Mental health problems are common among adolescents and greatly influenced by stressful events. This study sought to assess the prevalence and correlates of insomnia, depressive and anxiety symptoms among Chinese adolescents during the COVID-19. Method: Cross-sectional study (N = 1,794 adolescents, mean age = 15.26) was conducted in May 2020. An online survey was used to collect socio-demographic data, COVID-related fear (COVID-fear), nutrition, physical activity (PA) level and the symptoms of insomnia, depression and anxiety. Results: The prevalence of insomnia, depressive and anxiety symptoms was 37.80%, 48.20% and 36.70%, respectively, among Chinese adolescents during the pandemic. Generalized linear models revealed that female, left behind children, and students with greater COVID-fear tended to report symptoms of insomnia, depression and anxiety concurrently. After adjusting for socio-demographic factors and COVID-fear, better nutritional status and moderately active PA were both associated with lower levels of depressive and anxiety symptoms, while highly active PA was associated with lower levels of insomnia, depressive and anxiety symptoms. Conclusions: These findings suggest that more attention should be paid to psychological health among adolescents while combating COVID-19. To promote adolescents’ mental health, educators should help adolescents develop a healthy lifestyle with balanced diet and regular exercise.
Los problemas de salud mental son comunes en adolescentes y están influenciados por eventos estresantes. Se evaluó prevalencia y correlatos de síntomas de insomnio, depresión y ansiedad en adolescentes chinos durante el COVID-19. Método: En mayo de 2020 se realizó un estudio transversal (N = 1.794 adolescentes, edad media = 15,26) mediante una encuesta en línea para recopilar datos sociodemográficos, miedo relacionado con COVID-19, nutrición, actividad física (AF) y síntomas de insomnio, depresión y ansiedad. Resultados: La prevalencia de síntomas de insomnio, depresión y ansiedad fue del 37,80%, 48,20% y 36,70%, respectivamente. Modelos lineales generalizados revelaron que mujeres, niños abandonados y estudiantes con más miedo al COVID-19 tendían a informar síntomas de insomnio, depresión y ansiedad simultaneamente. Después de ajustar los factores sociodemográficos y el miedo al COVID-19, mejor estado nutricional y AF moderadamente activa se asociaron con niveles más bajos de síntomas de depresión y ansiedad, mientras que AF muy activa se asoció con niveles más bajos de insomnio, síntomas depresivos y de ansiedad. Conclusiones: Se debe prestar más atención a la salud psicológica de los adolescentes mientras se combate el COVID-19. Para promover su salud mental, los educadores deben ayudarles a desarrollar un estilo de vida saludable con una dieta equilibrada y ejercicio regular.
Since the outbreak of the 2019 novel coronavirus disease (COVID-19), over 47 million infected cases (including more than 1 million deaths) were reported globally as of November 6, 2020 (World Health Organization, 2020). To prevent the transmission of the COVID-19, protective/distancing measures (e.g., social isolation and quarantining) have been implemented in many nations and regions - such dramatic lifestyle changes potentially affect the well-being of different age groups (Brailovskaia & Margraf, 2020). Compared with a global prevalence estimate (3.44%) of depression in 2017, pooled prevalence from a recent meta-analysis conducted during the COVID-19 was 7 times higher (25%), which to a certain extent reflects a significant impact of the COVID-19 outbreak on mental health (Bueno-Notivol et al., 2021). Besides, the increased rates of mental problems were consistently reported to be prevalent among adolescents (Lei et al., 2020; Wang et al., 2020). It may be attributed to a transitional stage of physical and psychological development at which this age group is more sensitive to this life-threatening event, for example, unprecedented shift from on-site teaching to virtual classroom (Shen et al., 2020). Recent research has showed that the prevalence of insomnia, depressive and anxiety symptoms among Chinese middle school students was 21.90%, 43.70% and 37.40%, respectively, during the COVID-19 period (Zhou, Wang et al., 2020; Zhou, Zhang et al., 2020). Notably, insomnia is not simply associated with impaired daytime functioning, but also linked to emotional and behavioral problems (Zhao et al., 2019). In addition, adolescent depression and anxiety, as the most commonly reported negative emotions, can impair their academic and social functioning (Jaycox et al., 2009; Van Ameringen et al., 2003). Besides, most mental health issues usually start in adolescence and is key to address early in order to prevent the development of more severe psychiatric disorders in adulthood (Jones, 2013). Against this background, assessing the prevalence of these symptoms and identifying the protective/risk factors for mental health of adolescents during the COVID-19 is urgently needed.
Accumulating evidence has indicated that modifiable lifestyle factors, such as nutrition and physical activity (PA), are closely linked to mental health (Biddle et al., 2019; Cook et al., 2020). In fact, several experts have expressed concerns about nutrition and PA when it comes to psychological burden during the COVID-19 pandemic (Shen et al., 2020). It is suggested that unhealthy behaviors, such as physical inactivity was associated with poorer mental health during the COVID-19 pandemic (Werneck et al., 2020). Conversely, healthy behaviors during COVID-19 like healthy diet and more PA may help alleviate levels of depressive and anxiety symptoms (Fullana et al., 2020; Nguyen et al., 2020). Considering the fact that adolescence is a key period of physical, social, and emotional changes, nutritional status may play a crucial role in preventing mental health problems and promoting well-being among adolescents (Bühlmeier et al., 2018). Specifically, a recent research found that healthier diet patterns may promote better sleep quality among adolescents (Jansen et al., 2020). Additionally, data from the Global School-based Student Health Survey with 65,267 adolescents indicated that a healthy diet pattern with regular fruit intake was significantly associated with both lower risks of depressive and anxiety symptoms (Liu et al., 2020). Many researchers have indicated that different PA levels produce different degrees of health benefits. For example, a high level of PA was a protective factor for insomnia among a nationally representative sample of adolescents (Werneck et al., 2018). Furthermore, a recent research (including nearly 3,000 participants) found that both highly active and moderately active groups were significantly correlated with psychological well-being (Maugeri et al., 2020), indicating that mental health benefits are only attained if a certain PA level was achieved.
Since both nutrition and PA are essential components of adolescents’ lifestyle, studying their roles concurrently in a given adolescent population can inform health professionals and school administers to develop more effective interventions for preventing mental illnesses under such major public crisis like COVID-19. Notably, previous studies on this topic mainly focused on the impact of one lifestyle behavior (nutrient or PA) on one psychologically related outcome (e.g., insomnia, depressive, and/or anxiety symptoms). Besides, the relationship between the two lifestyle behaviors (nutrition and PA) with mental health have not yet been verified among Chinese adolescents during the pandemic. Therefore, for a better understanding of this topic, the main objective of this study was to investigate association of two critical lifestyle behaviors (nutrition or PA) with insomnia, depressive, or anxiety symptoms among Chinese adolescents during the COVID-19.
Despite lifestyle behaviors have profound impacts on the mental health of adolescents, some socio-demographic factors are also closely linked with psychological outcomes (Zhou, Zhang et al., 2020). According to the ecological risk/protection theory, personal (e.g., gender and grade) and family factors (e.g., family socioeconomic status; SES) may either promote or hinder the process of adolescent development (Bogenschneider, 1996). For example, it was found that female gender was a risk factor for depressive and anxiety symptoms (Zhou, Zhang et al., 2020). Besides, a systematic review found that adolescents with low SES was more likely to develop mental problems than counterparts with better SES (Reiss, 2013). Moreover, fear of COVID-19 (COVID-fear; e.g., fear of being infected) may increase the risk of developing mental illnesses (Ahorsu, Lin et al., 2020), which is supported by a recent study indicating that excessive COVID-fear caused anxiety, insomnia, and even suicide (Dsouza et al., 2020). Therefore, for future timely prevention and effective intervention, we attempted to analyze associations of the aforementioned factors (i.e., age, gender, grade, residence, left behind status, only child status, SES, and COVID-fear) with insomnia, depressive and anxiety symptoms.
Collectively, we conducted the present study with three specific aims: (1) to explore prevalence of insomnia, depressive and anxiety symptoms among Chinese adolescents during the COVID-19 outbreak; (2) to investigate associations of socio-demographic factors and COVID-fear with insomnia, depressive and anxiety symptoms; (3) to investigate associations of nutrition and PA with insomnia, depressive and anxiety symptoms after adjusting socio-demographic factors and COVID-fear.
MethodParticipants and procedureThis study was conducted between May 13 and 20, 2020, shortly after reopening schools in Hechi city, Guangxi province, China. During the study period, there were 1,772,000 students within more than 160 public junior high schools located in Hechi (Hechi Education Bureau, 2019). Of these public schools, thirteen were randomly recruited into the survey and completed the questionnaire, with 8,939 students providing data. To meet the age requirement of questionnaires for measuring PA, only participants who turned 15 and above were included in this study. In total, 1,856 students met the criterion. After the exclusion of 62 individuals with missing or incomplete responses, data of 1,794 students were retained for final analyses (96.70%).
Graduate students in Psychology conducted this survey with the assistance of mental health counselors from the local middle schools. Prior to data collection, the purpose of this study was explained to all participants, followed by obtaining their informed consents. All participants completed the questionnaires via an online survey platform in which instructions on how to fill out the survey were described. The questionnaires contained information on sociodemographic characteristics, COVID-fear, nutrition, PA, insomnia, depressive and anxiety symptoms. The study protocol was approved by the Human Research Ethics Committee of University (Code number: 2020005).
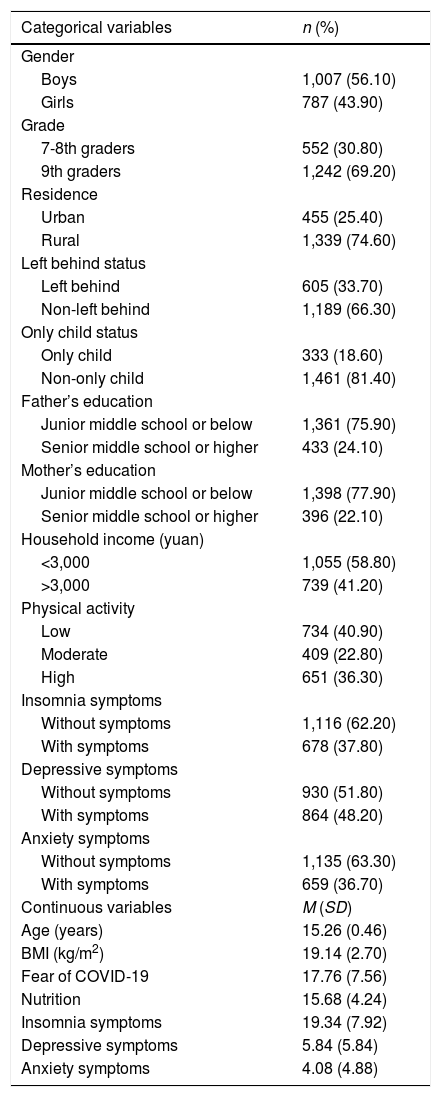
This study included 1,794 students aged 15 and 18 years (mean age: 15.26 ± 0.47). Males comprised 56.20% and females comprised 43.80% of the sample. Of all participants, 37.80% were reported with insomnia symptoms, 48.2% with depressive symptoms, and 36.70% with anxiety symptoms. More detailed information of the participants is presented in Table 1.
Participants’ characteristics.
| Categorical variables | n (%) |
|---|---|
| Gender | |
| Boys | 1,007 (56.10) |
| Girls | 787 (43.90) |
| Grade | |
| 7-8th graders | 552 (30.80) |
| 9th graders | 1,242 (69.20) |
| Residence | |
| Urban | 455 (25.40) |
| Rural | 1,339 (74.60) |
| Left behind status | |
| Left behind | 605 (33.70) |
| Non-left behind | 1,189 (66.30) |
| Only child status | |
| Only child | 333 (18.60) |
| Non-only child | 1,461 (81.40) |
| Father’s education | |
| Junior middle school or below | 1,361 (75.90) |
| Senior middle school or higher | 433 (24.10) |
| Mother’s education | |
| Junior middle school or below | 1,398 (77.90) |
| Senior middle school or higher | 396 (22.10) |
| Household income (yuan) | |
| <3,000 | 1,055 (58.80) |
| >3,000 | 739 (41.20) |
| Physical activity | |
| Low | 734 (40.90) |
| Moderate | 409 (22.80) |
| High | 651 (36.30) |
| Insomnia symptoms | |
| Without symptoms | 1,116 (62.20) |
| With symptoms | 678 (37.80) |
| Depressive symptoms | |
| Without symptoms | 930 (51.80) |
| With symptoms | 864 (48.20) |
| Anxiety symptoms | |
| Without symptoms | 1,135 (63.30) |
| With symptoms | 659 (36.70) |
| Continuous variables | M (SD) |
| Age (years) | 15.26 (0.46) |
| BMI (kg/m2) | 19.14 (2.70) |
| Fear of COVID-19 | 17.76 (7.56) |
| Nutrition | 15.68 (4.24) |
| Insomnia symptoms | 19.34 (7.92) |
| Depressive symptoms | 5.84 (5.84) |
| Anxiety symptoms | 4.08 (4.88) |
Sociodemographic factors. Information including age, gender (boy/girl), grade (7/8/9), residence (urban/rural), left behind status (left behind/non-left behind: left behind children refers to the children whose parents have been absent for at least one year since they worked in other cities) (Fan et al., 2010), and only child status (only/non-only) was collected. They were also asked to report their family SES, including parental educational (junior middle school or below/senior middle school or higher) and household monthly income per person (Chinese currency [Yuan as unit] - RMB: < 3,000/≥ 3,000).
COVID-related fear (COVID-fear). COVID-fear was measured using the Chinese version of the Fear of COVID-19 Scale (FCV-19S; Ahorsu, Lin et al., 2020; Chi et al., 2020). It consisted of 7 items, with each item that can be responded on a five-point Likert scale (strongly disagree = 1 to strongly agree = 5). Its total score (summation of individual response items) ranged from 7 to 35, with higher scores indicating greater COVID-fear level. CFA showed good model fits in this sample: χ2 = 55.42, degree of freedom (df) = 9, p < .001, comparative fir index (CFI) = .996, Tucker-Lewis index (TLI) = .991, root mean square error of approximation (RMSEA) = .054, standardized root mean squared residual (SRMR) = .008, indicating good structural validity. Cronbach’s α coefficient of .95 indicated an excellent reliability.
Nutrition. Data on nutrition were collected using the sub-scale of the Chinese version of the Health Promoting Lifestyle Profile-Ⅱ (HPLP-Ⅱ; Cao et al., 2016). Specifically, nutrition-related dimension included 6 items rated on a four-point Likert scale (1 = Never to 4 = Routinely). A total score that ranged from 6 to 24 can be obtained, with higher scores representing better nutrition. CFA indicated good structural validity, with good model fits in this sub-scale: χ2 = 42.91, df = 9, p < .001, CFI = .992, TLI = .987, RMSEA = .046, SRMR = .015. Cronbach’s α coefficient of .86 indicated a good reliability.
Physical activity. PA was assessed using the International Physical Activity Questionnaire Short Form (IPAQ-SF; Craig et al., 2003). The IPAQ-SF is considered a reliable instrument to assay the total amount of PA obtained in the 15-65 years people (Craig et al., 2003). Questions/items in the IPAQ-SF involved vigorous (i.e., heavy lifting, aerobic exercise by bicycles or treadmills), moderate (i.e., carrying light loads, bicycling at a regular pace, work out in the garden); and walking activities. Participants were required to recall the frequency and duration they were involved daily in each activity during the last 7 days. Based on the IPAQ recommendations for scoring protocol, participants were classified into three groups (lowly active, moderately active, and highly active) according to the cut-off of total metabolic equivalent task weekly (Fan et al., 2014; IPAQ group, 2002). The Chinese version of the IPAQ has been validated in a Chinese population with ICC of .79 and % CV of 26% (Macfarlane et al., 2007).
Insomnia symptoms. Insomnia was measured using the Chinese version of the Youth Self-Rating Insomnia Scales (YSIS; Buysse et al., 2006; Liu et al., 2019). The YSIS consisted of 8 items with each item that is rated on a 5-point scale. A total YSIS score that ranged from 8 to 40 can be obtained, with a higher total score indicating a greater severity of insomnia during the past month. Participants who scored 22 and above were identified as having insomnia symptoms, whereas participants with score of less than 22 had no insomnia symptoms (Liu et al., 2019). The psychometric properties of the YSIS were assessed in a large sample of Chinese adolescents (Liu et al., 2019), which is further supported by the current study. CFA indicated structural good validity, with model fits in this scale: χ2 = 280.37, df = 24, p < .001, CFI = .974, TLI = .961, RMSEA = .077, SRMR = .030. This scale was reliable, with a Cronbach’s α coefficient of .91.
Depressive symptoms. The Chinese version of the 9-item Patient Health Questionnaire (PHQ-9) was used to measure severity of depressive symptoms (Kroenke et al., 2001). A total score ranged from 0 to 27 (higher points indicating more severe depressive symptoms), with each item that can earn 0 to 3 points (0 = Not at all to 3 = Nearly every day). Total scores of 5, 10, 15, and 20 were identified as mild, moderate, moderately severe and severe depressive symptoms, respectively (Kroenke et al., 2001). Thus, a total score of 5 was set as a cut-off point to categorize participants into two groups: no depressive symptoms (PHQ-9 score <5) and depressive symptoms (PHQ-9 score ≥ 5). The Chinese version of PHQ-9 has been widely used and well validated in Chinese adolescents (Leung et al., 2020), which is further supported by the current study. CFA presented good model fits in this scale: χ2 = 364.20, df = 27, p < .001, CFI = .973, TLI = .963, RMSEA = .069, SRMR = .025, indicating good structural validity. This scale had good internal consistency, with a Cronbach’s α coefficient of .91.
Anxiety symptoms. Anxiety symptoms were measured using the Chinese version of the Generalized Anxiety Disorder scale (GAD-7; Tong et al., 2016). Each item has four response options with scores ranging from 0 to 3 (0 = Not at all to 3 = Nearly every day). Each participant can obtain a total score that ranged from 0 to 21, with higher score indicating more severe anxiety symptoms. Total scores of 5, 10, 15, and 20 were identified as mild, moderate, moderately severe and severe anxiety, respectively (Spitzer et al., 2006). Thus, with the cut-off point set at 5, participants were categorized into two groups: no anxiety symptoms (GAD-7 score <5) and anxiety symptoms (GAD-7 score ≥5). The Chinese version of GAD-7 has been widely used and well validated in multiple studies (Qing, 2013; Tong et al., 2016), which is further supported by the current study. CFA indicated good structural validity with model fits in this scale: χ2 = 124.31, df = 13, p < .001, CFI = 0988, TLI = .980, RMSEA = .069, SRMR = .016. This scale had good internal consistency, with a Cronbach’s α coefficient of .93.
Statistical analysesFirst, validity and reliability of scales used in this study were assessed. Validity was indicated by χ2, CFI, TLI, RMSEA and SRMR. Specifically, CFI or TLI with values greater than .95 indicated good fit (Hu & Bentler, 1999). RMSEA less than .07 (Steiger, 2007) and SRMR less than .08 indicated acceptable fit (Hu & Bentler, 1999). Cronbach’s α coefficients for each scale were calculated to present internal reliability. Second, descriptive analyses were performed for participant characteristics. Next, correlation analysis was used to preliminarily analyze the relationships between sociodemographic factors (i.e., age, gender, grade, residence, left behind status, only child status, SES), COVID-fear, nutrition and PA with the symptoms of insomnia, depression and anxiety. Then for further analysis, generalized linear models were performed with insomnia, depressive and anxiety symptoms as dependent variables, while factors significantly correlated to one or more symptoms were included as independent variables. Statistical analyses above were performed using SPSS version 26 and Mplus version 8. In the interpretation of the results, the statistical significance was set at p < .05 (two-tailed).
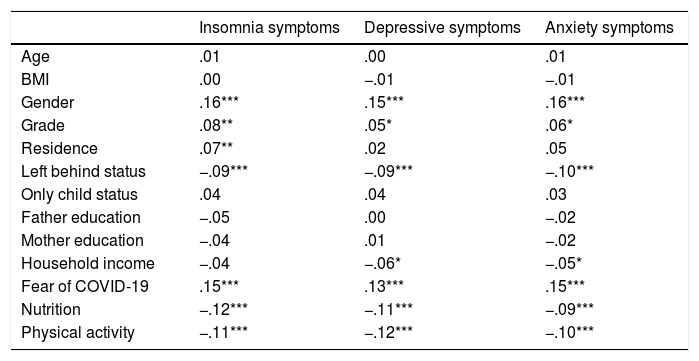
ResultsResults on correlations between variables in this study are presented in Table 2. Specifically, females, 9th graders and left behind children and students with more COVID-fear was significantly associated with higher level of insomnia, depressive and anxiety symptoms. However, both better nutrition and higher PA level were significantly correlated with lower level of the three symptoms. Specific correlation coefficients and significance can be obtained in Table 2.
Correlations between variables interested in this study.
| Insomnia symptoms | Depressive symptoms | Anxiety symptoms | |
|---|---|---|---|
| Age | .01 | .00 | .01 |
| BMI | .00 | −.01 | −.01 |
| Gender | .16*** | .15*** | .16*** |
| Grade | .08** | .05* | .06* |
| Residence | .07** | .02 | .05 |
| Left behind status | −.09*** | −.09*** | −.10*** |
| Only child status | .04 | .04 | .03 |
| Father education | −.05 | .00 | −.02 |
| Mother education | −.04 | .01 | −.02 |
| Household income | −.04 | −.06* | −.05* |
| Fear of COVID-19 | .15*** | .13*** | .15*** |
| Nutrition | −.12*** | −.11*** | −.09*** |
| Physical activity | −.11*** | −.12*** | −.10*** |
Note. * p < .05, ** p < .01, *** p < .001.
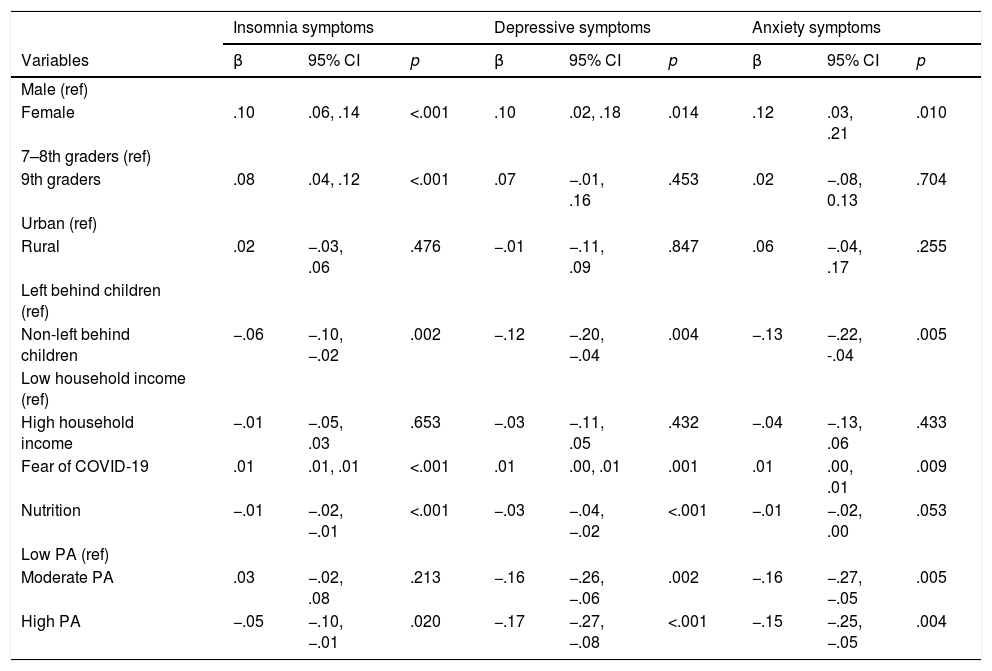
As shown in Table 3, eight variables significantly correlated with one or more symptoms (i.e., gender, grade, residence, left behind status, household income, COVID-fear, nutrition and PA) were included in the generalized linear models. Females, left behind children and students with more COVID-fear were more likely to develop insomnia symptoms (females: β = .10 [.06, .14], p < .001; non-left behind: β = −.06 [−.10, −.02], p = .002; more COVID-fear: β = .01 [.01, .01], p < .001), depressive symptoms (females: β = .10 [.02, .18], p = .014; non-left behind: β = −.06 [−.10, −.02], p = .002; more COVID-fear: β = .01 [.00, .01], p = .001) and anxiety symptoms (females: β = .012 [.03, .21], p = .010; non-left behind: β = −.13 [−.22, −.04], p = .005; more COVID-fear: β = .01 [.00, .01], p = .009) concurrently. Regarding the two lifestyle behaviors concerned in this study, better nutrition was associated with lower level of insomnia symptoms (β = −.01 [−.02,−.01], p < .001) and depressive symptoms (β = −.03 [−.04, −.02], p < .001); with lowly active physically as the referent, moderately active physically was significantly associated with lower level of depressive symptoms (β = −.16 [−.26, −.06], p = .002) and anxiety symptoms (β = −.16 [−.27, −.05], p = .005), while highly active physically was associated with lower level of insomnia symptoms (β = −.05 [−.10, −.01], p = .020), depressive symptoms (β = −.17 [−.27, −.08], p < .001) and anxiety symptoms (β = −.15 [−.25, −.05], p = .004).
Associations between gender, grade, residence, left behind status, household income, COVID-19 related fear, nutrition and physical activity with insomnia, depressive and anxiety symptoms.
| Insomnia symptoms | Depressive symptoms | Anxiety symptoms | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | β | 95% CI | p | β | 95% CI | p | β | 95% CI | p |
| Male (ref) | |||||||||
| Female | .10 | .06, .14 | <.001 | .10 | .02, .18 | .014 | .12 | .03, .21 | .010 |
| 7–8th graders (ref) | |||||||||
| 9th graders | .08 | .04, .12 | <.001 | .07 | −.01, .16 | .453 | .02 | −.08, 0.13 | .704 |
| Urban (ref) | |||||||||
| Rural | .02 | −.03, .06 | .476 | −.01 | −.11, .09 | .847 | .06 | −.04, .17 | .255 |
| Left behind children (ref) | |||||||||
| Non-left behind children | −.06 | −.10, −.02 | .002 | −.12 | −.20, −.04 | .004 | −.13 | −.22, -.04 | .005 |
| Low household income (ref) | |||||||||
| High household income | −.01 | −.05, .03 | .653 | −.03 | −.11, .05 | .432 | −.04 | −.13, .06 | .433 |
| Fear of COVID-19 | .01 | .01, .01 | <.001 | .01 | .00, .01 | .001 | .01 | .00, .01 | .009 |
| Nutrition | −.01 | −.02, −.01 | <.001 | −.03 | −.04, −.02 | <.001 | −.01 | −.02, .00 | .053 |
| Low PA (ref) | |||||||||
| Moderate PA | .03 | −.02, .08 | .213 | −.16 | −.26, −.06 | .002 | −.16 | −.27, −.05 | .005 |
| High PA | −.05 | −.10, −.01 | .020 | −.17 | −.27, −.08 | <.001 | −.15 | −.25, −.05 | .004 |
Using data from a large sample of Chinese adolescents collected during the COVID-19, this study aimed to determine correlates of insomnia, depressive and anxiety symptoms. Results showed that prevalence of these above-mentioned symptoms was high in our sample with being more prevalent among female participants, left behind children and students with higher COVID-fear. Both better nutritional status, moderately and highly active (PA) levels were protective factors for depression and anxiety, while highly active (PA) level was significantly associated with lower level of insomnia symptoms. Possible explanation for these results will be discussed below.
Prevalence of insomnia, depressive and anxiety symptoms in this study are similar to results from two previous large-scale epidemiological studies (conducted in March 2020) on Chinese adolescents (the peak period of COVID-19 in China) (Zhou, Wang, et al., 2020; Zhou, Zhang, et al., 2020). Due to the COVID-19 outbreak, schools in China have been locked down at all levels indefinitely. Although educational authorities have developed online portals and applications to deliver lectures or other teaching activities, the uncertainty of academic development would have adverse impact on students’ psychological health. Besides, students were required to report their daily health conditions and comply with strict prevention measures of the COVID-19, which may lead to psychological distress. The high prevalence of mental problems is a warning that we should not ignore, particularly among adolescents despite that COVID-19 situation has been better. In fact, recent studies have found that negative impact of the pandemic on mental health, may be continuous and long-term (Gan et al., 2020; Sher, 2020). Collectively, results in this stuy have informed stakeholders (policy makers, educators and psychologists) to provide timely and effective interventions for mental health benefits.
Consistent with pre-COVID-19 studies (Mallampalli & Carter, 2014; Salk et al., 2017), the present study shows that female participants were reported with higher level of insomnia, depressive and anxiety symptoms than their male counterpart. Previous studies have noted that females appear to be more vulnerable to insomnia, depressive and anxiety symptoms compared with males (Suh et al., 2018; Van Eycken et al., 2020). The gender differences in these symptoms may be be driven by a complicated interplay of biological, physiological and social factors that play differential roles throughout the life span (Suh et al., 2018). Such symptomatic variation in this study are thought to emerge in adolescence with the onset of menstruation in girls (Mallampalli & Carter, 2014). Moreover, gender differences may be related to social desirability: Girls are expected to be more emotionally sensitive, experiencie more body dissatisfaction and ruminate more as a coping strategy, which all have been associated with a greater likelihood of mental health problems (Martínez-Hernáez et al., 2016; Van Droogenbroeck et al., 2018).
Additionally, left behind children showed greater levels of insomnia, depressive and anxiety symptoms, indicating the negative impact of parental absence on mental health of Chinese left behind adolescents. The attachment theory has a great emphasis on the enduring bond of children to their parents - these ties are crucial for physical and emotional adaptation (Allen et al., 1998). Unfortunately, left behind children experience separation from an attachment figure, ongoing parent-child interactions to fortify their bonds become inhibited, which results in stressful situations that fuel sleep and mental health problems. Indeed, a previous study with a large sample of Chinese left behind children found that the longer the parents are absent, the higher the frequency of insomnia symptoms in children (Tang et al., 2020). Thus, the promotion of harmonious parent-child interactions is critical to enhance children’s sleep quality and their healthy development physically and mentally.
Besides, higher COVID-fear was significantly associated with greater levels of insomnia, depression and anxiety. This result is partially supported by a pre-COVID study indicating that individuals who lived in a stressful and fearful environment were more likely to report insomnia (Perogamvros et al., 2020). A recent study conducted during the COVID-19 also suggested that COVID-fear was associated with psychological distress and life dissatisfaction (Satici et al., 2020), indicating that such life-threatening perception possibly increases the incidence of mental health problems. In this regard, it was reported that individuals with increased fear of COVID-19 have committed suicide due to their fear of being infected, even though they were not (Dsouza et al., 2020; Mamun & Griffiths, 2020). Thus, the government and health authorities should update COVID-19 information in a timely and accurate manner to stop the spread of rumors, ultimately leading to the reduced possibility of being fearful. Although significant associations between fear and these negative mental outcomes have been documented among adults (Ahorsu, Imani et al., 2020), results of the present study has filled void in such COVID-19 condition, particularly among adolescents.
Despite risk factors mentioned above, the current study indicated that adopting a healthy lifestyle is helpful to protect adolescents’ mental health. Associations of single lifestyle behavior with the symptoms of insomnia, depression and/or anxiety have been reported in the absence of a pandemic (Biddle et al., 2019; Weng et al., 2012), which is further supported by our results. Numerous studies have investigated the effects of some sleep-promoting food (Stonge et al., 2016). Thus, it is reasonable to find that good nutrition could improve insomnia symptoms, while a unhealthy pattern has been found to worsen the mental state and cognitive functioning (Weng et al., 2012; Yu et al., 2020). Studies have found that sustained adherence to healthy eating patterns, such as the Mediterranean diet, can reduce markers of inflammation in humans (Kastorini et al., 2011). Since heightened inflammation have been found to be linked to various mental health conditions, including mood disorders (Yuan et al., 2019), which might present a pathway through which good nutrition could decrease the risk of depressive symptoms. Although the influence of diet and food components on mental health has been gaining special attention in recent years, the potential mechanisms regarding the relationship between nutritional habits and mental health has been unexplored (Moreno-Campuzano et al., 2020), which requires further investigation.
With regard to PA, both moderately and highly active (PA) levels are associated with lower level of depressive and anxiety symptoms in this study. Numerous reviews have demonstrated the positive impact of PA on adolescent mental health, with some hypothesized mechanisms related to neurobiological, psychosocial or behavioral factors (Lubans et al., 2016). The neurobiological mechanism hypothesis proposes that PA enhances mental health via changes in the structural and functional composition of the brain (Lin & Kuo, 2013). The psycholosocial mechanism hypothesis recognizes that physical activity provides an opportunity for social interaction, self-efficacy and perceived competence and improvements in body image (Doré et al., 2020). The behavioral mechanism hypothesis proposes that PA may improve self-regulation and coping skills which, in turn, helps adolescents effectively stay positive mentally (Lubans et al., 2016). Besides, question about the differential effects of PA intensity/level on mental health (Ayala et al., 2020; Kandola et al., 2020) is answered by results of the current study indicating that only the highly active group reported significantly lower level of insomnia symptoms as compared to the lowly active group. It may be that vigorous PA would consume much more individual energy stores than moderate and low PA, so it may increase the need for sleep at night in order to reduce metabolic requirements for energy conservation and/or body restoration (Driver & Taylor, 2000; Zou et al., 2018). Given the positive impact of good nutrition and moderately and highly active (PA) levels, it is expected that the combinations of better nutrition and active PA would lead to greater benefits in mental health than promoting one healthy lifestyle behavior alone during the COVID pandemic.
Some limitations in our study should be mentioned. First, the study involved only junior middle school students. Therefore, one should be cautious in generalizing our findings to Chinese adolescents. Second, exclusionary criteria was not listed (e.g., participants with diabetes, cardiovascular, neuropsychiatric disease), which may cause bias in our results. Third, the cross-sectional design precludes making causal inferences and no comparable pre-COVID-19 data were available within this study. Thus, longitudinal and retrospective study are encouraged. Forth, the self-reported information may cause bias due to the social desirability effect and memory error. Thus, there is a need for better-designed studies with lager sample size and objective measure to provide more valuable information. Fifth, although the presence of mental problems was assessed by standardized questionnaires, these measures are not equivalent to clinical diagnoses, thus future studies with diagnostic interviews should be used. Lastly, we did not measure our participants about their degree of trauma in the outbreak, such as whether any their family members lost their jobs or even lives due to the COVID-19, which might influence mental status.
Despite these limitations, our findings have clinical and policy implications. First of all, psychology counselors in school should pay attention to the assessment of students’ mental problems, communicating with their parents in a timely manner so as to implement effective intervention. In addition, health authorities and educators need to identify high-risk groups to carry out early psychological intervention. Moreover, more attention should be given to the female students, left behind children and students with greater level in COVID-fear. More importantly, healthy lifestyle behaviors (healthy diet and physically active) should be promoted as an important preventive strategy to maintain their mental health.
FundingThis work was supported by the National Social Science Foundation of China [grant number 16CSH049]; National Natural Science Foundation of China [grant number 31871115]; Key Research Projects of Colleges and Universities in Guangdong Province [grant number 2018WZXDM015]; and Shenzhen Basic Research Grant [grant number 2019SHIBS0003].