower levels of premature ejaculation symptoms on Days 12, 13, and 14 in the HIIT group (M ± SD = 16.19 ± 3.45, 15.96 ± 3.43, and 15.15 ± 3.62) compared to the normal breathing group (M ± SD = 17.68 ± 3.06, 17.68 ± 3.15, and 17.44 ± 3.25). Higher levels of attention regulation were associated with fewer premature ejaculation symptoms. We also found that a larger increase in heart rate from resting to after sex was associated with fewer premature ejaculation symptoms.
ConclusionCompared to the control group, the efficacy of two weeks of HIIT exercise in mitigating PE symptoms suggests its potential as a novel treatment for PE.
PE is characterized by a man's inability to maintain ejaculatory control as desired, resulting in a short intravaginal ejaculation latency time (IELT), such as ejaculating within one minute of penetration (Althof et al., 2014), which in turn leads to sexual distress as well as diminished self-esteem and self-confidence (Rowland et al., 2007; Symonds et al., 2003) and heightened levels of anxiety and depression (Ermeç et al., 2022; Porst et al., 2007), increased interpersonal difficulties (Giuliano et al., 2008; Patrick et al., 2005), and an altered rewarding processing (Y. Li et al., 2023). Furthermore, men suffering from PE symptoms have female sexual partners with reduced relationship and sexual satisfaction, elevating the risk of sexual dysfunction (Jern et al., 2020; Zhang et al., 2020).
The selective serotonin reuptake inhibitors (dapoxetine and paroxetine) have demonstrated an ejaculation-delaying effect (Kilinc et al., 2018; Rohilla et al., 2020). However, medical treatment has the risk of side effects and high cost (Park et al., 2017). Also, many men discontinue these treatments because of the side effects (Mondaini et al., 2013). Therefore, we aimed to develop a new treatment without negative side effects.
Sympathovagal imbalance hypothesisThe cause of PE is unknown (Althof et al., 2014). Sympathovagal imbalance has been proposed as a potential etiological factor (Erbay & Ceyhun, 2021; Rowland, 2010; Xia et al., 2014). It refers to an autonomic state characterized by hyperactivity in the sympathetic nervous system and hypoactivity in the parasympathetic nervous system. In the male sex response, initially, parasympathetic activity facilitates erection. Subsequently, during the ejaculation phase, the sympathetic activity facilitates the emission of seminal fluid (Alwaal et al., 2015).
Men with PE exhibit heightened and earlier sympathetic activation levels compared to sexually functional controls, both in non-aroused (Xia et al., 2014) and sexually aroused contexts (Rowland, 2010). Additionally, men with PE manifest lower parasympathetic activity and a higher sympathetic/parasympathetic ratio, which is an indicative measure of sympathovagal imbalance compared to a control group, especially a ratio surpassing 2.7 emerged as a highly sensitive predictor of PE (Erbay & Ceyhun, 2021). Overall, we assumed that sympathovagal imbalance plays some role in the etiology of PE.
Interoceptive awarenessInteroceptive awareness encompasses an individual's capacity to recognize, identify, and adeptly respond to internal signals emanating from their body (Craig, 2002; Mehling et al., 2012; Strigo & Craig, 2016), for example, heartbeat. Attention to bodily sensations is crucial for sexual function (Costa et al., 2016). As part of interoceptive awareness, attention regulation refers to the capacity to sustain and manage attention directed toward bodily sensations (Mehling et al., 2012). Low interoceptive awareness is associated with difficulty delaying ejaculation (Berenguer et al., 2019). Therefore, we hypothesized that heightened attention regulation would lead to more accurate sensations of sexual stimulation and the approaching orgasmic threshold allowing an adjustment of sexual stimulation and excitability resulting in delayed ejaculation.
Physical exercise also enhances interoceptive accuracy (Wallman-Jones et al., 2022) for perceiving interoceptive signals (Ferentzi et al., 2018), which is linked with interoceptive awareness (Garfinkel et al., 2015). Therefore, we hypothesized that a physical exercise would enhance interoceptive awareness, especially for attention regulation, consequently mitigating PE symptoms in men with PE.
High-intensity interval training (HIIT)A systematic review has shown that physical exercise interventions consistently reduce PE symptoms, without generating any negative side effects (Niu & Santtila, 2023). For example, engaging in moderate physical exercise training five times a week for 30 days led to an improvement in IELT among men with PE (Kilinc et al., 2018).
HIIT, characterized by repeated bouts of high-intensity physical exercises interspersed with short recovery intervals, reduces more sympathovagal imbalance compared to moderate-intensity continuous training (Alansare et al., 2018; Besnier et al., 2019; Ito, 2019); however, this does not apply to individuals with heart problems (Koufaki et al., 2014). A two-week HIIT intervention can alleviate PE symptoms in men with PE (Niu, Wen et al., 2023), especially for men who attain a sufficient HR increase during the HIIT intervention. However, the sample size in the latter study was small, and there was a lack of control for whether the participants made sufficient effort during the HIIT intervention. Considering that men with PE exhibit more sympathovagal imbalance symptoms (Erbay & Ceyhun, 2021) and physical exercise can improve interoceptive awareness (Wallman-Jones et al., 2022), we assumed that the HIIT intervention with sufficient HR increase would improve sympathovagal balance and interoceptive awareness which in turn would alleviate PE symptoms in men with PE.
Slow breathingSlow breathing refers to a low frequency (e.g., 5 breaths per minute) respiratory rhythm. Slow breathing interventions (5 to 8 breaths per minute) may improve sympathovagal balance (Fonkoue et al., 2018; C. Li et al., 2018) compared with normal breathing (14 to 16 breaths per minute). Also, slow breathing decreases sympathetic activity (Busch et al., 2012) and is associated with better interoceptive accuracy (Leganes-Fonteneau et al., 2021; Rominger et al., 2021). Therefore, we assumed the slow breathing intervention may also improve the sympathovagal balance and interoceptive awareness which in turn would reduce PE symptoms in men with PE.
Heart rate (HR)HR refers to the number of times the heart beats in a period of time, typically measured in beats per minute (bpm). The dynamics of HR and its variability are intricately influenced by the interplay between sympathetic and parasympathetic activity (Vitale et al., 2019). During physical exercise, sympathetic activity increases which in turn increases the HR and leads to energy expenditure, and parasympathetic activity decreases (Vitale et al., 2019). After physical exercise, parasympathetic activity restores the HR to its resting baseline while sympathetic activity diminishes (Vitale et al., 2019). Therefore, individuals who engage in more physically straining efforts (i.e., higher jumps and harder body movement) during HIIT exercise may have elevated sympathetic activity which in turn contributes to a greater increase in the HR rise from the baseline. We considered the HR increase during the HIIT intervention to be an index of the physical exertion of participants engaging in HIIT. A previous study found an association between the HR increase during HIIT and fewer PE symptoms (Niu, Wen et al., 2023). Therefore, we hypothesized an increase in HR during HIIT could be linked to PE symptom reduction.
Sexual intercourse for men has moderate physical demands that vary depending on contextual variables, for example, intercourse position and duration (Oliva-Lozano et al., 2022). Considering the association between physical activity and HR, we hypothesized that men with fewer PE symptoms would have more physical activity during sex which would subsequently lead to a larger HR increase from resting to after sex.
HR recoveryHR recovery refers to the ability of the autonomic regulation to return the HR of an individual to the baseline level from its highest values following an intense physical exercise (Peçanha et al., 2014), for example, the reduction of HR within the 60 s after the physical exercise (Fecchio et al., 2019). Recovery is characterized by a concurrent decrease in sympathetic activity and an increase in parasympathetic activity (Peçanha et al., 2014). Turan and Gürel (2020) found impaired HR recovery in men with PE following stress tests, signifying excessive sympathetic and deficient parasympathetic activation in this cohort compared to a control group (Turan & Gürel, 2020).
Sympathovagal imbalance is associated with sympathetic overactivity (Alvares et al., 2016). Therefore, a poorer HR recovery could be considered an index reflecting sympathovagal imbalance (Peçanha et al., 2014; Turan & Gürel, 2020). Based on the established effects of the HIIT interventions on the sympathovagal imbalance (Alansare et al., 2018; Besnier et al., 2019; Ito, 2019), we assumed that the HIIT intervention would lead to better HR recovery which in turn would alleviate PE symptoms.
HypothesesWe expected that higher levels of pre-intervention physical activity levels (Hypothesis 1) and attention regulation (Hypothesis 2) would be associated with fewer PE symptoms.
We expected PE symptoms to decrease following HIIT and slow breathing interventions [vs. normal breathing control]. Specifically, we tested Hypothesis 3a: Time (Day 1 vs. Day 14) × Group (HIIT vs. Slow breathing vs. Normal breathing) interaction, and Hypothesis 3b: Day (1 to 14) × Group (HIIT vs. Slow breathing vs. Normal breathing) interaction.
We expected attention regulation to increase while engaging in HIIT and slow breathing interventions [vs. normal breathing control]. Specifically, we tested Hypothesis 4a: Time (Day 1 vs. Day 14) × Group (HIIT vs. Slow breathing vs. Normal breathing) interaction and Hypothesis 4b: Day (1 to 14) × Group (HIIT vs. Slow breathing vs. Normal breathing) interaction.
We also expected attention regulation to improve (Hypothesis 5a) and the HR to change to an increase from resting to after sex (Hypothesis 5b) during the HIIT and slow breathing interventions. Additionally, we expected the HR to change to an increase from resting to after the HIIT intervention (Hypothesis 5c), and the HR recovery after the HIIT intervention to improve [i.e. increase] (Hypothesis 5d), during the HIIT intervention.
We expected that an improved attention regulation (Hypothesis 6a) and a larger HR increase from resting to after sex (Hypothesis 6b) would be related to fewer PE symptoms while engaging in HIIT and slow breathing interventions. Additionally, we expected a larger HR increase from resting to after the HIIT intervention (Hypothesis 6c) and an improved HR recovery after the HIIT intervention (Hypothesis 6d) to be associated with fewer PE symptoms.
MethodsPreregistrationWe pre-registered the sample size, hypotheses, variables, experimental conditions, and planned analyses for this study on the As Predicted website before the commencement of data collection: https://aspredicted.org/28V_99G.
ParticipantsTo assess the requisite sample size, we conducted an a priori power analysis using G*Power 3.1 (Faul et al., 2007) for two ANOVAs that are characterized by repeated measurement and within-between interaction design. The analysis indicated that a minimum sample size of 66 (22 for each group) is required for a 2 Time (Day 1 vs. Day 14) × 3 Intervention (HIIT vs. Slow breathing vs. Normal breathing) design and a sample size of 21 (7 for each group) participants for a 14 Day (1 to 14) × 3 Intervention (HIIT vs. Slow breathing vs. Normal breathing) design. The detailed information is provided as supplementary materials.
Initially, we recruited a total of 128 participants based on the inclusion criteria: 1) biological sex at birth male; 2) only sexually attracted to women; 3) sexual identity heterosexual; 4) a stable female sexual partner with whom they had penile-vaginal sex at least once a week and exclusion criteria: 1) current substance abuse involving alcohol or drugs; 2) the use of Selective Serotonin Reuptake Inhibitor medications (such as fluoxetine, and paroxetine); 3) or the use of medication to delay ejaculation (e.g., dapoxetine); 4) a history of cardiovascular or endocrine diseases; 5) a history of significant medical, psychiatric, or neurological disorders. Seventy-six participants aged from 18 to 34 (M = 21.89, SD = 3.32), were randomly allocated to one of the three groups: 26 individuals to the HIIT group, 25 participants to the slow breathing group, and an additional 25 participants to the normal breathing group, all of whom completed the whole experiment. The detailed information for the excluded participants is provided as supplementary materials.
MeasuresDemographic informationParticipants reported first their age, height, weight, assigned sex at birth, sexual identity, and if they had a stable female sexual partner with whom they have had penile-vaginal sex at least once a week.
We calculated the body mass index (BMI) by dividing the weight in kilograms by the square of the participants' height in meters. Self-reported BMI has been demonstrated to be highly accurate (Chia et al., 2023).
Checklist for early ejaculation symptoms (CHEES)PE symptoms of participants were assessed using the CHEES score, a 5-item diagnostic tool refined for enhanced validity derived from three precursor ejaculation diagnostic instruments (Jern et al., 2013). Respondents rated items, such as “Over the past six months, was your control over ejaculation during sexual intercourse” on a 5-point Likert scale ranging from 1 (very good) to 5 (very poor). The cumulative score of the five items was computed to assess PE severity, with the present study reporting a Cronbach's α of 0.727. Higher values indicated more PE symptoms. In the present study, the male participants whose CHEES score was equal to or over 17 would be considered as men with PE.
To measure participants’ PE symptoms for the last two weeks before the intervention, we revised the time frame of the CHEES to create CHEES for the pre-intervention (CHEES-Pre). Cronbach's α was 0.815. The example item reported above was reformulated to “Over the past two weeks, was your control over ejaculation during sexual (penile-vaginal) intercourse”.
To measure participants’ PE symptoms for individual instances of penile-vaginal intercourse within the last day, we revised the time frame and formulations of the CHEES to create CHEES for Individual Sexual Events (CHEES-E). The example item reported above was reformulated to “Was your control over ejaculation during this penile-vaginal intercourse”. Cronbach's α was 0.958.
Physical activity questionnaireThe 5-item Physical Activity Questionnaire (Cho, 2016) was used to assess the participant's physical activity level in their free time. The items included the type of physical activity, frequency, duration, intensity, and overall length of time for the physical activities that participants engage in. The Cronbach's α was 0.671 in the present study. Higher values indicated individuals engaged in more physical activity in their free time.
HR measurementParticipants monitored their HR over 14 days, once before each intervention and five times after the intervention, at a rate of once per minute for 5 min. In addition, participants monitored their HR once immediately after penile-vaginal sex with their partner. The application information is provided as supplementary materials. The HR measurements were conducted by placing the forefinger on the rear smartphone camera, providing a user-friendly and accessible method for data acquisition. Evidence indicates that HR monitoring using a smartphone camera is accurate and reliable (Antoniou et al., 2023).
Attention regulationThe attention regulation subscale of the Multidimensional Assessment of Interoceptive Awareness scale was used (Mehling et al., 2012, 2018). The attention regulation subscale (e.g., I can maintain awareness of my inner bodily sensations even when there is a lot going on around me) assesses the ability to sustain and control attention to body sensations (Mehling et al., 2012). The subscale values for the response options ranged from 0 (never) to 5 (always). Higher subscale values indicated greater ability. The Cronbach's α was 0.871.
ProcedureFig. 1 shows the experimental procedure. The recruitment process is provided as supplementary material. Only men who met all the eligibility criteria could read the detailed description of the study at the end of the survey. After which, if they chose the option “Yes, I would like to participate”, they would provide their WeChat ID or email address and then complete the CHEES scale. Participants whose CHEES score was 17 or above, which is considered indicative of PE, were considered eligible for the experiment. Next, we contacted them via WeChat or email and scheduled the experiment.
After the participants read the consent form online and decided they agreed to participate in this study, they were randomly assigned to one of three groups: the HIIT group, the slow breathing group, and the normal breathing group, with complete random assignment using the R package “Randomizr” (Coppock, 2023). The detail information is provided as supplementary material.
The day before the intervention phase, participants were instructed to measure their HR once per minute for 3 min. Then, participants filled in a pre-intervention questionnaire including questions regarding demographic information, HR, PE symptoms for the last two weeks, attention regulation, and physical activity level in their free time.
During the intervention phase, participants completed a survey once every day after the intervention for two weeks. This survey included questions regarding HR before and after the intervention and any penile-vaginal sex after the intervention on the previous day. After the intervention, participants who, on the previous day, had engaged in penile-vaginal sex with their female partner would assess their PE symptoms, and attention regulation for this sexual event, and report their HR after sex.
In the HIIT intervention group, participants engaged in a 7-minute HIIT exercise guided by an instructional video every day between 6 a.m. and 9 a.m. or between 6 p.m. and 9 p.m. from day 1 to day 14. We used the instructional video created by Ego360 for the LumoWell / LumoFit project (Lumowell, 2014). Participants recorded their exercise session via video to verify adherence to the guided video. Participants were also instructed to declare the date of the exercise at the commencement of each video recording. These videos were transmitted to the researchers for confirmation, with a prompt deletion immediately upon verification of compliance. The exercises in the video had two versions: A normal level and a lower level. Participants chose which level to do based on their fitness level. In addition, participants were instructed to do the training with sufficient effort, more specifically, with enough exertion that their HR increased by 26 bpm from resting to after the HIIT intervention. Participants received feedback on whether their HR increased sufficiently. If not, participants were instructed to increase the effort the next day.
In the slow breathing and normal breathing intervention groups, the participants engaged in a 7-minute slow breathing or normal breathing training, respectively, following an instructional video that guided participants to breathe 5 times per minute (Maher, 2020) or 15 times per minute, respectively. Participants were instructed to breathe in for four seconds through the nose and breathe out for eight seconds through the mouth or breathe in for two seconds through the nose and breathe out for two seconds through the mouth. The other processes were the same as in the HIIT intervention group.
Finally, each participant was compensated 300 RMB (45 USD) in total for completing the experiment. The New York University Shanghai Institutional Review Board reviewed and approved the present study following the ethical standards as laid down in the 1964 Declaration of Helsinki.
Statistical analysesShort form data fileWe used SPSS v. 26.0 to conduct the data analyses. The detail information for the short form data file is provided as supplementary material.
Previous studies indicated that age (Niu, Ventus et al., 2023), BMI (Niu, Liu et al., 2023), and physical activity (Niu, Wen et al., 2023; Ventus & Jern, 2016; Yildiz et al., 2018) are associated with PE symptoms. Therefore, we conducted the ANOVA analyses both with and without these covariates.
First, we performed a one-way ANOVAs to investigate differences in age, BMI, physical activity, and CHEES-Pre pre-intervention among the intervention groups (HIIT vs. Slow breathing vs. Normal breathing) to verify successful random allocation.
Then, we performed bivariate correlations to investigate the associations between age, BMI, physical activity, attention regulation, and CHEES-Pre pre-intervention.
Next, we conducted two 2 Time (Day 1 vs. Day 14) × 3 Intervention (HIIT vs. Slow breathing vs. Normal breathing) mixed ANOVA to explore the differences in PE symptoms and attention regulation score between pre and post-intervention in the three intervention groups separately. To explore during the 14 days, any intervention effects would be noticeable, we also conducted two 14 Day (1 to 14) × 3 Intervention (HIIT vs. Slow breathing vs. Normal breathing) mixed ANOVA to explore the variation in PE symptoms and attention regulation score over the 14 intervention days with planned comparisons between the groups on each day separately.
We conducted a 2 Time (Day 1 vs. Day 14) × 3 Intervention (HIIT vs. Slow breathing vs. Normal breathing) mixed ANOVA to explore the differences in HR before the intervention and the first HR after the intervention to verify successful HIIT intervention work.
We also conducted a 2 Time (Day 1 vs. Day 14) repeated measures ANOVA analysis to investigate whether the HR recovery index increased after the HIIT intervention. Follow-up post-hoc comparisons at each time point were conducted after each ANOVA.
Long form data file with daily measurementFig. 2 shows the HR measurement and HR variables during the daily experiment task. The detail information for the long form data file is provided as supplementary material.
Heart rate measurement and related outcomes.
Note. Delta “△” 1 = Heart rate increase from resting to after sex. Delta “△” 2 = Heart rate increase from resting to after the high-intensity interval training (HIIT) intervention. Delta “△” 3 = Heart rate recovery after the HIIT intervention.
We conducted linear mixed-effect models using the “lmerTest'' package (Kuznetsova et al., 2017) in RStudio 2023.6.2.561(Racine, 2012) to investigate the main effect of the intervention group on the CHEES-E, attention regulation, the HR increase from resting to after penile-vaginal sex, while controlling for the subject random effect also for the below analyses. In addition, we investigated the associations between CHEES-E, attention regulation, the HR increase from resting to after sex, and the intervention day among the three groups. Additionally, we investigated the association between the HR increase from resting to after the HIIT intervention, the HR recovery after the HIIT intervention, and the intervention day. Finally, we investigated the associations between attention regulation, the HR increase from resting to after sex, and CHEES-E among the three groups. Additionally, we investigated the association between HR recovery after the HIIT intervention, HR increase from resting to after the HIIT intervention, and CHEES-E.
ResultsPreliminary analysesTable 1 shows the descriptive statistics of age, BMI, physical activity level, attention regulation, and PE symptoms before the intervention in the intervention groups. Results of the one-way ANOVAs showed no significant difference between the intervention groups for age (F(2, 73) = 0.932, p = .398), BMI (F(2, 73) = 1.324, p = .272), physical activity level (F(2, 73) = 0.744, p = .479), attention regulation score (F(2, 73) = 1.342, p = .268), or CHEES-Pre score (F(2, 73) = 1.133, p = .328) before the intervention showing that the randomization had been successful. The result of sexual events is provided as supplementary material.
Descriptives for men with premature ejaculation in different groups before the intervention.
Note. HIIT = High-intensity interval training. CHEES-Pre = The Checklist for Early Ejaculation Symptoms for last two weeks. The higher values for CHEES suggest more premature ejaculation symptoms. Higher values of physical activity suggest individuals engaged in more physical activity in their free time. A higher attention regulation score indicated a better ability to sustain and control attention to body sensations.
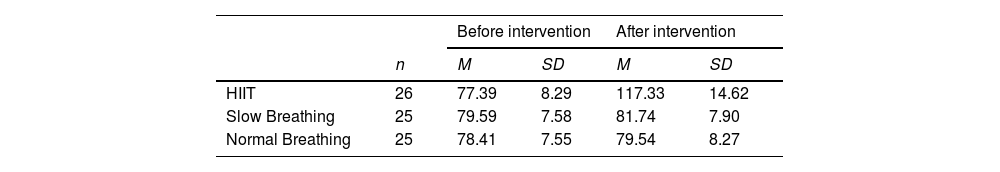
Table 2 shows the descriptive statistics for the average HR before and after interventions during the intervention. A 2 Time (Before vs. After intervention) × 3 Intervention (HIIT vs. Slow breathing vs. Normal breathing) a mixed ANOVA showed a significant interaction effect (F(2, 73) = 192.918, p < .001, partial η2 = 0.841). The main effects of Time (F(1, 74) = 242.441, p < .001, partial η2 = 0.769) and Intervention (F(2, 73) = 36.594, p < .001, partial η2 = 0.501) were also significant. The post hoc tests showed that there was no significant difference in HR before the intervention (F(1, 74) = 0.504, p < .606) between the intervention groups. The HR after the HIIT intervention was significantly higher than before the HIIT intervention (F(1, 74) = 637.525, p < .001, partial η2 = 0.897), while no significant difference was found in the slow breathing (F(1, 74) = 1.783, p = .186) or normal breathing groups (F(1, 74) = 0.492, p = .485). The average increase in the HIIT group was almost 40 bpm. These results show that the participants complied with the HIIT intervention.
Hypothesis testing (Short form data)Table 3 shows the relationship between age, BMI, physical activity level, attention regulation score and CHEES-Pre score before the intervention phase. The results indicated physical activity and attention regulation were not significantly associated with the CHEES-Pre score before the intervention phase, thus not supporting Hypotheses 1 and 2.
Correlations between Age, BMI, physical activity, attention regulation, and premature ejaculation before the intervention phase.
| Pre-intervention | Premature ejaculation (CHEES-Pre) | Age | BMI | Attention regulation |
|---|---|---|---|---|
| Age | −0.062 | |||
| BMI | −0.188 | .150 | ||
| Attention Regulation | .016 | −0.280* | −0.091 | |
| Physical Activity | −0.188 | −0.115 | .095 | .145 |
Note. CHEES-Pre = The Checklist for Early Ejaculation Symptoms for last two weeks. Higher values for CHEES suggest more premature ejaculation symptoms. Higher values for physical activity suggest individuals engaged in more physical activity in their free time. Higher attention regulation score indicated a better ability to sustain and control attention to body sensations. *p < .05.
The main effect of Time was significant both before (F(1, 74) = 38.903, p < .001, partial η2 = 0.348) and after (F(1, 74) = 12.462, p < .001, partial η2 = 0.151) controlling for covariates. The main effect of the Intervention was not significant either before (F(2, 73) = 2.138, p = .125) or after (F(2, 73) = 1.868, p = .162) controlling for covariates. The 2 Time (Day 1 vs. Day 14) × 3 Intervention (HIIT vs. Slow breathing vs. Normal breathing) mixed ANOVA showed no significant interaction effect before controlling for covariates (F(2, 73) = 2.817, p = .066). However, after controlling for covariates, the interaction was significant (F(2, 73) = 3.587, p = .033, partial η2 = 0.093). Post-intervention, the CHEES-E score in the HIIT group was significantly lower than in the normal breathing (F(1, 49) = 10.404, p = .002, partial η2 = 0.184) but not in the (F(1, 49) = 0.455, p = .504) slow breathing group. These results partially supported Hypotheses 3a and 3b.
Table 4 shows the change in the CHEES-E score in the intervention groups over the 14-day intervention. The 14 Day (1 to 14) × 3 Intervention (HIIT vs. Slow breathing vs. Normal breathing) mixed ANOVA showed that Mauchly's Test of Sphericity was significant. The main effect of Day was significant both before (F(13, 62) = 20.421, p < .001, partial η2 = 0.219) and after (F(13, 62) = 9.244, p < .001, partial η2 = 0.117) controlling for covariates. The main effect of Intervention was not significant either before (F(2, 73) = 0.956, p = .389) or after (F(2, 73) = 0.922, p = .402) controlling for covariates. The result showed no significant interaction effect before controlling for the covariates (F(26, 49) = 1.794, Sphericity Assumed p = .009, Greenhouse-Geisser p = .114, Huynh-Feldt p = .109, partial η2 = 0.047). However, after controlling for covariates, the interaction was significant (F(26, 49) = 2.118, Sphericity Assumed p < .001, Greenhouse-Geisser p = .058, Huynh-Feldt p = .05, partial η2 = 0.057). Post hoc tests indicated that CHEES-E score in the HIIT group on Day 12 (F(1, 49) = 5.305, p = .026, partial η2 = 0.103), Day 13 (F(1, 49) = 6.598, p = .014, partial η2 = 0.125) and Day 14 (F(1, 49) = 10.404, p = .002, partial η2 = 0.184) was significantly lower than in the normal breathing group (See Fig. 3). These results partially supported Hypotheses 3a and 3b given that the results were clearly in line with the expectations only when the covariates were included in the analyses.
Descriptives of premature ejaculation symptoms in the intervention groups over the 14-day intervention.
Note. HIIT = High-intensity interval training intervention. CHEES-E = The Checklist for Early Ejaculation Symptoms for the individual sexual events. Higher values of CHEES suggest more premature ejaculation symptoms. Different superscripts indicate premature ejaculation symptoms differed significantly from each other.
Differences in premature ejaculation symptoms between the intervention groups over the 14-day intervention.
Note. HIIT = High-intensity interval training intervention. CHEES-E = The Checklist for Early Ejaculation Symptoms for the individual sexual events. Higher values of CHEES suggest more premature ejaculation symptoms.
A 2 Time (Day 1 vs. Day 14) × 3 Intervention (HIIT vs. Slow breathing vs. Normal breathing) mixed ANOVA showed a significant main effect of Time (F(1, 74) = 94, p < .001, partial η2 = 0.563), no significant main effect of Intervention (F(2, 73) = 0.968, p = .385) and no significant interaction effect (F(2, 73) = 0.268, p = .766) for attention regulation. Next, we looked at the effect of Time (Day 1 vs. Day 14) separately in the three groups. The results showed that compared to the value on Day 1, attention regulation score on Day 14 had increased in the HIIT (F(1, 74) = 32.866, p < .001, partial η2 = 0.342), slow breathing (F(1, 74) = 34.673, p < .001, partial η2 = 0.303) and normal breathing groups (F(1, 74) = 27.181, p < .001, partial η2 = 0.256).
Table 5 shows the variation in the attention regulation score in the different intervention groups during the 14-day intervention. A 14 Day (1 to 14) × 3 Intervention (HIIT vs. Slow breathing vs. Normal breathing) mixed ANOVAs showed a significant main effect of Day (F(13, 62) = 7.020, p < .001, partial η2 = 0.599), no significant main effect of the Intervention (F(2, 73) = 0.903, p = .410) and no significant interaction effect (F(26, 49) = 0.825, p = .708). These results show that attention regulation improved in all three groups; this result fails to support Hypotheses 4a and 4b.
Description of the attention regulation score in the intervention groups over the 14-day intervention.
Note. HIIT = High-intensity interval training intervention. A higher attention regulation score indicates a better ability to sustain and control attention to body sensations.
The main effect of the Intervention on the CHEES-E score was not significant (F(2, 73) = 2.181, p = .120).
Importantly, the results indicated that the CHEES-E score decreased over the intervention across all three groups (B = −0.200, SE = 0.050, t = −4.019, p < .001). This decrease was significant in the HIIT group (B = −0.275, SE = 0.094, t = −2.938, p = .006), as expected, but also in the normal breathing group (B = −0.196, SE = 0.082, t = −2.409, p = .022), which was unexpected, but not in the slow breathing group (B = −0.086, SE = 0.075, t = −1.149, p = .261).
The main effect of the Intervention on the attention regulation score was not significant (F(2, 73) = 1.115, p = .334).
However, the results indicated that the attention regulation score increased over the intervention (B = 0.035, SE = 0.010, t = 3.581, p < .001) among the three groups. Attention regulation increased over the intervention in the HIIT (B = 0.027, SE = 0.014, t = 1.945, p = .059) group, as expected, and normal breathing group (B = 0.059, SE = 0.019, t = 3.086, p = .004), which was unexpected, but not in the slow breathing group (B = 0.025, SE = 0.019, t = 1.367, p = .184). These results did not support Hypothesis 5a.
We also found, as expected, that a better attention regulation score was associated with a lower CHEES-E score (B = −0.993, SE = 0.348, t = −2.854, p = .005) across the three groups. Further, the association between a higher attention regulation score and a lower CHEES-E score was significant in the HIIT (B = −1.901, SE = 0.707, t = −2.687, p = .011) and normal breathing groups (B = −0.973, SE = 0.459, t = −2.12, p = .041), but no association was found in the slow breathing group (B = −0.411, SE = 0.603, t = −0.682, p = .499). These results only partly support Hypothesis 6a.
The main effect of the Intervention on the HR increase from resting to after sex was not significant (F(2, 73) = 1.262, p = .291).
The HR increase from resting to after sex increased over the intervention (B = 0.688, SE = 0.314, t = 2.189, p = .031) among the three groups. The effect was significant in the normal breathing group (B = 1.268, SE = 0.522, t = 2.43, p = .021), but not in the HIIT (B = 0.756, SE = 0.568, t = 1.331, p = .192) or slow breathing (B = 0.043, SE = 0.498, t = 0.087 p = .932) groups. These results did not support Hypothesis 5b.
Overall, we found no significant association between HR increase from resting to after sex and CHEES-E score (B = −0.022, SE = 0.012, t = −1.828, p = .070) even though the association was in the expected direction. Separately, in the HIIT group, the results showed that the greater HR increase from resting to after sex was associated with a lower CHEES-E score (B = −0.042, SE = 0.02, t = −2.077, p = .043). This was not the case in the slow breathing (B = 0.003, SE = 0.02, t = 0.172, p = .865) or normal breathing (B = −0.017, SE = 0.022, t = −0.772, p = .444) groups. This result did not fully support Hypothesis 6b.
In the HIIT group, the HR increase from resting to after HIIT significantly increased over the intervention (B = 0.571, SE = 0.050, t = 11.540, p < .001). This result supports Hypothesis 5c. However, there was no significant association between HR increase from resting to after HIIT and CHEES-E score (B = 0.016, SE = 0.023, t = 0.676, p = .502). This result did not support Hypothesis 6c.
In the HIIT group, HR recovery did not significantly increase over the intervention (B = 0.123, SE = 0.199, t = 0.619, p = .536). However, there was a tendency for HR recovery after the HIIT intervention and the CHEES-E score to be associated as expected (B = 0.055, SE = 0.03, t = 1.851, p = .07). The result did not support Hypothesis 5d or 6d.
DiscussionWe explored the effectiveness of a two-week intervention involving a 7-minute HIIT or slow and normal breathing training on alleviating PE symptoms in men with PE. We found a significant Time × Intervention interaction, as expected, showing that PE symptoms after the HIIT intervention were fewer than those under the normal breathing intervention (Hypothesis 3a). We also demonstrated that the PE symptoms decreased more while engaging in the HIIT intervention than the normal breathing intervention over the intervention period (Hypothesis 3b). Importantly, after the HIIT and slow breathing interventions, the CHEES-E score decreased to approximately 15, indicating a low probability of PE on the 14th day. However, this was not observed in the normal breathing intervention group. Overall, the HIIT intervention was more effective than the control (normal breathing) intervention in alleviating PE symptoms. We did not find the expected significant Time × Intervention interaction only showing attention regulation in the HIIT and slow breathing groups (Hypotheses 4a & 4b). Instead, attention regulation also improved in the normal breathing control group. However, we found the HIIT and slow breathing interventions to be effective in enhancing attention regulation during the intervention (Hypothesis 5a) as in some previous studies (Rominger et al., 2021; Wallman-Jones et al., 2022).
Unsurprisingly, the HIIT intervention improved attention regulation, a key element of interoceptive awareness (Mehling et al., 2012). During the HIIT intervention, participants not only need to pay attention to making the body move to complete the exercises but also regulate their breathing. After repeated practice, their ability to regulate the attention to the internal and external body sensations may improve. The mechanism of enhanced attention regulation would be the potential roles of the sympathetic and parasympathetic nervous systems on the neural circuit of interoception (Berntson & Khalsa, 2021; Craig, 2002). Previous studies found that HIIT intervention can improve the sympathovagal balance (Alansare et al., 2018; Besnier et al., 2019; Ito, 2019) leading to more effective neural signal transmission from the brain to the body or from the body to brain during the interoception generation (Berntson & Khalsa, 2021; Craig, 2002). Because the afferent and efferent pathways of interoception improve, interoceptive awareness including attention regulation may improve. However, we also found that the normal breathing intervention improved attention regulation. Participants who engaged in slow breathing and normal breathing interventions were instructed to direct their attention to breathing during the breathing intervention in the daily questionnaire. This may have improved attention regulation in all groups. Alternatively, both breathing interventions involved following the instruction video that directed the participants to pay attention to the sensation of the breath and to bring their breath rhythm to a conscious level, especially for the movement of inspiratory and expiratory muscles. Thereby participants practiced regulating attention to internal signals and perceiving the internal and external signs and made related responses to follow the breath rhythm which subsequently enhanced the participants’ ability to regulate the attention.
Notably, there was a robust association between attention regulation during sex and fewer PE symptoms (Hypothesis 6a). This suggests that individuals with better attention regulation would have an improved ability to perceive the bodily sensations associated with increased sexual stimulation during sexual intercourse, especially when sexual arousal is close to the orgasm threshold. This means that the individuals would be able to regulate sexual stimulation intensity and also translate the attention from sexual stimulation to other body sensations which in turn would decrease sexual excitability which may lead to better ejaculation control. In addition, individuals with better attention regulation have been found to have a greater ability to reduce anxiety (Derryberry & Reed, 2002) which would lead to an improved sympathovagal balance (Chalmers et al., 2014; Goessl et al., 2017; Rowland & van Lankveld, 2019) and this may play a role in the etiology of PE (Erbay & Ceyhun, 2021). Considering that PE symptoms decreased over the intervention, this suggested that attention regulation may play a potential role in the improvement of ejaculation control. While we did not expect any improvements in the control condition (normal breathing), however, given that they had an instruction to pay attention to their breathing, there may have been an impact on attention regulation.
In the HIIT group, HR from resting to after the HIIT intervention during the intervention increased (Hypothesis 5b). However, HR increase from resting to after HIIT and the PE symptoms were unrelated (Hypothesis 6b). Previously, a greater HR increase during a HIIT intervention was associated with fewer PE symptoms (Niu, Wen et al., 2023). There may be a ceiling effect in the HR increase from resting to after HIIT in the present study. The average HR increase from resting to after HIIT was almost 40 bpm which was higher than the medium HR increase of 26 bpm in the previous study (Niu, Wen et al., 2023). Previously, participants with at least a 26 bpm increase from resting to after the HIIT intervention have more reduction in the PE symptoms compared to before the intervention (Niu, Wen et al., 2023).
However, during a two-week HIIT intervention, this study did not find a significant improvement in HR recovery (Hypothesis 5c). In addition, the study did not find a robust association between a greater HR recovery and more PE symptoms (Hypothesis 6c).
We found some indication that the HR from resting to after sex increased during the intervention (Hypothesis 5d). More importantly, the greater HR increase from resting to after sex was associated with fewer PE symptoms (Hypothesis 6d). This might suggest that individuals with better ejaculation control would more likely engage in more physically demanding penile-vaginal sex (e.g., more demanding positions). More physical activity during sex could trigger a higher level of sympathetic activity which would lead to the HR increase.
Surprisingly, the study did not find an association between pre-intervention physical activity level (Hypothesis 1) and attention regulation (Hypothesis 2) and PE symptoms.
Compared with the other physical exercise treatments, the two weeks of the HIIT treatment would be more time-effective than the ten weeks of yoga (Rohilla et al., 2020) and 30 days of running (Kilinc et al., 2018). Compared with the medical treatment, for example, ten weeks of paroxetine (Rohilla et al., 2020), the HIIT treatment also would be more time-effective. Therefore, the HIIT treatment may be a time-effective treatment for PE without side effects.
Limitations and future directionsThe sample population in this study was relatively young limiting generalizability. Also, some participants’ highest HR value may occur during the HIIT intervention. In the present study, we only measured the HR after the HIIT intervention. Further studies could also measure the HR variation during and after the physical exercise. Finally, participants monitored their HR using the smartphone app that collected the physical signs via the rear smartphone camera. However, the reliability of the method may be limited. Lastly, Cronbach's α of the Physical Activity Questionnaire was lower than 0.70. The reason for this result may be that only two participants performed two or three types of physical activity. Therefore, there were missing values for the other 12 items for other participants who only performed one type of physical activity (5 items).
ConclusionCompared to the control group, the efficacy of two weeks of HIIT exercise in mitigating PE symptoms suggests its potential as a novel treatment for PE. The association between the increase in attention regulation and reduction in PE symptoms suggesting its significant role in the etiology of PE.
Funding informationThe original data collections were partly funded by an individual grant from New York University Shanghai. This work was funded by a state scholarship fund from the China Scholarship Council (No. 202306140145).
CRediT authorship contribution statementCaoyuan Niu: Investigation, Data curation, Methodology, Formal analysis, Writing – original draft, Visualization. Guangju Wen: Formal analysis. Daniel Ventus: Formal analysis, Writing – review & editing. Patrick Jern: Formal analysis, Writing – review & editing. Thomas J. Nyman: Writing – review & editing. Yansong Li: Writing – review & editing. Pekka Santtila: Conceptualization, Supervision, Writing – review & editing.