After an acquired brain injury (ABI), the person remains with several impairments and disabilities that cause a decrease in his/her quality of life (QoL), which could change over time. The objective of the study was to analyse the evolution patterns of QoL in a sample of persons with ABI for one-year as well as the differences in proxy- and self-report versions of a QoL instrument. Method: The sample comprised 402 persons with ABI with ages ranging between 18 and 91 years, whom 36.20% had had the accident recently (i.e., three years or less). Patients, professionals and relatives responded at three evaluation points to the CAVIDACE scale, an ABI-specific QoL tool. Results: ANOVAs showed an improvement in QoL in the two follow-ups; the improvement was especially significant in the period between baseline and six months. The respondent factor did not interact with the evaluation time, but significant differences were found between respondents, with scores of patients higher than that for proxies. Finally, the QoL’s evolution interacts with the time elapsed since injury, showing significant improvements in the most recent group (i.e., three years or less). Conclusions: QoL must be considered from the earliest moments after ABI to obtain more significant improvements.
Después del daño cerebral adquirido (DCA), la persona permanece con secuelas y discapacidades severas que pueden causar una disminución de su calidad de vida (CV) variable a lo largo del tiempo. El objetivo de este estudio es analizar los cambios en la CV a lo largo de un año, así como las diferencias entre las versiones autoinforme y heteroinforme de un instrumento de CV. Método: La muestra estuvo compuesta por 402 personas con DCA, con edades entre 18 y 91 años, de quiénes el 36,20% había tenido el accidente recientemente (tres años o menos). Pacientes, profesionales y familiares respondieron en los tres momentos de evaluación a la escala CAVIDACE, un instrumento específico para DCA. Resultados: Los ANOVAs mostraron una mejoría en muchas de las dimensiones de CV en ambos seguimientos, especialmente significativa entre la línea base y los seis meses. Los pacientes puntuaron más alto que el resto de evaluadores, pero este factor no mostró interacción con el momento de evaluación. Finalmente, la evolución de la CV interactuó con el tiempo transcurrido desde el DCA, encontrándose mejorías en el grupo con menor recorrido. Conclusiones: La CV debe ser tenida en cuenta desde los primeros momentos tras el DCA para obtener mejorías más significativas.
Acquired brain injury (ABI) is a leading cause of death and disability in the world (Nichol et al., 2011). In Spain, there is a prevalence of 420,064 people with ABI and approximately 104,701 new cases per year (Quezada et al., 2015). Although it is increasingly possible to save more lives because of advances in medicine, the percentage of people left with impairments after the ABI is very high, even with mild injuries (Chiang et al., 2015; Haagsma et al., 2015). Individuals who have sustained an ABI often experience physical and emotional problems (Haagsma et al., 2015; Lin et al., 2010; Yeoh et al., 2019), cognitive deficits (Grauwmeijer et al., 2018; Yeoh et al., 2019) and behavioural and social alterations (Azouvi et al., 2016; Lin et al., 2010). Some of these impairments may have a prolonged progression time that lead to chronic health problems (Azouvi et al., 2016; Grauwmeijer et al., 2018), which negatively impact the quality of life (QoL) (Andelic et al., 2009; Forslund et al., 2013; Pagnini et al., 2019; Yeoh et al., 2019).
Traditionally, QoL has been studied through generic instruments conceptualized from a health-related QoL approach (HRQoL), such as the SF-36 (Ware & Sherbourne, 1992). HRQoL focused on very specific domains of the person’s QoL, mainly related to health and physical well-being. In recent years, a specific instrument for ABI has been developed: the QOLIBRI scale (von Steinbüchel et al., 2010), which allows a more specific and comprehensive QoL evaluation. However, it continued to be sheltered by the HRQoL model, excluding important QoL areas such as self-determination, material well-being or personal development. In addition, this instrument has been used only in populations with traumatic brain injury (TBI), while its use in other ABI aetiologies (stroke, brain anoxia, brain tumour or cerebral infection) has been ignored.
In 2018, a specific-ABI QoL instrument was developed and validated, based on a comprehensive model that considers a psychosocial approach that goes beyond aspects merely related to health, and that can be used in the entire ABI population: the CAVIDACE scale (Fernández et al., 2019). This instrument is based on Schalock and Verdugo’s QoL model, which has been widely used in other populations, such as intellectual and developmental disabilities (Schalock & Verdugo, 2002) and the elderly (Vanleerberghe et al., 2017). According to the model (Schalock et al., 2018), QoL is a multidimensional phenomenon that reflects the well-being desired by the person in relation to eight basic needs: emotional well-being (EW), interpersonal relations (IR), material well-being (MW), personal development (PD), physical well-being (PW), self-determination (SD), social inclusion (SI) and rights (RI). Moreover, this core domain shows intergroup stability and sensitivity to personal perceptions, including subjective and objective aspects, and are influenced by environmental and personal factors and their interaction (Schalock et al., 2016, 2018).
QoL has been considered a subjective construct that should be evaluated through self-report. However, in many cases of people with ABI, this is not possible due to the severity of the impairments (e.g., consciousness alterations) or the inability to communicate (e.g., global aphasia). Furthermore, the validity of the self-reports has been questioned because of the frequent presence of memory alterations and anosognosia in this population (Formisano et al., 2017; Grauwmeijer et al., 2018). Therefore, in some cases, it is necessary to use QoL instruments that can be answered by a relative or professional who knows the person (Kozlowski et al., 2015). However, there are very few studies that have analysed the discrepancies depending on the assessment approach (Verdugo et al., 2005) and how they have evolved over time. The existing studies show discordant results, with some showing an overestimation of the QoL by the ABI person when compared to their relatives’ evaluation (Formisano et al., 2017; Hwang et al., 2017; Kozlowski et al., 2015) and others showing high correlations between the results found (Câmara-Costa et al., 2020).
QoL after ABI is not stable over time. Most of the studies refer to a period of time around one (Chiang et al., 2015; Haller et al., 2017; Pucciarelli et al., 2019; Yeoh et al., 2019) or two years after ABI (Hu et al., 2012; Zhang et al., 2013), in which the QoL can improve and then achieve stability (Andelic et al., 2018; Forslund et al., 2013; Grauwmeijer et al., 2018), but generally staying lower than in the normative population (Forslund et al., 2013; Hu et al., 2012; Yeoh et al., 2019; Zhang et al., 2013). On the other hand, there are studies which show late recovery patterns three and four years after ABI (Gould & Ponsford, 2015), while others have shown evidence that the QoL worsens from the beginning (Schindel et al., 2019). The use of different instruments, aetiologies and research designs could explain this lack of agreement. However, they distinguish different evaluation patterns in QoL levels, and these patterns depend on multiple factors such as age, gender or severity of the injury (Scholten et al., 2015). Furthermore, the QoL evolution is not uniform between the different domains, with higher rates of improvement in the physical aspects than in the emotional (Haller et al., 2017; Scholten et al., 2015) and social areas (Chuluunbaatar et al., 2016; Lin et al., 2010; Pucciarelli et al., 2019).
In summary, longitudinal QoL studies in ABI have typically reported an initial period of improvement followed by later stabilization. However, we do not have comparative data on this evolution depending on whether self- or proxy-report instrument are used, or taking into account QoL’s domains that go beyond a HRQoL model. This manuscript aimed to contribute to the current literature by: (1) describing the patterns of evolution of the eight-QoL domains over a one-year follow-up in a sample of Spanish adults with ABI; (2) determining whether there are differences when the QoL assessment is carried out by a relative, professional or by the person with ABI; and (3) examining whether these evolution patterns depend on the time elapsed since the injury, considering recent (i.e., three years or less) or chronic ABI.
MethodDesignThis is a quantitative longitudinal study. Participating organizations providing attention to ABI population were primarily recruited through emails and telephone calls by the research team. Once a centre expressed interest in participating in the study, a research team member visited it and provided them all the necessary information. In each centre, a research assistant was trained to oversee the administration of the CAVIDACE scale in professionals, families and patients (T1). The research team provided the printed copies, but they also had the possibility to complete the scales online.
A follow-up was then carried out at 6 (T2) and 12 months (T3), again with the application of the QoL instrument to professionals, families, and patients. Demographic and clinical information was collected only at baseline. In the baseline, there were a total of 402 participants. However, at 6 and 12 months of follow-up, only 270 and 200 participants (respectively) were maintained. The causes of sample loss of 31% and 49% were end of rehabilitation, death of patient or refusal to continue in the study.
This study was approved by the Bioethics Committee of the University of Salamanca (No: 20189990014185/ Record: 2018/REGSAL-1931). Written informed consent was obtained from both participants with ABI and their relatives. Personal and clinical data were collected, stored and protected in accordance with the Organic Law 3/2018 of December 5 on Data Protection and Guarantee of Digital Rights.
ParticipantsParticipants were recruited following a non-probabilistic convenience sampling process. ABI participants had to meet the following inclusion criteria: (a) have an ABI; (b) are 16 years or older; (c) are treated in a specific centre; and (d) sign informed consent. The ABI sample was composed of 402 adults from 27 rehabilitation centres providing health and social services throughout Spain.
Professionals, families and patients responded to a QoL measure. For inclusion in the study, professionals and families had to know the person with ABI for at least 3 months and in different contexts. A professional responded to the QoL measure in all cases and in most cases (N = 343) also a family member. The inclusion criterion of ABIs was the ability to understand and respond to the scale, determined by the clinical judgement of professionals. The exclusion criteria were as follows: (a) are in a state of coma or minimum consciousness; and (b) have a global aphasia. Three hundred fifty-four of 402 participants were able to respond to the self-report instrument.
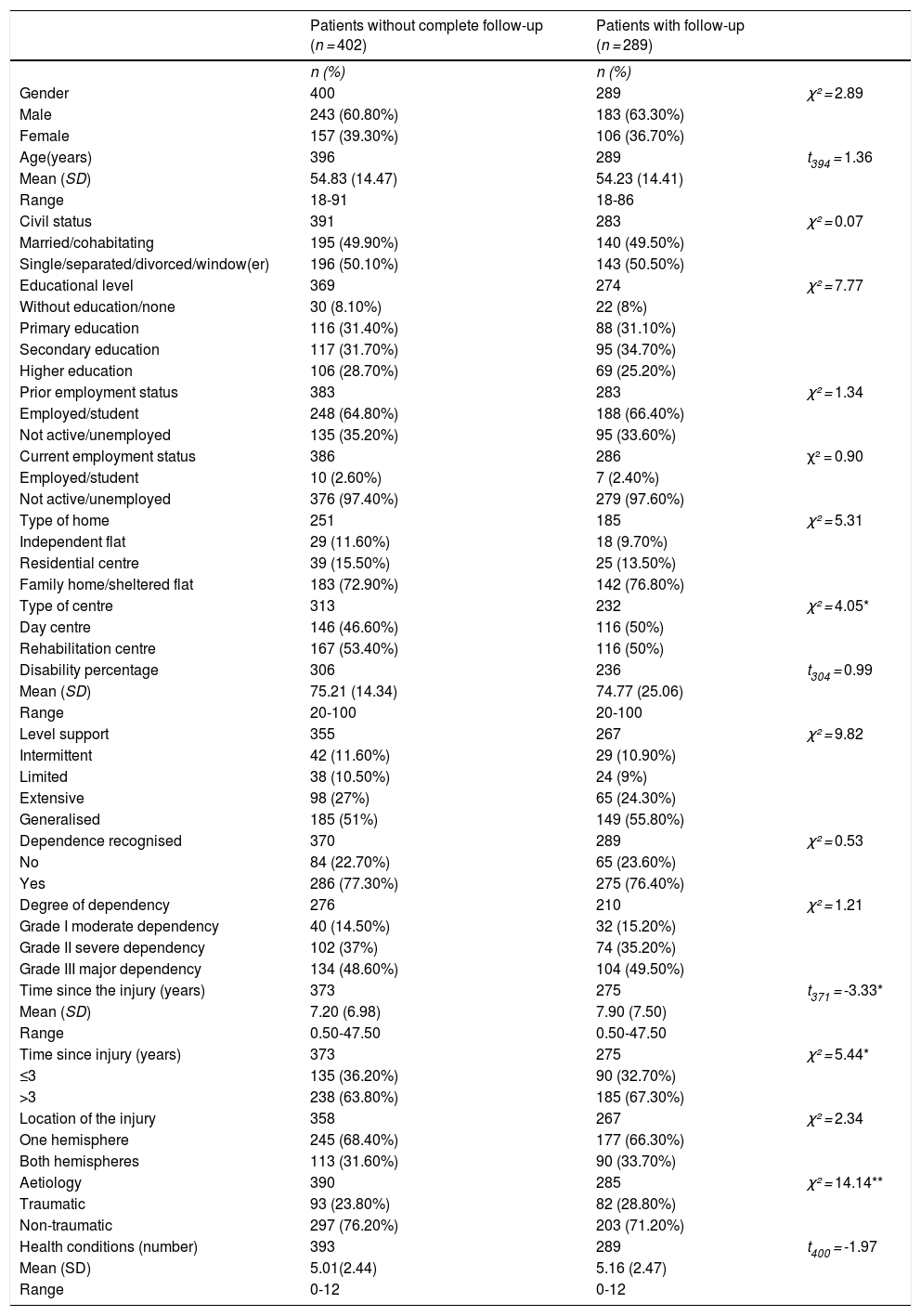
More than half of the sample was male (60.80%), with ages between 18 and 91 years (M = 54.83; SD = 14.47). There was a low percentage of subjects who returned to work or study after ABI (2.60%) and living independently (11.60%). Stroke was the main aetiology of the injury (60.90%), and the average time since injury was 7.20 years (SD = 6.98; range 0.50-47.50). When comparing the differences between patients with and without follow-ups, significant differences were found in (Table 1 for in-depth information): time since injury (t371 = -3.33, p = .001), type of centre (χ² = 4.05, p = .04) and aetiology (χ² = 14.14, p < .001). People for whom follow-up evaluations were not available had the ABI less time ago, went more to rehabilitation centres than to day centres, and had a higher prevalence of stroke.
Participant’s sociodemographic and clinical characteristics.
| Patients without complete follow-up (n = 402) | Patients with follow-up (n = 289) | ||
|---|---|---|---|
| n (%) | n (%) | ||
| Gender | 400 | 289 | χ² = 2.89 |
| Male | 243 (60.80%) | 183 (63.30%) | |
| Female | 157 (39.30%) | 106 (36.70%) | |
| Age(years) | 396 | 289 | t394 = 1.36 |
| Mean (SD) | 54.83 (14.47) | 54.23 (14.41) | |
| Range | 18-91 | 18-86 | |
| Civil status | 391 | 283 | χ² = 0.07 |
| Married/cohabitating | 195 (49.90%) | 140 (49.50%) | |
| Single/separated/divorced/window(er) | 196 (50.10%) | 143 (50.50%) | |
| Educational level | 369 | 274 | χ² = 7.77 |
| Without education/none | 30 (8.10%) | 22 (8%) | |
| Primary education | 116 (31.40%) | 88 (31.10%) | |
| Secondary education | 117 (31.70%) | 95 (34.70%) | |
| Higher education | 106 (28.70%) | 69 (25.20%) | |
| Prior employment status | 383 | 283 | χ² = 1.34 |
| Employed/student | 248 (64.80%) | 188 (66.40%) | |
| Not active/unemployed | 135 (35.20%) | 95 (33.60%) | |
| Current employment status | 386 | 286 | χ² = 0.90 |
| Employed/student | 10 (2.60%) | 7 (2.40%) | |
| Not active/unemployed | 376 (97.40%) | 279 (97.60%) | |
| Type of home | 251 | 185 | χ² = 5.31 |
| Independent flat | 29 (11.60%) | 18 (9.70%) | |
| Residential centre | 39 (15.50%) | 25 (13.50%) | |
| Family home/sheltered flat | 183 (72.90%) | 142 (76.80%) | |
| Type of centre | 313 | 232 | χ² = 4.05* |
| Day centre | 146 (46.60%) | 116 (50%) | |
| Rehabilitation centre | 167 (53.40%) | 116 (50%) | |
| Disability percentage | 306 | 236 | t304 = 0.99 |
| Mean (SD) | 75.21 (14.34) | 74.77 (25.06) | |
| Range | 20-100 | 20-100 | |
| Level support | 355 | 267 | χ² = 9.82 |
| Intermittent | 42 (11.60%) | 29 (10.90%) | |
| Limited | 38 (10.50%) | 24 (9%) | |
| Extensive | 98 (27%) | 65 (24.30%) | |
| Generalised | 185 (51%) | 149 (55.80%) | |
| Dependence recognised | 370 | 289 | χ² = 0.53 |
| No | 84 (22.70%) | 65 (23.60%) | |
| Yes | 286 (77.30%) | 275 (76.40%) | |
| Degree of dependency | 276 | 210 | χ² = 1.21 |
| Grade I moderate dependency | 40 (14.50%) | 32 (15.20%) | |
| Grade II severe dependency | 102 (37%) | 74 (35.20%) | |
| Grade III major dependency | 134 (48.60%) | 104 (49.50%) | |
| Time since the injury (years) | 373 | 275 | t371 = -3.33* |
| Mean (SD) | 7.20 (6.98) | 7.90 (7.50) | |
| Range | 0.50-47.50 | 0.50-47.50 | |
| Time since injury (years) | 373 | 275 | χ² = 5.44* |
| ≤3 | 135 (36.20%) | 90 (32.70%) | |
| >3 | 238 (63.80%) | 185 (67.30%) | |
| Location of the injury | 358 | 267 | χ² = 2.34 |
| One hemisphere | 245 (68.40%) | 177 (66.30%) | |
| Both hemispheres | 113 (31.60%) | 90 (33.70%) | |
| Aetiology | 390 | 285 | χ² = 14.14** |
| Traumatic | 93 (23.80%) | 82 (28.80%) | |
| Non-traumatic | 297 (76.20%) | 203 (71.20%) | |
| Health conditions (number) | 393 | 289 | t400 = -1.97 |
| Mean (SD) | 5.01(2.44) | 5.16 (2.47) | |
| Range | 0-12 | 0-12 |
Note. *p < .05, **p < .01
The proxy versions were administered to almost 500 informants (i.e., 147 professionals and 343 family members). The professionals (women: 79%) were primarily neuropsychologists (24%), occupational therapists (20%), and physiotherapists (19%). As for the family members, they were primarily partners (50%) and parents (28%); 68% distributed in the category women.
InstrumentThe QoL assessment was carried out through the administration of the CAVIDACE scale, an ABI disease-specific instrument based on an external observer (i.e., proxy measure) (Fernández et al., 2019). It consists of 64 items that assess the eight domains of Schalock and Verdugo’s QoL model (2002). Responses are recorded on a four-point frequency scale: 0 = never, 1 = sometimes, 2 = frequently and 3 = always. For its correction, direct scores obtained in each of the eight domains are transformed into standard scores (M = 10, SD = 3) and a raw QoL score (i.e., the sum of the standard scores), where higher scores indicate better QoL. This overall score may be converted into a QoL index (M = 100, SD = 15). It has demonstrated very good psychometric properties. Validity evidence based on the internal structure of the scale was provided through confirmatory factor analyses. Reliability was analysed in terms of internal consistency and inter-rater reliability. The results supported the internal structure of the scale, based on eight intercorrelated first-order domains (CFI = .890, RMSEA = .065, SRMR = .071). The internal consistency was good or excellent for the eight domains (ordinal alpha ranging from .77 to .93) and the inter-rater reliability was very high (ICC = .97) (Fernández et al., 2019).
The self-report version of the CAVIDACE Scale is an adaptation of the original scale, which is completed by individuals with ABI. It consists of 40 items, which also assess the eight domains of the model and uses the same frequency rating scale, index and scores (Aza et al., 2020). Its psychometric properties are comparable to those of the original scale: QoL is composed of eight first-order intercorrelated domains (RMSEA = .050, CFI = .891, TLI = .881). The internal consistency was adequate in seven of the eight domains (ω = .66–.87) and showed excellent indexes of convergent-divergent validity (Aza et al., 2020).
Statistical analysesSPSS version 24 was used for statistical analysis. Statistical significance was set at p= .05 with Bonferroni adjustment. Descriptive data of the sample are shown. Patients who completed two or more measurements were included in the analysis. When comparing characteristics between the included patients and those who were lost to follow-up, the categorical variables were analysed with chi-squared test and the continuous variables with independent t-test.
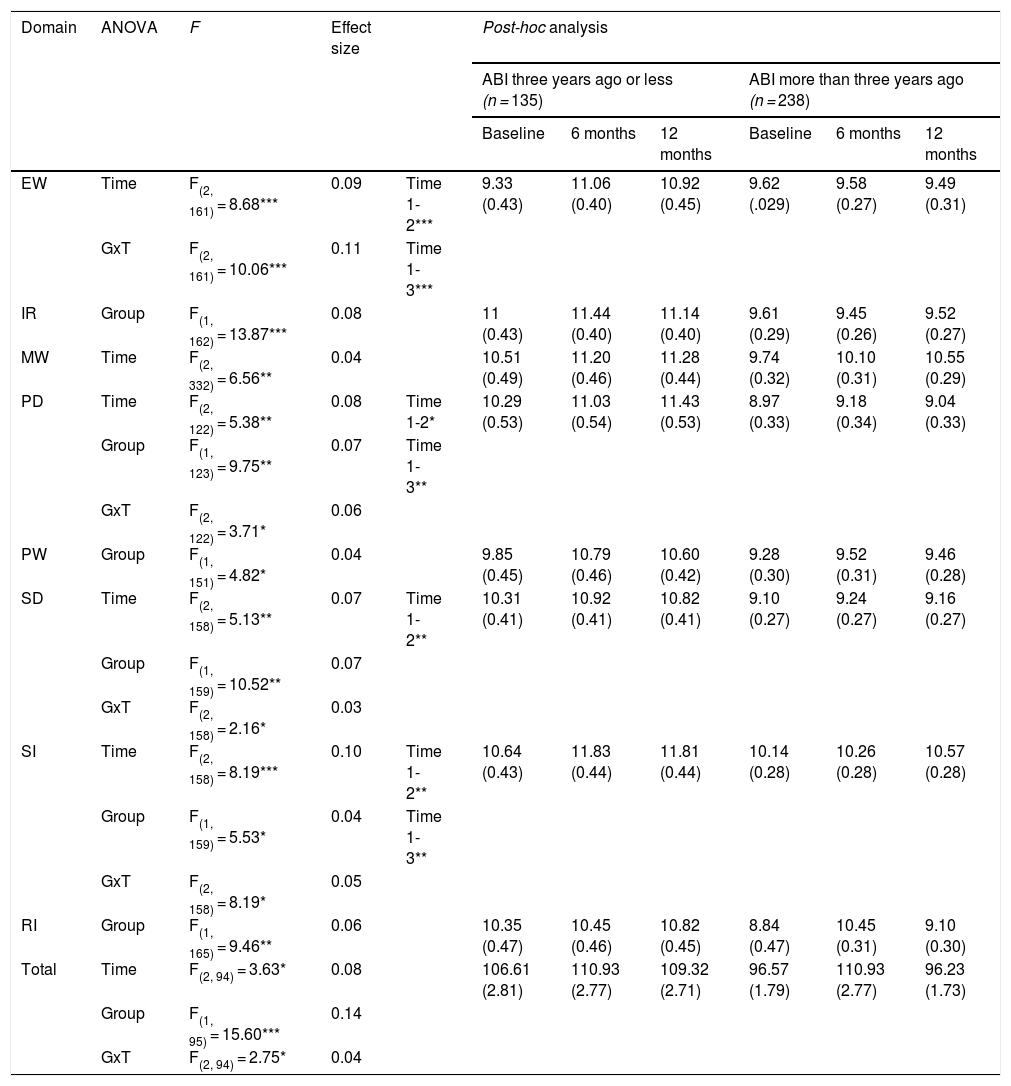
Second, the researchers calculated descriptive QoL’s values and conducted 3 × 3 analyses of variance (ANOVAs) for each domain (standard scores) and total score (QoL index) to determine the changes from baseline to 6 and 12 months of follow-up (within-subject factors) in the three respondents (within-subjects factor) as well as the interaction effect. Bar charts are presented. Post-hoc analyses and effect sizes were through eta-squared (η2) were calculated.
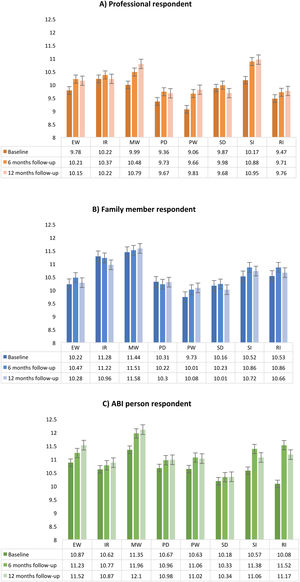
To determine whether QoL followed different patterns based on time elapsed since injury, patients were divided into those who had the accident three years ago or less and those who had it longer. Descriptive data were calculated, and the differences between baseline and follow-ups were assessed through mixed ANOVAs 2 × 3. We conducted the analyses only for the professional evaluation. Main effects of the within-subjects factors (evaluation time), between-subjects factors (time since injury) and interaction were calculated. Post-hoc analyses and η2 were also analysed.
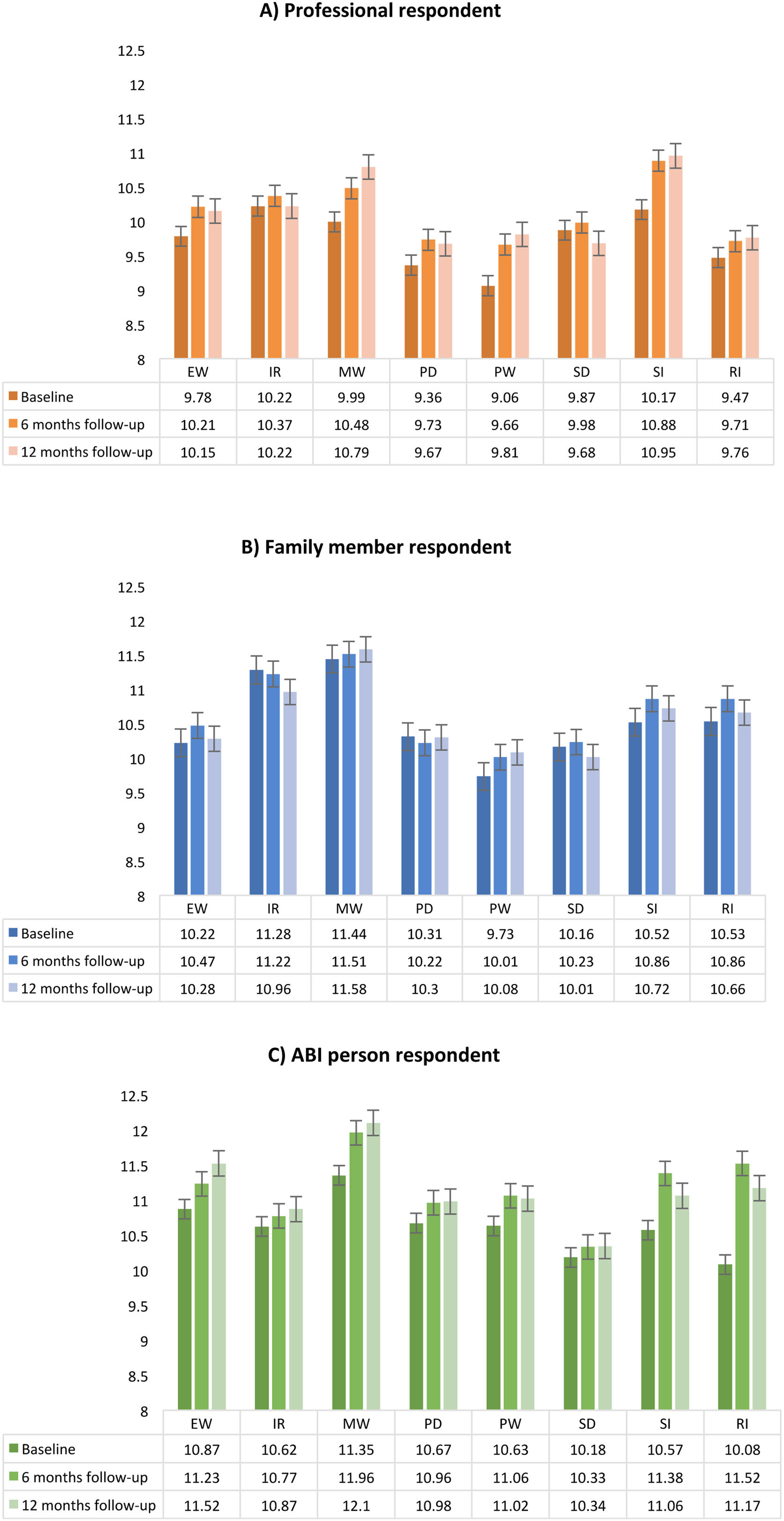
ResultsChanges in QoL during one-year follow-upThe means of the CAVIDACE scale domains for professionals, families, and patients in three evaluation periods are presented in Figure 1. Regarding the evaluations conducted by professionals, the lowest scores were found for PW in the baseline and the highest in SI at six and 12 months. In the relatives’ evaluation, the lowest scores were found again in PW at baseline, while the highest were found in MW at six and 12 months of follow-up. Finally, in the self-report, the worst-rated domain was RI at baseline, and the most positive results were found in MW at six and 12 months.
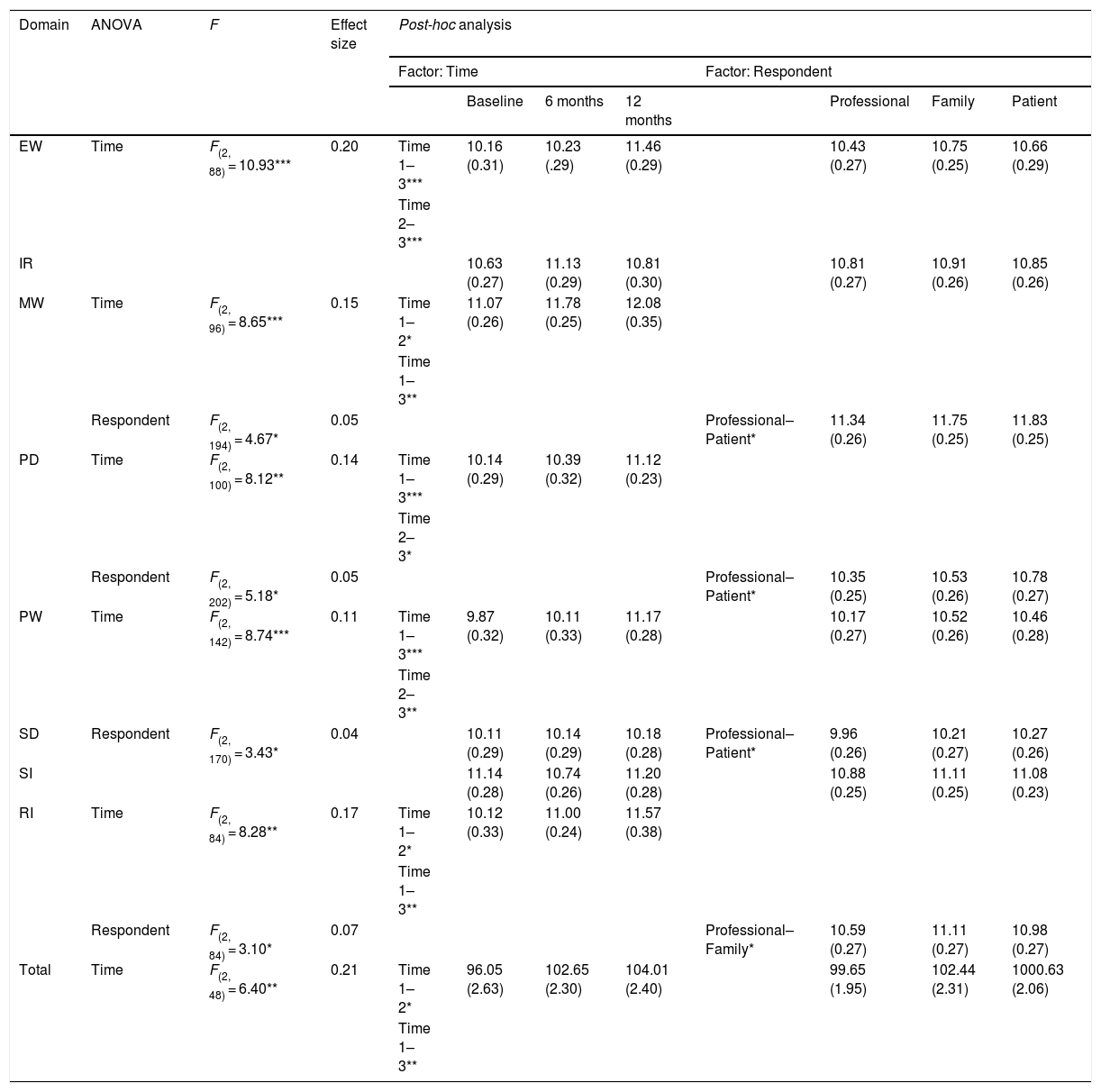
Repeated-measures ANOVA revealed statistically significant results for the factor time in five domains and in four domains for the factor respondent. No significant results were found in the interaction Time x Respondent. In the post-hoc analyses of the time’s main effect, we observed significant differences between baseline and 12 months follow-up in EW, MW, PD, PW, and RI. We also found significant differences between baseline and six months of follow-up in MW and RI, and between both follow-ups in EW, PD and PW. As shown in Table 2, an improvement in QoL was experienced over time in all cases. On the other hand, in the factor respondent, we found significant differences between professional and ABI patient in almost all significative cases (MW, PD and SD) except in the RI domain, where the differences were between the proxy reports. In the first case, it was the patients who always obtained better scores and in the case of the RI domain, it was the families.
ANOVA analysis within-subjects 3 × 3 (Time x Respondent) for QoL domains and total score.
| Domain | ANOVA | F | Effect size | Post-hoc analysis | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Factor: Time | Factor: Respondent | ||||||||||
| Baseline | 6 months | 12 months | Professional | Family | Patient | ||||||
| EW | Time | F(2, 88) = 10.93*** | 0.20 | Time 1–3*** | 10.16 (0.31) | 10.23 (.29) | 11.46 (0.29) | 10.43 (0.27) | 10.75 (0.25) | 10.66 (0.29) | |
| Time 2–3*** | |||||||||||
| IR | 10.63 (0.27) | 11.13 (0.29) | 10.81 (0.30) | 10.81 (0.27) | 10.91 (0.26) | 10.85 (0.26) | |||||
| MW | Time | F(2, 96) = 8.65*** | 0.15 | Time 1–2* | 11.07 (0.26) | 11.78 (0.25) | 12.08 (0.35) | ||||
| Time 1–3** | |||||||||||
| Respondent | F(2, 194) = 4.67* | 0.05 | Professional–Patient* | 11.34 (0.26) | 11.75 (0.25) | 11.83 (0.25) | |||||
| PD | Time | F(2, 100) = 8.12** | 0.14 | Time 1–3*** | 10.14 (0.29) | 10.39 (0.32) | 11.12 (0.23) | ||||
| Time 2–3* | |||||||||||
| Respondent | F(2, 202) = 5.18* | 0.05 | Professional–Patient* | 10.35 (0.25) | 10.53 (0.26) | 10.78 (0.27) | |||||
| PW | Time | F(2, 142) = 8.74*** | 0.11 | Time 1–3*** | 9.87 (0.32) | 10.11 (0.33) | 11.17 (0.28) | 10.17 (0.27) | 10.52 (0.26) | 10.46 (0.28) | |
| Time 2–3** | |||||||||||
| SD | Respondent | F(2, 170) = 3.43* | 0.04 | 10.11 (0.29) | 10.14 (0.29) | 10.18 (0.28) | Professional–Patient* | 9.96 (0.26) | 10.21 (0.27) | 10.27 (0.26) | |
| SI | 11.14 (0.28) | 10.74 (0.26) | 11.20 (0.28) | 10.88 (0.25) | 11.11 (0.25) | 11.08 (0.23) | |||||
| RI | Time | F(2, 84) = 8.28** | 0.17 | Time 1–2* | 10.12 (0.33) | 11.00 (0.24) | 11.57 (0.38) | ||||
| Time 1–3** | |||||||||||
| Respondent | F(2, 84) = 3.10* | 0.07 | Professional–Family* | 10.59 (0.27) | 11.11 (0.27) | 10.98 (0.27) | |||||
| Total | Time | F(2, 48) = 6.40** | 0.21 | Time 1–2* | 96.05 (2.63) | 102.65 (2.30) | 104.01 (2.40) | 99.65 (1.95) | 102.44 (2.31) | 1000.63 (2.06) | |
| Time 1–3** | |||||||||||
Note. Data are presented as means and standard deviation. EW = emotional well-being; IR = interpersonal relationships; MW = material well-being; PD = personal development; PW = physical well-being; SD = self-determination; SI = social inclusion; RI = rights. *p < .05, **p < .01, ***p < .001.
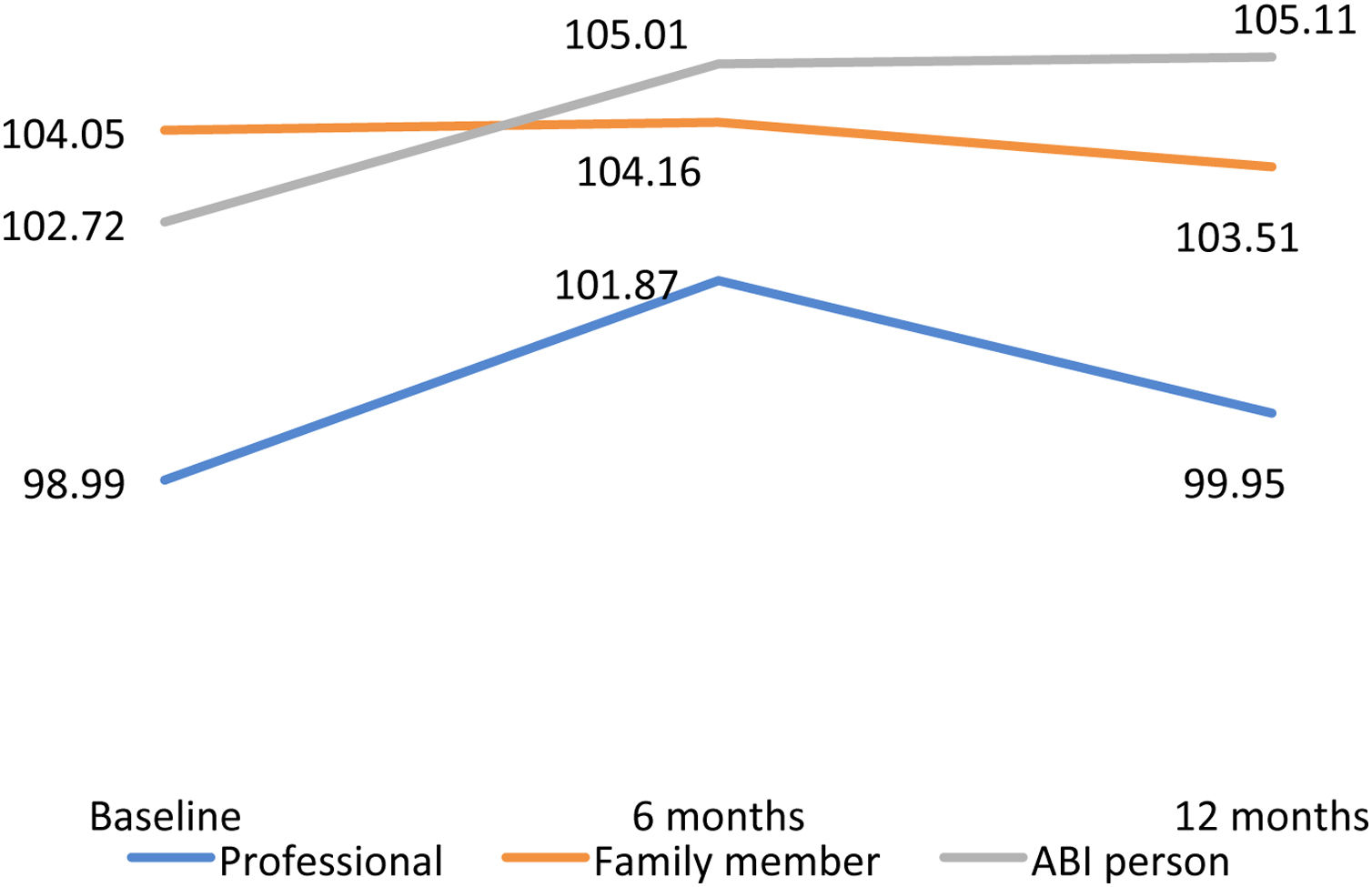
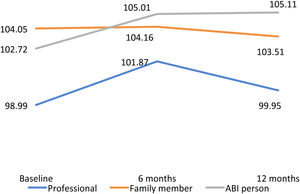
For the total QoL index, the lowest score was found in the professional evaluation at baseline (M = 98.99, SD = 15.09) and 12 months of follow-up (M = 99.95, SD = 15.77) and the best results in the self-report evaluation at six (M = 105.01, SD = 15.51) and 12 months (M = 105.11, SD = 15.51). ANOVA analysis revealed significant main effect in time for the total scores between baseline with six and 12 months of follow-up (Figure 2).
Patterns of change in QoL according to time since injuryFinally, ANOVAs reported a main significant simple effect in the group factor (recent or chronic ABI) for all the domains (except EW and MW) and QOL index. As shown in the graphs included in Appendix A, the group that had ABI three years ago or less scored more positively than those who had it longer. The effect of Group x Time interaction was significant in some domains. This translated into the existence of significant differences between the three evaluations in the group of recent ABI that were not found in the chronic group. Specifically, there was a significant improvement in the evaluation carried out at six months in: EW (Mbaseline = 9.33, M6months = 11.06, p < .001), PD (Mbaseline = 10.29, M6months = 11.03, p = .039), SD (Mbaseline = 10.31, M6months = 10.92, p = .007), SI (Mbaseline = 10.64, M6months = 11.83, p = .001) and total QoL(Mbaseline = 106.61, M6months = 110.93, p = .019). These improvements were maintained at 12 months, except in SD (M12months = 10.82) and total QoL (M12months = 109.32). Table 3 summarises all the analyses. Post-hoc analyses of the main time effect were not presented as they are included in Table 2.
ANOVA analysis inter-intra 2 × 3 (Group x Time) for QoL domains and total score (professional respondent).
| Domain | ANOVA | F | Effect size | Post-hoc analysis | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ABI three years ago or less (n = 135) | ABI more than three years ago (n = 238) | |||||||||
| Baseline | 6 months | 12 months | Baseline | 6 months | 12 months | |||||
| EW | Time | F(2, 161) = 8.68*** | 0.09 | Time 1-2*** | 9.33 (0.43) | 11.06 (0.40) | 10.92 (0.45) | 9.62 (.029) | 9.58 (0.27) | 9.49 (0.31) |
| GxT | F(2, 161) = 10.06*** | 0.11 | Time 1-3*** | |||||||
| IR | Group | F(1, 162) = 13.87*** | 0.08 | 11 (0.43) | 11.44 (0.40) | 11.14 (0.40) | 9.61 (0.29) | 9.45 (0.26) | 9.52 (0.27) | |
| MW | Time | F(2, 332) = 6.56** | 0.04 | 10.51 (0.49) | 11.20 (0.46) | 11.28 (0.44) | 9.74 (0.32) | 10.10 (0.31) | 10.55 (0.29) | |
| PD | Time | F(2, 122) = 5.38** | 0.08 | Time 1-2* | 10.29 (0.53) | 11.03 (0.54) | 11.43 (0.53) | 8.97 (0.33) | 9.18 (0.34) | 9.04 (0.33) |
| Group | F(1, 123) = 9.75** | 0.07 | Time 1-3** | |||||||
| GxT | F(2, 122) = 3.71* | 0.06 | ||||||||
| PW | Group | F(1, 151) = 4.82* | 0.04 | 9.85 (0.45) | 10.79 (0.46) | 10.60 (0.42) | 9.28 (0.30) | 9.52 (0.31) | 9.46 (0.28) | |
| SD | Time | F(2, 158) = 5.13** | 0.07 | Time 1-2** | 10.31 (0.41) | 10.92 (0.41) | 10.82 (0.41) | 9.10 (0.27) | 9.24 (0.27) | 9.16 (0.27) |
| Group | F(1, 159) = 10.52** | 0.07 | ||||||||
| GxT | F(2, 158) = 2.16* | 0.03 | ||||||||
| SI | Time | F(2, 158) = 8.19*** | 0.10 | Time 1-2** | 10.64 (0.43) | 11.83 (0.44) | 11.81 (0.44) | 10.14 (0.28) | 10.26 (0.28) | 10.57 (0.28) |
| Group | F(1, 159) = 5.53* | 0.04 | Time 1-3** | |||||||
| GxT | F(2, 158) = 8.19* | 0.05 | ||||||||
| RI | Group | F(1, 165) = 9.46** | 0.06 | 10.35 (0.47) | 10.45 (0.46) | 10.82 (0.45) | 8.84 (0.47) | 10.45 (0.31) | 9.10 (0.30) | |
| Total | Time | F(2, 94) = 3.63* | 0.08 | 106.61 (2.81) | 110.93 (2.77) | 109.32 (2.71) | 96.57 (1.79) | 110.93 (2.77) | 96.23 (1.73) | |
| Group | F(1, 95) = 15.60*** | 0.14 | ||||||||
| GxT | F(2, 94) = 2.75* | 0.04 | ||||||||
Note. Data are presented as means and standard deviation. EW = emotional well-being; IR = interpersonal relationships; MW = material well-being; PD = personal development; PW = physical well-being; SD = self-determination; SI = social inclusion; RI = rights. *p < .05, **p < .01, *** p < .001.
The study presents a longitudinal analysis of the QoL during one-year follow-up in Spanish adults, who experienced ABI time ago before the inclusion in the study, using a specific instrument: the CAVIDACE scale. Likewise, it also explores the differences in QoL depending on whether a proxy- (family or professional) or a self-report evaluation is taken. Finally, it analyses how the time elapse since the ABI affects the evolution patterns of QoL. Therefore, the study contributes to the knowledge of the QoL evolution and understanding of different assessment approaches based on a multidimensional model.
In general, the results by domains showed that MW and SI had the highest values, whereas PW and SD obtained the lowest scores. These are consistent with the results obtained in other studies with ABI (Verdugo et al., 2019), and with other populations (Gómez et al., 2013). The highest outcomes could be explained based on the fact that these are people who are receiving care in specialised centres. On the other hand, the high prevalence of comorbidities and the poor ability to perform basic daily living activities independently (Zhang et al., 2013), as well as limitations in personal autonomy and problem solving, may explain the negative results. In any case, discrepancies should be carefully analysed depending on the respondent and the time evaluation. For example, in the proxy evaluators the lowest scores are obtained in PW in the first evaluations (baseline and six months follow-up) but in the last one it is in SD domain. This occurs because PW experiences an improvement that does not happen for SD. On the other hand also, regardless the time of evaluation, relatives and ABIs reported higher levels of MW. However, professionals reported IR and SI as more positively. It is possible that there is a social desirability effect with the MW together with an observational bias on the part of the professionals who can observe the person with ABI in a context in which they interact and relate within the community.
QoL levels experienced improvement at six months (Hu et al., 2012), regardless of the respondent. If we consider the 12-month time period, late improvements were also found in some QoL domains and total QoL score (Chiang et al., 2015; Lin et al., 2010; Yeoh et al., 2019). In line with the few studies on the subject, it has been found that social domains (Lin et al., 2010; Pucciarelli et al., 2019), such as IR or SI, do not experience a significative improvement. There were also other domains in which no significant changes were experienced, such as SD. It could be because the return to an independent and active working life do not usually occur, even in the long term, in this population. However, significant improvements were experienced in EW (Hu et al., 2012) that were not found in other studies (Chiang et al., 2015). We must note that our sample was receiving psychological and neuropsychological attention in most cases, and that the EW domain on the CAVIDACE Scale differs from other scales that refer to cognitive abilities that experience less change. In this sense, depression and anxiety could improve over time (Lam et al., 2019). Finally, although there were some cases in which a significant late improvement occurred between the assessments at 6 and 12 months (EW, PD and PW), in most cases, there were substantially smaller improvements than those experienced between baseline and six months; even, in many cases, we found lower levels of QoL at 12 months than at six months. This pattern of QoL evolution has been reported in previous studies (Hu et al., 2012; van-Mierlo et al., 2017), showing the importance of timeframe for functional recovery.
The lack of interaction between the time- and the respondent factor shows that these patterns of change between the different evaluations do not depend on the respondent employed (proxy or self-report), which supposes an argument in favour of the existence of agreement between evaluators. However, there was a pattern of greater stability when it was the relative who responded. Total QoL and domain scores were higher when self-reported data were analysed as compared to professional- or family-reported data. This finding concurs with those of other studies that have assessed the QoL of individuals with ABI (Hilari et al., 2007; Kozlowski et al., 2015) and it may occur due to issues such as the high presence of anosognosia in the ABI population (Formisano et al., 2017). In this sense, professionals always obtained lower scores than the other two groups. It seems that professional used stricter criteria when they assessed the QoL of individuals with ABI. One possible explanation could be their in-depth knowledge of all the deficits of the affected individuals. The significant differences between respondents have been found in those areas that have been least traditionally studied within the concept of QoL, such as MW, PD, SD, and RI, and which also coincide with those that may be less observable through external indicators (Hwang et al., 2017; Kozlowski et al., 2015). For EW that calls attention to the existence of agreement between the respondents (Câmara-Costa et al., 2020). The lack of concordance between proxy- and self-report QoL instruments led us to consider the use of one or another based on the goal of assessment (Verdugo et al., 2005): self-reports are used for developing person-centred programmes, while proxies are for programme evaluation, improvement of quality of services and evaluation of organisational services (Verdugo et al., 2013).
Numerous investigations have shown that QoL improves in the first months or years after ABI to remain at more stable levels subsequently (Andelic et al., 2018; Grauwmeijer et al., 2018). Since in our study a part of the sample had a recent ABI (three years ago or less) and the other a chronic ABI condition, it was analysed how this affected the longitudinal changes experienced. This analysis was performed only with the sample of professionals, since including all respondents would have exceeded the limits of this paper. On the one hand, it was found that people who had the ABI for a shorter amount of time had higher QoL. Previous studies have reported negative correlations between QoL and time since injury (Tomberg et al., 2007). It may be that factors such as age (Haller et al., 2017; Hu et al., 2012), limited possibilities of rehabilitation in the chronic phase and underdeveloped community-based social support (Tomberg et al., 2007) could mediate these results. On the other hand, time elapsed since ABI was found to interact significantly in most domains and overall score with QoL evolution patterns, showing significant improvements in the group with the most recent ABI not found in the chronic group. As expected, these changes were especially significant in the period between baseline and six months, stressing the importance of early changes.
This study has limitations. First, there was a substantial loss of subjects throughout follow-up evaluations. However, it was found that there were hardly any differences between the sample with complete follow-ups and the sample “loss”. Second, as we used convenience and snowball sampling to recruit participating centres, the personal biases of professionals may affect the process, although each centre was instructed to select random participants. This procedure limits the generalisability of the findings. However, while most studies have focused only on TBI or stroke, our sample was composed of all ABI aetiologies, providing a broader view of the condition. Third, as with all longitudinal studies, knowledge of the instruments may affect the responses given.
Despite its limitations, the present study provides important information for scientific development and professional clinical practice with ABI population. This emphasizes that the initial time after ABI and the first phases of care (even in the chronic phase), are vital for the improvements obtained in QoL. This implies the need for intensive interventions at this time as well as the revision of the interventions objectives that are carried out during later phases. On the other hand, it is important to review and improve the interventions that are made with the domains related to interpersonal relationships, inclusion in the community or the self-determination and productivity of this population. Future research should focus on assessing QoL since the occurrence of ABI by using longer than one-year follow-up periods to being able to appreciate later changes. Equally interesting would be to use estimators of the QoL levels before ABI and to study predictive factors of QoL change to be able to intervene in them.
Funding and acknowledgmentsWe gratefully acknowledge the funding and support of the Spanish Ministry of Economy and Competitiveness (Grant PSI2015-65193-P [MINECO/FEDER, UE]) and the fellowship provided to Alba Aza Hernández (BES-2016-078252) of the Spanish Ministry of Economy and Competitiveness. We would also like to thank the people with brain injury, their family, the professionals and the organizations for completing the questionnaires and for their support on this project.